2. Health care needs and organisation of primary health care in Brazil
The expansion of PHC in Brazil has been remarkable, contributing to significant improvements in many measures of population health over the past decades. SUS prioritisation on PHC permitted to offer services free of charge to the Brazilian population, allowing an easier contact with the health system at the community level through the development of modern multi-disciplinary family health teams. But gains have not been equal across the country, with North and Northeast regions faring worse than South and Southeast regions in terms of health improvements and health outcomes. There has also been a rise in the number of elderly patients and an increasing prevalence of risk factors for health and chronic non-communicable diseases. Tackling these challenges call for more effective PHC, responsive to people’s changing needs, capable of offering preventive, continuous and co-ordinated care.
Brazil is a high-middle income country, with a population of 212 million inhabitants in 2020. The country is divided into 26 states and one federal district, with 5 570 municipalities. The states are further organised into five geopolitical regions: North, Northeast, Centre-West, Southeast and South. Health is a universal right for the whole population and a state responsibility since the approval of the new Brazilian constitution in 1988, which established the Unified Health System (Sistema Único de Saúde, SUS) in 1990. The management and financing of SUS is shared between the Federal Ministry of Health, state departments and municipal health departments. In the decentralised health care system, municipalities have the freedom to organise PHC family health teams according to the population needs and geographic characteristics.
Brazil has made investments in PHC a priority to address disparities in access to care and improve health outcomes. The Family Health Strategy, one of the largest community-based PHC programme worldwide, launched in 1994 was successful to increase population coverage and improve health outcomes. The expansion of the Family Health Strategy has contributed to measurable improvements in terms of infant mortality rates, maternal health, immunisation uptake and avoidable hospitalisation. However, PHC in Brazil faces a number of challenges resulting from its vast territory and complex geography, which have made difficult to meet the needs of population living in vulnerable and remote communities. The expansion of PHC has been marked by stark disparities across the states and municipalities, linked mainly to workforce shortages and imbalances in the distribution of medical doctors. There has also been a rise in the number of elderly patients and an increasing prevalence of chronic non-communicable diseases, which call for effective prevention and stronger PHC to better manage the burden of chronic conditions.
This chapter describes the PHC system in Brazil. It starts by analysing the socio-economic context in which the system operates, as well as describing the governance of the PHC sector. The chapter then examines the health care needs of the Brazilian population, and lastly presents the organisation of the PHC sector.
Brazil’s government is divided into 26 states and the federal district, and 5 570 municipalities. The states and the federal district are also grouped into five regions: North, Northeast, Central-West, Southeast and South, which are used mainly for statistical purposes and to define the distribution of federal funds. Municipalities are granted the status of federal entities, at the same level as the states. While there is great heterogeneity in the geographical area and population, as well as social and economic indicators, among the subnational jurisdictions, all Brazilian municipalities enjoy the same legal status (OECD/UCLG, 2019[1]). In 2015, 17 municipalities had more than 1 million inhabitants (22% of population). About 44% of municipalities had less than 10 000 inhabitants. Brazil also has 438 health regions, which are made up of municipalities, and are very heterogeneous in their demographics, socio-economic indicators and governance structures (Ministério da Saúde, 2020[2]).
In the recent past, strong economic growth and income distribution programmes were the driving forces for generating significant inequality and poverty reduction in Brazil. However, income inequalities have been rising again in recent years, and there are large regional disparities in prosperity and growth across the country, with North and Northeast regions faring worse than South and Southeast regions. Large inequalities along several dimensions affect health status.
2.2.1. Despite progress, socio-economic inequalities remain a significant problem in Brazil
Brazil has had strong economic growth combined with remarkable social progress over the past two decades. In 2010, Brazil GDP grew by 7.5%, compared to around 3% across OECD countries. Currently social benefits amount to over 15% of GDP, and are characterised by poor targeting if pensions are also included. As a result, poverty rates have been reduced from 41% of the population in 2001 to 19% in 2019.1 Public programmes have contributed to the decline in poverty rates (OECD, 2020[3]). Recent evidence shows that the Bolsa Familia programme alone has reduced poverty rates by 15% (Ferreira de Souza, Osorio and Paiva e Sergei Soares, 2019[4]).
These progresses have also generated reduction in income inequality. From 2001 to 2011, the GINI of income inequality in Brazil dropped continuously from around 58 to 52. However, it has been rising again in recent years, at around 53, and remains a significant problem in Brazil. Currently, the richest 10% of the population earn more than four times as much as the bottom 40% (OECD, 2020[3]).
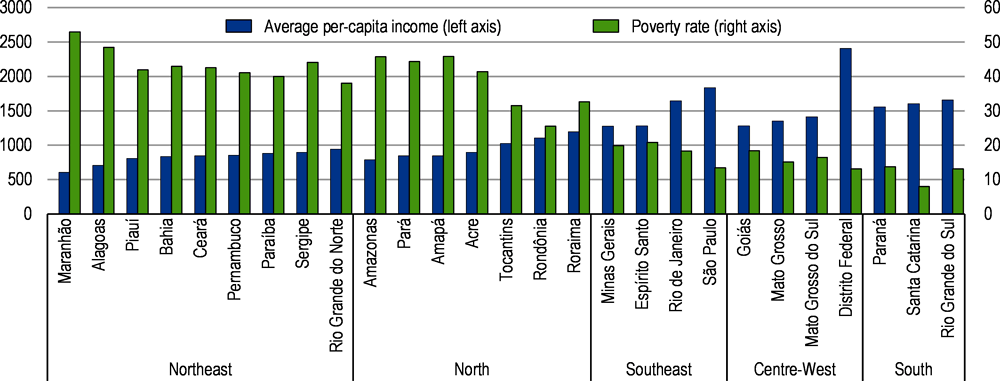
Regional inequalities are another crucial challenge in Brazil. The distribution of income across Brazilian regions is highly unequal. Average incomes in the Northeast state of Maranhão are less than half of the national average. The opposite holds true for poverty. The poverty rates in the North and Northeast regions are between three to four times higher than the poverty rates in the Southeast, Central-west and South regions (Figure 2.1). Large regional disparities also exist with regards to labour market informality and illiteracy, which are three to four times more common in the poorer North and Northeast regions than in the relatively affluent South and Southeast regions (OECD, 2020[3]). As the social and economic context strongly influences health outcomes, economic disparities across regions are mirrored in health status and health outcomes.
2.2.2. The management of the Brazilian Unified Health System is decentralised
The principles and structure of Brazil’s health care system were conceived in 1988 after the approval of the new Brazilian Constitution that established health as a universal right for the whole population. It became a state responsibility with the establishment of the Unified Health System (Sistema Único de Saúde, SUS). The SUS is structured around three main priorities (Massuda et al., 2020[6]):
The universal right to comprehensive health care at all levels of complexity (primary, secondary, and tertiary).
