3. Financial sustainability of health spending and efficiency
The introduction of the Sistema Único de Saúde (SUS) has been a major achievement for Brazil in increasing access to health care services and reducing health inequalities. However, sufficient financing has been a constant challenge since its inception and there is dissatisfaction with apparent inefficiencies in the Brazilian health system. Recent projections suggest that a substantial increase in health spending will be necessary over the next decades to meet future health and long-term care needs. A combination of initiatives that focus, on the one hand, on generating fiscal space to allow for more public financing in health, and on the other hand, on facilitating a more efficient provision of health care can help meet future health care financing needs. Fiscal space could, for example, be achieved by reducing the tax deductibility of private health spending. Potential for efficiency gains exist throughout the health system.
Modern, patient-centred health systems need to make sure that sufficient financial and physical resources are available to meet population health needs now but also in the future. This requires flexible financing mechanisms that increase available funding if needed. On the other hand, tools need to be in place to make sure that any additional funding is “value for money” and the health services are provided efficiently. For this reason, this chapter analyses the financial sustainability of health spending in Brazil and the efficiency of the health system.
The chapter is structured as follows. First, health spending in Brazil is put into context by comparing it to OECD countries and contextual information on the health financing infrastructure in Brazil is provided. After displaying the latest health spending projection for Brazil until the year 2040, the different options on how to finance future health and long-term care needs associated with an ageing society and their feasibility are discussed. These options include a general increase of government spending, the re-allocation of public resources within the existing public spending towards health or leaving more future health financing obligations to the private sector.
A fourth option to address the increasing health financing needs in Brazil that will be discussed extensively in the chapter is to find efficiency gains in the health system. The analysis will cover the entire health system including primary health care, hospital care, pharmaceutical spending, long-term care or administration including planning and co-ordination. All the areas will be analysed in depth and any potential for efficiency gains highlighted.
3.2.1. How does health spending in Brazil compare internationally?
Brazil has high overall spending on health but the public share is low
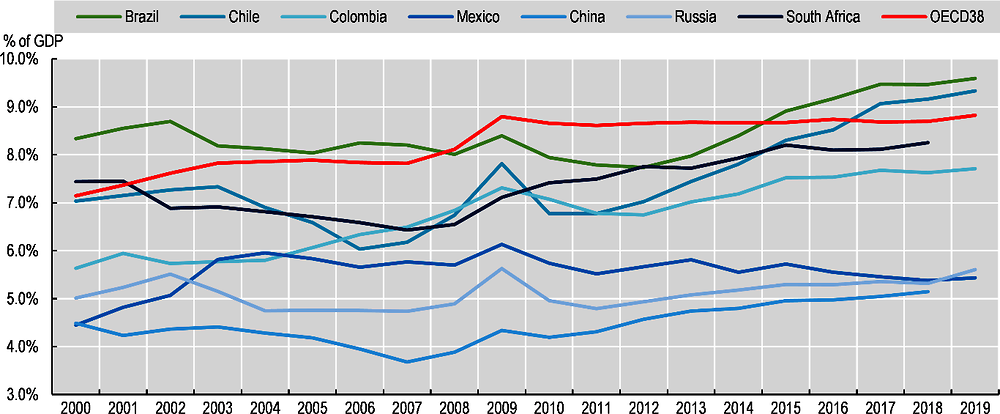
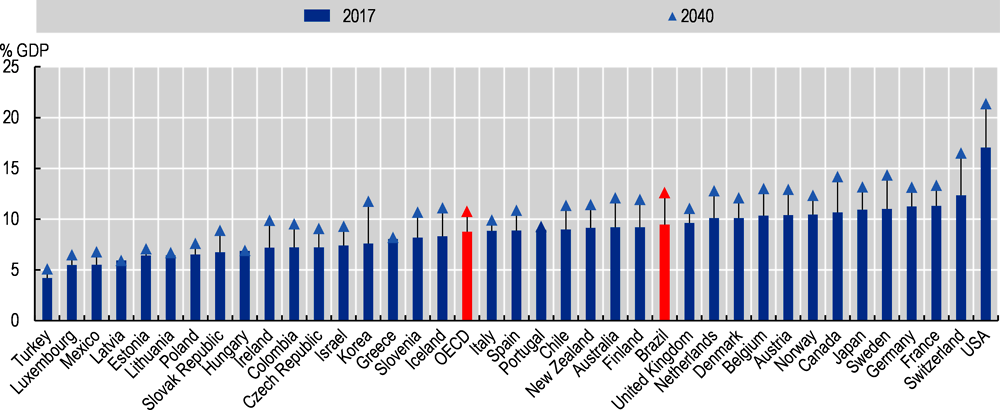
Health care in Brazil is financed by a wide range of actors with the public Sistema Único de Saúde (SUS), private health insurance schemes and direct payments by private household being by far the most important payers. In 2019, Brazil allocated 9.6% of its GDP to health care (corresponding to USD 1 514 per capita when adjusted for differences in purchasing power). This share has been growing since 2000, up from 8.3%. The total share is relatively high given Brazil’s state of economic development. It is above the values seen in Chile (9.3%), Colombia (7.7%) and Mexico (5.4%), and higher than in China and Russia (Figure 3.1). It stands also above the OECD average (8.8%). That being said, the United States (16.8%), and some Western European countries such as Switzerland, Germany and France (11-12%) still allocate a substantially greater part of their GDP to health care than Brazil.