Decentralisation with responsibilities given to the three levels of government: federal, state, and municipal
Social participation in formulating and monitoring the implementation of health policies through federal, state, and municipal health councils.
The management of SUS is shared across three different levels of governance: Federal Ministry of Health, state departments and municipal health departments. At federal level, the Ministry of Health defines the general objectives of the SUS and sets policy development, planning financing, auditing and control of health policies and health services linked to SUS. It is responsible for the overall co-ordination of the national priorities and actions defines as part of the Multi-Annual Plan 2020-23 and the National Health Plan (Plano Nacional de Saúde, [PNS]) 2020-23. The health related objectives for the Multi-Annual Plan 2020-23 is the expansion of the coverage and resolution of PHC, improving prevention and strengthening of integration between health care services. The PNS 2020-23 elaborates on SUS health policy objectives, with the definition of seven programmes (Ministério da Saúde, 2020[7]):
In the area of PHC, the PNS 2020-23 is structured around three main priorities. First, the expansion of PHC access and of its infrastructure. Second, improvement in the digitalisation of PHC units, with better-integrated data and use of electronic medical records in North and Northeast regions. Third, increasing health promotion and prevention at PHC levels to address risk factors for health (for example nutrition and smoking) and encourage uptake of screening exams (for example cytopathology and mammography exams). The PNS 2020-23 defines 20 objectives in the area of PHC, with specific targets to achieve by 2023 around for example the number of Family Health Teams (both for the general and incarcerated populations), dental care coverage, pregnant women’s prenatal consultations, cytopathology and mammography exams coverage, and quality of mental health (Table 2.1).
The 26 state governments, through states secretary of health, are responsible for regional governance and the regional health system organisation, co-ordination of strategic programmes, and delivery of specialised health care services that have not been decentralised to municipalities. At local level, 5 570 municipalities, through municipal secretary of health, handle the management of SUS, including co-financing, co-ordination of health programmes, and direct delivery and contracting of health services, including PHC services (Massuda et al., 2020[6]).
The Interfederative Pact of Executive Management allows SUS to have a dynamic functioning through agreements between each federative entity, with the establishment of the following councils or commissions:
The Conselho Nacional de Secretários de Saúde (CONASS) brings together the health secretaries of the states and the Federal District with the purpose of implementing SUS principles, legislation and guidelines into health actions and services. CONASS also allows the exchange of experiences and information among States Secretaries.
The Conselho Nacional das Secretarias Municipais de Saúde (CONASEMS) represents municipal health departments, with the objective of guiding health managers for the provision of PHC services.
The Conselho Estadual de Secretarias Municipais de Saúde (COSEMS) brings together municipal secretaries of health to discuss and co-ordinates strategic health issues.
The Política Nacional de Atenção Básica (PNAB) describes the governance of PHC in Brazil, the roles of the main actors and other strategic aspects of the PHC policy. The federal government, the state governments and municipalities are the main actors involved in the governance of PHC in Brazil. The specific competencies of each level of government is foreseen in the Federal Constitution and the PNAB (art. 7, Ord. 2 436).
The formulation of policy priorities and actions for the PHC sector is agreed and approved during the CIT, which is made of representatives from the Ministry of Health, CONASS and CONASEMS. Decisions on the operational, financial and administrative aspects for the management of PHC are taken by consensus.
Within the Ministry of health, the PHC Secretariat (SAPS) (established in 2019 – Decreto nº 9 795) is responsible for defining and co-ordinating the PNAB. It is also responsible for allocating federal resources to finance PHC (on a monthly, regular and automatic basis), providing integrated support to the state and municipal managers, formulating strategies for monitoring and improving PHC quality, establishing national guidelines and providing technical and educational supports for PHC managers and professionals.
The states define decentralised PHC actions, strategies, guidelines, as well as rules for the implementation of the PNAB during the CIB, which is made of representatives from the state secretaries of health and COSEMs. States are expected to allocate financial resources for PHC, monitor PHC actions and care quality in municipalities, verify the quality and consistency of information sent by municipalities. They might also provide institutional support to the municipalities in the process of implementing and monitoring PHC and expanding the Family Health Strategy. States are expected to provide technical and educational instruments to the municipalities to facilitate training and continuous education of PHC managers and professionals.
Municipalities have the main attribution concerning the provision and financing of PHC services. They are responsible for organising, managing and providing services and actions within each territory. Municipalities have to provide support to PHC teams and units in the process of monitoring and expanding the Family Health Strategy. To this end, municipalities select, hire and remunerate the PHC professionals in accordance with the current legislation, and guarantee that PHC teams and units have sufficient material resources, equipment and supplies to deliver PHC services. They might organise effective patient flow within SUS and adopt referral mechanisms to ensure effective care co-ordination. Municipalities should keep the registration of teams, professionals, workload, available services and equipment on a monthly basis in the National Registry System of Health Establishments according to specific regulations. Community participation should also be guaranteed through social control. Lastly, municipalities are required to analyse and verify the quality and consistency of the data collected in the national health information systems to be sent to other spheres of management, use them in the health care planning and disseminate results.
Source: Information provided by Brazilian Ministry of Health.
The Comissão Intergestores Tripartite (CIT) and the Comissão Intergestores Bipartite (CIB) are important bodies for the development of SUS strategies and resource allocation through collective consensus from the different spheres of government (see Box 2.1). The National Health Council, a collegiate body composed of government representatives, service providers, health professionals and users, is also involved in the formulation of PHC priorities and actions. The OECD health system review provides a detailed description of these governance bodies (OECD, 2021[8]).
Since the establishment of SUS, Brazil has made substantial progress toward achieving universal health coverage. Virtually all of the population is covered for equal benefits and equal financial protection within the public health sector. Since its inception, a strong focus of SUS was to strengthen the role of PHC to reduce health inequalities and improve access to care, but also to move away from a health system that was historically very hospital-centred.
2.2.3. Brazil makes spending on PHC a priority
The public system is financed by tax revenues and social contributions from all three levels of government. By law, the federal government is required to spend 15% of net current government income on health, the states are required to spend 12% of total revenue on health, and municipalities are required to spend 15% of total revenue on health (Massuda et al., 2020[9]). It is reported that over the past 30 years, the share of municipal funding has increased to reach nearly one-fourth of their own total revenues on health (Massuda et al., 2020[9]).
Under SUS, the federal government has traditionally financed roughly one-third of total PHC costs (33%), with the remaining part being funded predominantly by municipalities (61%) (Ministério da Saúde/Fundação Oswaldo Cruz, 2018[10]). The participation of states is the smallest, with very few cases where states co-finance policies for PHC.
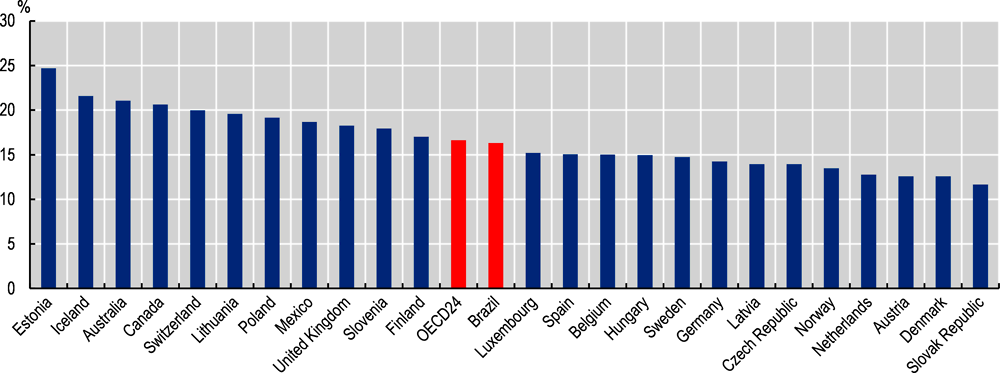
Analysing the composition of overall health spending in an international context, Brazil seems to make spending on PHC a higher priority than many OECD countries. In 2019, Brazil dedicated around 16% of its financial resources to general outpatient care, dental care, home-based curative care and preventive activities (Figure 2.2).
In 2020, the budget allocated to PHC from the federal government was BRL 20.9 billion, compared to BRL 17.5 billion in 2019 (CONASEMS, 2020[11]). In total, the federal government increased its PHC budget by around BRL 3.4 billion between 2019 and 2020.
Since SUS inception, Brazil has made significant developments by improving in most of the general population health indicators. Brazil is however undergoing a profound demographic transition. As a result of decrease in fertility and mortality rates, the Brazilian population is rapidly ageing. The rapidly ageing population and increasing risk factors for health in Brazil (notably growing overweight rates) goes hand in hand with an increased prevalence of chronic non-communicable diseases, which call for effective prevention and stronger PHC to better manage the burden of chronic conditions.
2.3.1. Life expectancy at birth has improved in recent years, but is still falling behind other OECD countries
Life expectancy at birth in Brazil increased rapidly over the past decades, but is still five years below the OECD average of 81 years but above the LAC average of 75.6 years (see Figure 2.3). In Brazil, life expectancy at birth increased by more than five years between 2000 and 2019 (rising from 70.2 to 75.9 years), compared to four years across OECD countries. The gap in longevity between Brazil and other OECD countries has shortened from 6.5 years to 5.1 years.
Infant mortality rates have decreased from 30.3 deaths per 1 000 live births in 2000 to 12.4 deaths per 1 000 live births in 2019. Despite this decrease, the infant mortality rate in Brazil is still above the OECD average of 4.2 deaths per 1 000 live births. The same is true for maternal mortality rates in Brazil, which have decreased to 60 women per 100 000 live births in 2017 (13 percentage points reduction since 2000), although still higher than the OECD average of 8 per 100 000 live births but lower than the LAC average of 83 (OECD/The World Bank, 2020[13]).
2.3.2. Brazil faces rapid ageing of its population
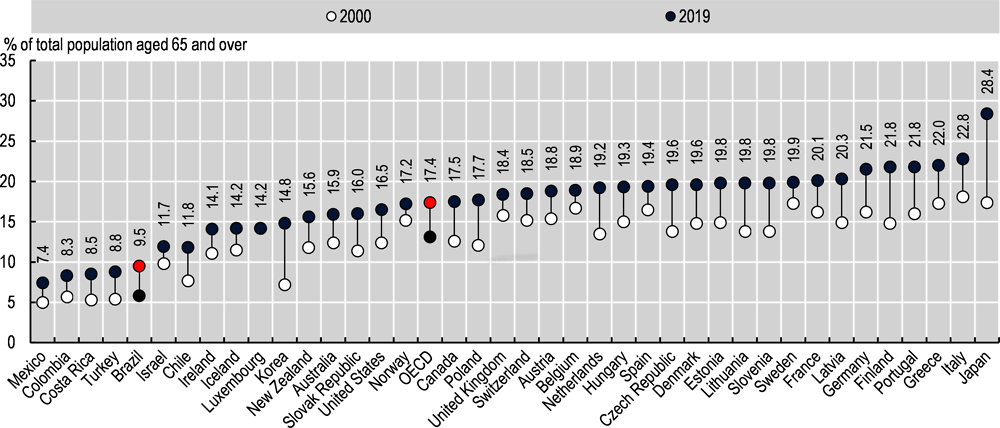
Brazil, similarly to other OECD countries, is experiencing a demographic transition characterised by a shift from high levels of mortality and fertility to lower levels. The fertility rate fell from 2.9 births per woman in 1990 to 1.7 births per woman in 2019 (OECD, 2021[14]). The combination of falling mortality rates (resulting in increasing life expectancy) and fertility rates causes rapid population ageing. The share of the population aged over 65 years has increased by 65% over the past decade, rising from 5.8% in 2000 to 9.5% in 2019 (Figure 2.4). Across the OECD, the share has increased by 32% over the same period, rising from 13.1 in 2000 to 17.4 in 2019.
Therefore, the dependency ratio (the number of people of working age for every person aged 65 years and more) is projected to substantially decrease by 2050, close to the OECD level. The rapid ageing population has an important impact on the health of the population in Brazil, putting pressure on both the health care systems and the economy.
2.3.3. Rapidly increasing risk factors for health and associated ill-health are a major concern
Several risk factors for health give cause for concern in Brazil, including particularly overweight. Being overweight is a major risk factor for various chronic non-communicable diseases including diabetes, cardiovascular diseases and certain cancers. While overweight in Brazil is currently below OECD average, the trend is increasingly upwards. In 2016, estimations show that 56.5% of adults in Brazil were overweight, close to the OECD average of 58.4%. However, Brazil showed the fourth largest change in overweight between 2006 and 2016 with a growth of 13% in the past decade, compared to an increase of 8% across the OECD. This is the third highest growth rates behind Japan, Costa Rica and Korea (Figure 2.5).
Children overweight rates in Brazil are also increasing at a fast rate. In 2016, Brazil had a children overweight rate of 28%, very close to the 28.5% in average amongst OECD countries. Nevertheless, Brazil experienced an increase of 27% between 2006 and 2016, higher than the 15% increase in the OECD. Increasing children overweight rates means higher risk of cardiovascular diseases or diabetes during adult age, putting further pressure on the PHC sector.
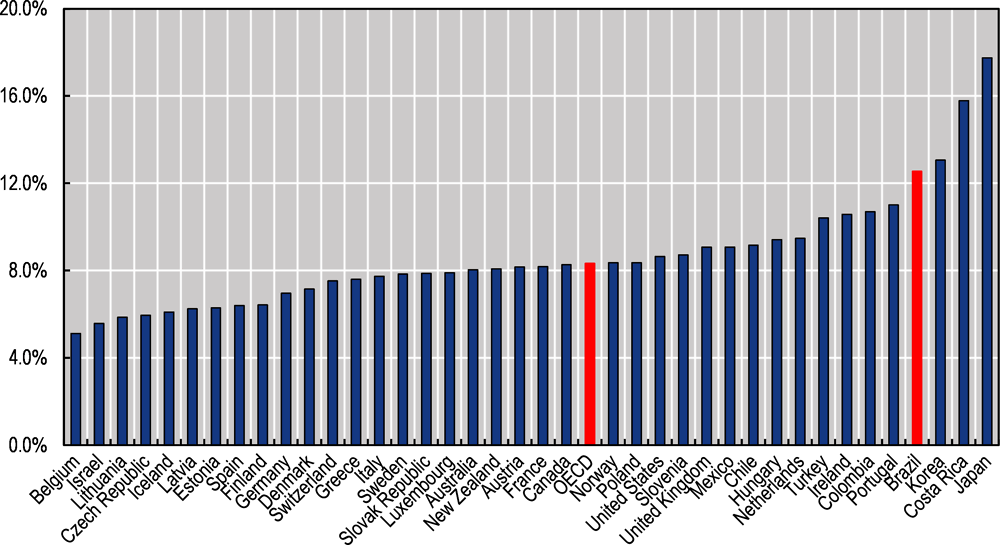
Already, when compared to OECD countries, diabetes represents a higher burden of disease in Brazil. Raised levels of blood sugar can lead to the development of diabetes. Fasting blood glucose (FBG) contributes to diagnose and monitor diabetes. In Brazil, 8.3% of the population had raised FBG in 2014, above the 6.7% average in OECD countries. Importantly, between 2004 and 2014, Brazil recorded one of the largest increase in its population with raised FBG, increasing by 15.3% (Figure 2.6). Only Turkey, Mexico, Chile, Costa Rica and Colombia had larger increases amongst OECD countries, evidencing a worrying trend in Brazil.
Overall, with increasing risk factors for health, the predominance of chronic non-communicable diseases is growing in Brazil. In 2017, four chronic non-communicable diseases dominated the causes of mortality in Brazil: circulatory system diseases (27%), neoplasms (17%), chronic respiratory diseases (12%), external causes (12%) and diabetes (5%), compared to only two in 1990 (cardiovascular diseases with 27.8%, and neoplasms with 11.4%).
2.3.4. There are large regional differences in health
There are large regional inequalities in health status across Brazil, where the most vulnerable municipalities consistently present poorer health outcomes than national average. While infant mortality rate in Brazil has decreased from 47.1 to 12.4 per 1 000 live births between 1990 and 2019, there are large differences in the magnitude of this reduction across Brazil’s regions. The Northeast region showed the most significant decline of 80% in the period, while the lowest degree of reduction occurred in the Centre-west and North regions (reduction of 62%) (Szwarcwald et al., 2020[16]).
Another illustration of regional differences in health can be seen in terms of avoidable hospitalisation for conditions that could be treated in the PHC setting. The proportion of hospitalisations due to conditions that could be more effectively treated in the PHC setting ranges from 24% in the South region to 40% in the North region (Figure 2.7). Such regional differences point out that some remote and vulnerable areas require more attention than others to improve quality of PHC.
There are also significant inequalities in the rates of vaccination against yellow fever in Brazilian states where vaccination has been recommended, ranging, in 2018, from 21.8% in Sergipe to 100% in the Federal District and Roraima (the national average for all states where vaccination is recommended is 64.1%).
Regional inequalities in health have aggravated the impact of the COVID-19 pandemic and will likely exacerbate health inequalities in the future. The most precarious and vulnerable population are more likely to be affected by the COVID-19 virus, not only because of poor living and working conditions, but also because they are more likely to suffer from comorbidities and risk factors for COVID-19 severity. Mortality rates in the State of Amazonas have been found four-times higher than the national average, particularly among indigenous people (Pires, Carvalho and Rawet, 2020[17]). Box 2.2 presents the impact of COVID-19 on health in Brazil.
The first case of COVID-19 in Brazil was reported on the 25th of February 2020. Since then, the impact on population health has been large. The total number of registered deaths is above 611 000 as of 17 November 2021 with 41 000 average monthly registered deaths in 2021. This situates COVID-19 as the first cause of death during the pandemic when compared to the average monthly figures for 2015-19 of deaths attributed to other conditions, the highest ones being 30 000 for circulatory diseases, 18 500 for cancers, and 13 000 for diseases of the respiratory system. However, there are scientific basis showing an underreporting of around 22% due to limitations to perform the SARS-CoV-2 screen by RT-PCR test (Carvalho, Boschiero and Marson, 2021[18]).
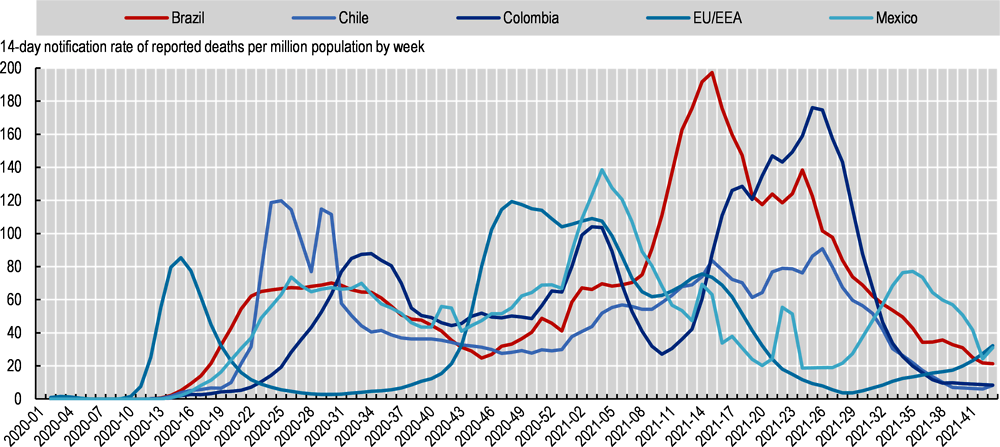
The mortality epidemic curve in Brazil experienced an increase in cases by early April 2020, reaching the first peak during July 2020, later than what Europe experienced in the early months of the pandemic (Figure 2.8). Then, cases started to reduce but still with high level of virus circulation and mortality rates, similar to other Latin American countries such as Chile, Colombia and Mexico but dissimilar to Europe where mortality was substantially lowered between July and September. By mid-November, cases in Brazil began to rise once again. By the beginning of April 2021, mortality rate in Brazil reached its highest levels since the start of the pandemic and then started to decline.
One of the most important problems in handling the COVID-19 pandemic in Brazil was weaknesses in governance of the health sector. At the federal level, in the first year of the pandemic, four different ministers of health were in office, limiting continuity in the management of the response. Risk communication from federal authorities has also been conflicting and confusing for the population. Brazil is not unique, in that other OECD countries have pursued similar approaches.
As highlighted in Chapter 3, the COVID-19 crisis demonstrates the importance of placing PHC at the core of health systems, both to reduce pressure on health systems and minimise complications and direct deaths from the COVID-19, as well as to maintain ongoing routine care to patients who do not have COVID-19.
In Brazil, the 5 570 municipalities handle the management, organisation and delivery of PHC. The Family Health Strategy programme launched in 1994 was remarkable. Based on multi-professionals PHC teams (called Family Health Teams), the expansion of the Family Health Strategy led to improvement in health care coverage and health outcomes. SUS prioritisation on PHC permitted an easier contact with health services at the community level.
2.4.1. Municipalities have primary responsibility for managing and delivering PHC
Since the implementation in 1994 of the federal programme called the Family Health Strategy (Estratégia de Saúde da Família – ESF), also known as the Family Health Programme (Programa Saúde da Família), the 5 570 municipalities have primary responsibility for managing and delivering PHC. With federal funding, municipalities have the freedom to organise family health teams according to the population needs and geographic characteristics.
The ESF is a decentralised programme aimed at expanding the PHC system in Brazil toward more co-ordinated, comprehensive and continuous care. The overarching objective was to ensure universal access to health care services for all Brazilians under the overall organisation of SUS (Macinko and Harris, 2015[20]; Castro et al., 2019[21]). The ESF became the main mechanism for expanding coverage to PHC services in Brazil. The ESF resulted in two major shifts. First a shift in priorities, from treating patients with diseases to delivering comprehensive care and preventing diseases through active health promotion. Second a shift in governance, from states to municipalities to allow for greater accountability and more collaboration between the private and public sector.
The ESF is funded through federal transfers but also includes financial contributions from municipalities. As earlier mentioned, the municipalities is the main financing agent of PHC. Smallest municipalities (up to 20 000 inhabitants), where there is no other supply of health care services, spend around 60% of their health expenditure directed towards PHC.
2.4.2. Public PHC is free of charge and is expected to be the initial contact point to SUS
SUS offers preventive services and PHC free of charge. Services that are publicly covered are based on health conditions, clinical and nonclinical procedures, and target population groups. The list of services has been gradually adapted to reflect changes in population health. Treatment and control of major chronic conditions (such as hypertension and diabetes) have been added in the list of services covered (OECD, 2015[22]). The federal Ministry of Health negotiates with state and municipal health secretariats to decide new health care services to be covered by SUS.
PHC provided by the ESF is expected to be the initial contact point for patients having new health needs, although it does not work as a “gatekeeper” and many Brazilian have direct access to outpatient specialties and hospital. For example, the latest Health Information Survey found that around 50% of the diabetic population identified basic health units as their last contact with the health system, 11% used public speciality units in hospitals, 6% public urgent care units and 30% private practices or clinics (IGBE, 2020[23]).
This is unlike many other OECD countries such as Australia, Canada, or the United Kingdom where general practitioners operate as gatekeeper to the health system as a referral is required and compulsory to access to specialist and hospital care (OECD, 2020[24]).
In PHC, private sector is more supplemental as health plans mainly offer specialist and hospital services. However, health plans in the private sector have begun to offer access to family doctors with no co-payment as an alternative to specialist visits (Massuda et al., 2020[9]).
2.4.3. PHC in Brazil is provided by multidisciplinary Family Health Teams
Prior to 1994, the role of PHC and health promotion was limited and services were predominantly delivered in a range of hospitals. As a community-based, large-scale PHC programme, the ESF relies on multi-professional teams called Family Heath Teams (FHTs). Each FHT is assigned a geographic area, covering up to 4 000 individuals located in non-overlapping areas. This helps FHTs to consider social, economic and environmental factors of the catchment area. FHT are responsible for registering every family in their geographic area, and are thus designed to facilitate access to the health care system (Massuda et al., 2020[9]).
A range of different health professionals are involved in PHC delivery. The FHT include physicians, nurses, and up to 12 community health workers. Other PHC workers, including nutritionists, pharmacists, social workers, psychologists, obstetricians and gynaecologists, and public health workers can provide additional support depending on local needs. Oral health teams have been integrated to the FHT in recent years to provide universal and free oral health services to the population. By 2019, there were 43 234 Family Health Teams and 27 564 Oral Health Teams in operation throughout Brazil (Figure 2.9). Solo practice in Brazil is thus becoming scarce, although there is no official registration and reporting of this practice.
This model of service delivery – based on multidisciplinary team – is well aligned with modern approaches to PHC which house multiple professionals with advanced skills working in teams (OECD, 2020[24]). Such models of PHC based on teams or networks of providers were reported by 18 OECD countries in 2018, including Australia, Canada, France, Switzerland or the United States.
FHTs are working in basic health care units (Unidades Basicas de Saude – UBS) or other PHC facilities called health clinics, health centres or health posts, and can also receive support from the Family Health Support Centers (Nucleos de Apoio à Saúde da Familia – NASFs). NASFs were introduced in 2008 to provide support to between one and nine FHTs. NASF is composed of health and social workers included for example acupuncturists, social workers, physical education professionals, pharmaceuticals, physiotherapists, gynaecologists and obstetricians; homeopathic doctors; nutritionists; paediatricians or psychologists. By 2019, there were 4 487 NASFs in operation throughout Brazil (see also Chapter 4 for a detailed description of NASFs). As of May 2021, there is a total of 50 029 PHC facilities in Brazil, including among other UBS, Health Post and NASFs.
In 2020, the government introduced a new classification of 12 health teams categories (Table 2.2 summarises the various family health teams in Brazil).
The scope of practice of the FHT has gradually increased over the past years to provide proactive preventive care and deliver public health intervention including for instance immunisation programmes and screening programmes (see Chapter 3). Services include not only maternal and child health care services, but also entail preventive care and control and management of chronic non-communicable diseases (Özçelik et al., 2021[25]). The FHT also link patients with social services (such as conditional cash transfer programmes), water and sanitation services, law enforcement, and school programmes (Massuda et al., 2020[9]).
2.4.4. The expansion of the Family Health Strategy has been remarkable, improving health care coverage and health outcomes
In 2019, 98% of the municipalities had adopted the Family Health Strategy model. In 2019, there were 43 223 family health teams, 27 564 oral health teams and 4 487 family health support centres (Figure 2.9), providing care to more than 127 million people (61% of the population). The number of family health teams and oral health teams has increased by respectively 36% and 34% over the past decade. At the same time, the number of NASFs has more than tripled over the past decade (Figure 2.9). As of May 2021, there are more than 50 000 PHC facilities in Brazil where teams can deliver services.
There are strong evidence suggesting that the FHT provides better access and quality than other traditional health posts and centres (Massuda et al., 2020[9]). In a systematic review of the literature examining the impact of the ESF in Brazil, Bastos et al. (2017) show that increasing health care coverage through the expansion of the ESF was consistently associated with improvement in child mortality (Bastos et al., 2017[26]). A longitudinal analysis using panel data show that a 10% increase in FHT coverage was associated with a 4.5% decrease in infant mortality rate, all other things being equal (Macinko, Guanais and Marinho De Souza, 2006[27]).
Among adults, expansion of the ESF was associated with reductions in hospitalisations for diabetes mellitus and respiratory problems (Guanais and MacInko, 2009[28]). Estimations show that the ESF may have contributed to an estimated 126 000 fewer hospitalisations between 1999 and 2002. More recently, Pinto and Giovanella (2018) show that the implementation of the ESF was associated with a reduction of 45% of the standardised hospitalisation rates per 10 000 inhabitants between 2001 and 2016. The decline was particularly pronounced for hospitalisation due to asthma, gastroenteritis and cardiovascular and cerebrovascular diseases (Pinto and Giovanella, 2018[29]). The implementation of the ESF is also positively associated with a significant reduction in the number of hospitalisations for heart failure and stroke per 10 000 inhabitants from 1998 to 2013 (De Fátima Barros Cavalcante et al., 2018[30]). Better prevention of PHC sensitive conditions, greater follow-up for chronic conditions, improved diagnosis, and easier access to medicines partly explain improvement in health care quality.
In addition to improving health outcomes through better access to care, the SUS made considerable investments to expand the availability and equipment of PHC facilities through the Requalifica programme. The programme carries out construction, expansion and refurbishment of the PHC facilities, including the construction of the Basic Fluvial Health Units, providing better conditions for accessing and offering public health actions and services. It also involves actions aimed at the computerisation of PHC, and the qualification of PHC workers (Ministério da Saúde, 2020[2]).
While these are all welcome news, the ESF expansion has also been marked by stark disparities across the states and municipalities (Andrade et al., 2018[31]). The ESF expansion has been heterogeneous across municipalities mainly because of geographic imbalances in the supply of physicians. The lack of PHC physicians in some remote municipalities has been one of the most important barrier to the expansion of the ESF (Andrade et al., 2018[31]).
2.4.5. The role of community health workers is predominant
Following the implementation of the Community Health Agents Programme (PACS), community health workers (CHWs) started to play a crucial role in the Brazilian PHC system. CHWs are frontline public health workers, often members of the communities in which they work. They have valuable knowledge of people needs and are trustful source of information. The implementation of the ESF gave an expanded role of CHWs, at the core of the country’s PHC policy (Wadge et al., 2016[32]).
CWHs are integrated members of the FHT. They provide comprehensive PHC supports including clinical triage, supporting chronic disease management, screening uptake, immunisations, providing pre- and postnatal care assistance, health promotion, social determinants, community participation and household data (Wadge et al., 2016[32]). They are expected to resolve many low-level problems such as medication review for chronically ill patients, while referring more complex issues to doctors and nurses of the FHT. At the clinic or health posts, CHWs are also responsible for organising the waiting rooms and appointments for other health workers, and offering educations sessions.
Each CHW is assigned to maximum 150 households in a geographic area, and each household receives at least one visit every month from a dedicated CHW irrespective of needs or demand. Patients are not able to choose their CHW. Monthly visits allow health promotion activities and basic clinical care, checking whether prescriptions have been filled and whether patients have been taking their medications regularly, identifying risk factors for health or other social determinants, but also collecting individual and household level data (Wadge et al., 2016[32]). CHWs also help co-ordinate PHC services with public health efforts.
In 2020, more than 250 000 CWHs served 61% of the population (see Chapter 5), up from 60 000 in 1998. The minimum requirement to become a CHW is to get secondary education, but around two-thirds of them have a professional diploma. CHWs are most often recruited from within their own community. It is a stable and respectful profession and as a result, turnover is low.
A large body of evidence demonstrates the positive impact of CHWs on patient satisfaction and health literacy, notably for low-income and vulnerable groups (Wadge et al., 2016[32]; Grossman-Kahn et al., 2018[33]). CHWs have been key to effectively respond to the Zika virus for instance, providing health advice and incidence reporting. CHWs could thus have played a greater role to support the COVID-19 response. So far, evidence shows that only an estimated 9% of CHWs have received infection control training and personal protective equipment during the pandemic. They have not been provided with clear guidance about their role in the COVID-19 response. The COVID-19 pandemic has revealed governance issues linked to the health sector, mainly due to a lack of leadership and oversight from the federal government. Risk communication from federal authorities has also been conflicting and confusing for the population and PHC workers, with no overall co-ordination (Lotta et al., 2020[34]).
2.4.6. Municipalities are responsible for hiring health professionals for PHC, with wide variations across the country
In the decentralised health care system, municipalities are responsible for the organisation, management and delivery of PHC services. In 2020, the federal government provided BRL 20.9 billion to the municipalities, which were then responsible for organising and delivering PHC services, by hiring FHT members as civil servants. As each municipality defines the level of salaries for health team members, there are wide wage variations across the country (Massuda et al., 2020[6]).
There are three types of possible contractual schemes with the municipality:
Public officials: there are civil servants hired as statutory workers (there are salaried, with a stable position and there is a ceiling of money to pay them);
Private workers hired by social organisations, non-profit private NGO (but anecdotal evidence suggests there are forms of corruption under such schemes),
Private workers hired by Government owned social organisation NGO.
2.4.7. There are too few PHC physicians in Brazil
The number of trained PHC physicians is well below the OECD countries, and of other LAC countries. In Brazil, practicing doctors per 1 000 population in 2019 were very low compared to the OECD average, at 2.3 compared to 3.5 (Figure 2.10). This is among the lowest density, just above Colombia (with 2.2 doctors per 1 000 population) and the LAC average (2.1 doctor per 1 000 population). However, the number of doctors increased by 50% in Brazil over the past decade.
At the same time, while the specialty of family and community medicine was introduced as a clinical and licensed specialty, the number of PHC doctors has not increased accordingly. In Brazil, PHC is mostly delivered by physicians who do not have any specialty or by physicians with a specialty in internal medicine (see Chapter 5).
In 2020, there are around 60 000 medical doctors working in PHC, alongside 50 000 nurses and 35 000 dentists currently in practice in Brazil. In 2018, only 5 486 medical doctors had a specialty training in family and community medicine, representing only 1.4% of all specialists in Brazil (see Table 2.3). Medical doctors specialised in internal medicine who have some competencies in family medicine to provide PHC, represent 11.2% of all specialists in Brazil. Lastly, there are 169 479 physicians, with no specialty training, representing around 37% of all medical doctors.
2.4.8. The uneven distribution of medical doctors is a major concern in Brazil
There is a marked disparity in the concentration of doctors in different regions and states, and between state capitals and other parts of states. Overall, there are 2.3 doctors per thousand population (Figure 2.10) but there are capitals with more than 12 doctors per thousand population – like Vitória, in Espírito Santo – and in the interior part of the Northeast region or in the Amazon with values below one doctor per thousand inhabitants. The Southeast is the region with the highest medical density per inhabitant (with 2.81 per thousand population), against 1.16 per thousand population in the North and 1.41 in the Northeast (Scheffer et al., 2018[35]).
Among states, the Federal District has the highest density with 4.35 doctors per thousand population, followed by Rio de Janeiro (with 3.55 doctors per thousand population), São Paulo (with 2.81), Rio Grande do South (with 2.56), Espírito Santo (with 2.40), and Minas Gerais (with 2.30). At the other end of the scale, are states of the North and Northeast. Maranhão presents the lowest density of medical doctors with 0.87 doctor per thousand population, followed by Pará with 0.97 doctor per thousand population (Scheffer et al., 2018[35]).
Geographical inequalities in the distribution of medical doctors hold true when looking at physicians with specialty training. Evidence indicates a clustering of PHC specialists in some regions: the best supplied regions are the South and Southeast Regions, followed by the Central-West (Scheffer et al., 2018[35]). Workforce imbalance across regions is analysed in further details in Chapter 5 of this report.
Several nationwide initiatives have attempted to address the imbalances in the distribution of health workers. Brazil introduced several programmes to improve access to medical training in underserved communities, including the 2001 Programme of the Interiorisation for Health Work (Programa de Interiorização do Trabalho em Saúde), the 2011 Programme for Valuing PHC Professionals (Programa de Valorização dos Profissionais da Atenção) and the 2013 More Doctors Programmes (Programa Mais Médicos).
As described by Chapters 4 and 5 of this report, the More Doctor Programme (MDP) is considered as the world’s largest government-led initiative that recruited domestic and foreign physicians to work in PHC settings within municipalities that typically faced difficulties in recruitment and retention. By November 2020, the programme was responsible for the presence of 16 426 doctors in 3 837 Brazilian municipalities. This programme has proven to have positive results, for instance, in terms of investment in PHC facilities, doctors availability and health outcomes (Hone et al., 2020[36]; Netto et al., 2018[37]).
On a less positive note, unfilled medical positions are still common in Brazil, even after the implementation of the MDP. In April 2019, it is estimated that 3 847 public sector medical positions in almost 3 000 municipalities remained unfilled (Scheffer et al., 2018[35]). Unfilled medical positions in the PHC sector certainly impede prevention, early diagnoses, the monitoring of children, pregnancies and the continuation of treatments for those having underlying health conditions.
In Brazil, the 5 570 municipalities handle the management, organisation and delivery of PHC. SUS offers preventive services and PHC free of charge for its population, based on multidisciplinary family health teams. Overall, the organisation of PHC delivery in Brazil is well aligned with modern approaches to PHC, which house multiple professionals with advanced skills working in teams. SUS prioritisation on PHC also permitted an easier contact with health services at the community level. The implementation of the Family Health Strategy, one of the largest community-based PHC programme worldwide, has contributed to increase population coverage, and led to measurable improvements in terms of infant mortality rates, maternal health, and avoidable hospitalisations. The life expectancy at birth in Brazil increased rapidly over the past decades – faster than across the OECD countries.
Despite major investments to improve access to PHC, health continue to be unequally distributed with people in North and Northeast regions suffering from poorer health outcomes. In part, these disparities are linked to workforce shortages and imbalances in the distribution of medical doctors, as well as lower PHC infrastructure and equipment in North and Northeast regions. There are also been a rise in the number of elderly patients and an increasing prevalence of chronic non-communicable diseases, which call for more effective prevention and stronger PHC to better manage the burden of chronic conditions. Brazil will need to continue to invest in a strong PHC system that is responsive to people’s changing needs, capable of offering continuous, proactive and preventive care. The next four chapters set out in detail where changes are needed and how it can be achieved, notably to increase screening and prevention for the main chronic non-communicable diseases (Chapter 3), enhance the quality of PHC provision (Chapter 4), tackle workforce challenges in PHC (Chapter 5) and promote the digitalisation of PHC (Chapter 6).
References
[26] Bastos, M. et al. (2017), “The impact of the Brazilian family health on selected primary care sensitive conditions: A systematic review”, PLoS ONE, Vol. 12/8, https://doi.org/10.1371/journal.pone.0182336.
[18] Carvalho, T., M. Boschiero and F. Marson (2021), “COVID-19 in Brazil: 150 000 deaths and the Brazilian underreporting”, Diagnostic Microbiology and Infectious Disease, Vol. 99/3, p. 115258, https://doi.org/10.1016/j.diagmicrobio.2020.115258.
[21] Castro, M. et al. (2019), “Brazil’s unified health system: the first 30 years and prospects for the future”, The Lancet, Vol. 394/10195, pp. 345-356, https://doi.org/10.1016/s0140-6736(19)31243-7.
[11] CONASEMS (2020), Painel de Apoio – Previne Brasil – Resultado 2020, https://www.conasems.org.br/painel/previne-brasil-resultado-2020/.
[30] De Fátima Barros Cavalcante, D. et al. (2018), Did the family health strategy have an impact on indicators of hospitalisations for stroke and heart failure? Longitudinal study in Brazil: 1998-2013, https://doi.org/10.1371/journal.pone.0198428.
[19] ECDC (2021), COVID-19 situation updates, https://www.ecdc.europa.eu/en/COVID-19/situation-updates.
[4] Ferreira de Souza, P., R. Osorio and L. Paiva e Sergei Soares (2019), Os Efeitos do Programa Bolsa Família sobre a Pobreza e a Desigualdade: um balanço dos primeiros quinze anos, https://www.ipea.gov.br/portal/images/stories/PDFs/TDs/td_2499.pdf.
[33] Grossman-Kahn, R. et al. (2018), “Challenges facing Community Health Workers in Brazil’s Family Health Strategy: a qualitative study”, Int J Health Plann Manage., Vol. 33/2, https://doi.org/10.1002/hpm.2456.
[28] Guanais, F. and J. MacInko (2009), “Primary care and avoidable hospitalisations: Evidence from Brazil”, Journal of Ambulatory Care Management, Vol. 32/2, https://doi.org/10.1097/JAC.0b013e31819942e51.
[36] Hone, T. et al. (2020), “Impact of the Programa Mais médicos (more doctors Programme) on primary care doctor supply and amenable mortality: quasi-experimental study of 5 565 Brazilian municipalities”, BMC Health Services Research, Vol. 20/1, p. 873, https://doi.org/10.1186/s12913-020-05716-2.
[5] IBGE (2019), Síntese de Indicadores Sociais: uma análise das condições de vida da população, https://biblioteca.ibge.gov.br/visualizacao/livros/liv101678.pdf.
[23] IGBE (2020), Pesquisa Nacional de Saude 2019: percepção do estado de saúde, estilos de vida, doenças crônicas e saúde bucal: Brasil e grandes regiões, IGBE, https://www.ibge.gov.br/estatisticas/sociais/saude/9160-pesquisa-nacional-de-saude.html?=&t=publicacoes.
[31] Kroneman, M. (ed.) (2018), “Transition to universal primary health care coverage in Brazil: Analysis of uptake and expansion patterns of Brazil’s Family Health Strategy (1998-2012)”, PLOS ONE, Vol. 13/8, p. e0201723, https://doi.org/10.1371/journal.pone.0201723.
[34] Lotta, G. et al. (2020), “Community health workers reveal COVID-19 disaster in Brazil”, The Lancet, Vol. 396, https://doi.org/10.1016/S0140-6736(20)31521-X.
[27] Macinko, J., F. Guanais and M. Marinho De Souza (2006), “Evaluation of the impact of the Family Health Program on infant mortality in Brazil, 1990-2002”, Journal of Epidemiology and Community Health, Vol. 60/1, https://doi.org/10.1136/jech.2005.038323.
[20] Macinko, J. and M. Harris (2015), “Brazil’s Family Health Strategy – Delivering Community-Based Primary Care in a Universal Health System”, New England Journal of Medicine, Vol. 372/23, pp. 2177-2181, https://doi.org/10.1056/nejmp1501140.
[6] Massuda, A. et al. (2020), Brazil – International Health Care System Profiles, Commonwealth Fund, https://www.commonwealthfund.org/international-health-policy-centre/countries/brazil (accessed on 2 December 2020).
[9] Massuda, A. et al. (2020), Brazil., International Health care System Profiles, https://www.commonwealthfund.org/international-health-policy-centre/countries/brazil (accessed on 8 September 2020).
[2] Ministério da Saúde (2020), Plano Nacional de Saúde 2020-23.
[7] Ministério da Saúde (2020), Plano Nacional De Saúde 2020-23, https://bvsms.saude.gov.br/bvs/publicacoes/plano_nacional_saude_2 020_2023.pdf (accessed on 15 March 2021).
[10] Ministério da Saúde/Fundação Oswaldo Cruz (2018), Contas do SUS na perspectiva da contabilidade internacional: Brasil 2010-14, https://portalarquivos.saude.gov.br/images/pdf/2018/junho/22/CONTAS-DO-SUS.pdf.
[37] Netto, J. et al. (2018), Contributions of the Mais Médicos (More Doctors) physician recruitment programme for health care in Brazil: An integrative review, Pan American Health Organization, https://doi.org/10.26633/RPSP.2018.2.
[14] OECD (2021), “Fertility rates (indicator)”, https://doi.org/10.1787/8272fb01-en.
[12] OECD (2021), OECD Health Statistics, http://stats.oecd.org/.
[8] OECD (2021), OECD Reviews of Health Systems: Brazil 2021, OECD Publishing, Paris, https://doi.org/10.1787/146d0dea-en.
[3] OECD (2020), OECD Economic Surveys: Brazil, OECD Publishing, https://doi.org/10.1787/250240ad-en.
[24] OECD (2020), Realising the Potential of Primary Health Care, OECD Publishing, Paris, https://doi.org/10.1787/a92adee4-en.
[22] OECD (2015), OECD Economic Surveys: Brazil 2015, OECD Publishing, Paris, https://dx.doi.org/10.1787/eco_surveys-bra-2015-en.
[13] OECD/The World Bank (2020), Health at a Glance: Latin America and the Caribbean 2020, OECD Publishing, Paris, https://dx.doi.org/10.1787/6089164f-en.
[1] OECD/UCLG (2019), 2019 Report of the World Observatoryon Subnational Government Finance and Investment – Country Profiles.
[25] Özçelik, E. et al. (2021), “A Comparative Case Study: Does the Organization of Primary Health Care in Brazil and Turkey Contribute to Reducing Disparities in Access to Care?”, Health Systems & Reform, Vol. 7/2, https://doi.org/10.1080/23288604.2021.1939931.
[29] Pinto, L. and L. Giovanella (2018), “The family health strategy: Expanding access and reducing hospitalisations due to ambulatory care sensitive conditions (ACSC)”, Ciencia e Saude Coletiva, Vol. 23/6, https://doi.org/10.1590/1413-81232018236.05592018.
[17] Pires, L., L. Carvalho and E. Rawet (2020), “MULTI-DIMENSIONAL INEQUALITY AND COVID-19 IN BRAZIL”, IE, Vol. 80/315.
[35] Scheffer, M. et al. (2018), Demographia Médica No Brasil 2018.
[16] Szwarcwald, C. et al. (2020), “Inequalities in infant mortality in Brazil at subnational levels in Brazil, 1990 to 2015”, Population Health Metrics, Vol. 18/S1, p. 4, https://doi.org/10.1186/s12963-020-00208-1.
[32] Wadge, H. et al. (2016), “Brazil’s Family Health Strategy: Using Community Health Workers to Provide Primary Care”, The Commonweath Fund Publication, Vol. 14/1914.
[15] WHO Global Health Observatory (2017),, https://www.who.int/data/gho.
Note
← 1. The poverty rates is measured by the poverty headcount ratio at USD 5.50 a day (2011 PPP).