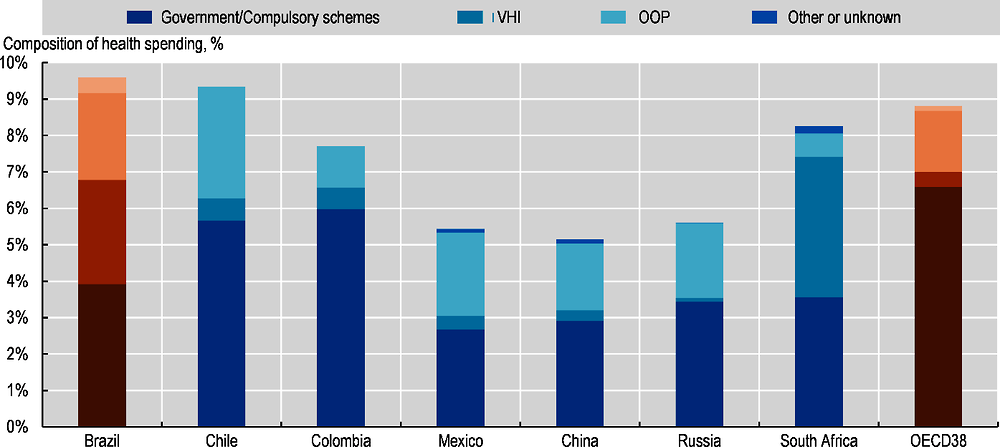
While Brazil spends more on health care than many peer countries overall, the country relies heavily on financing from the private sector, either via voluntary private health insurance or direct payments by households. In 2019, only 41% of all health spending was financed publicly1 (equivalent of 3.9% of GDP) – mainly via SUS, 30% by private health insurance (2.9% of GDP) and 25% referred to out-of-pocket payments (2.4% of GDP).2 While the spending share of private health insurance has increased significantly since 2000 (up from 1.7% of GDP), the share of public spending has grown only moderately (up from 3.5% in 2000). The proportion of household out-of-pocket spending in GDP (2.4% in 2019) is smaller than in 2000 (3.0%) but above the value seen in 2015 (2.2%), suggesting an increasing need by patients to finance health care good and services themselves in the most recent years.
In 2019, public spending on health as share of GDP in Brazil was on a similar level than in South Africa (3.6%), and higher than in Russia, China and Mexico (around 3%). However, it was below the proportions recorded in Colombia and Chile (5.7% and 6%, respectively). In most OECD countries, public health spending accounts for a significantly higher share of their GDP than in Brazil (Figure 3.2). In 2019, the average stood around 6.6% and was above 9% in France, Sweden, Germany and Japan. The share of voluntary private health insurance in GDP on the other hand is exceptionally high in Brazil, only topped by South Africa. Australia, Canada and Slovenia are OECD countries with important voluntary private health insurance markets where they account for shares between 1-1.5% of GDP.3 With a proportion of 25% out-of-pocket payments in total health spending,4 Brazil relies less on households’ ability to pay directly for health care goods and services than some other medium-income countries such as Chile (33%) or Mexico (42%), but much more than Colombia (15%). Financial protection is also much more comprehensive in the OECD as a whole – only 20% of all health spending originate directly from households.
Brazil spends less on inpatient care but more on outpatient care and administration than OECD countries
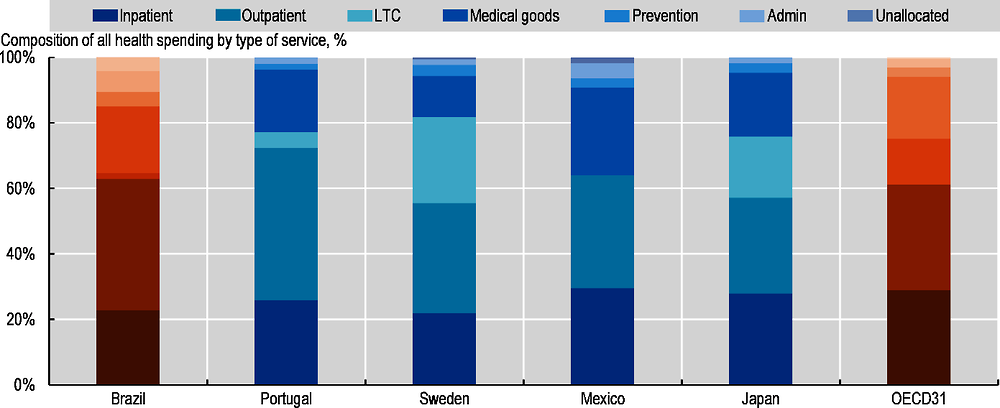
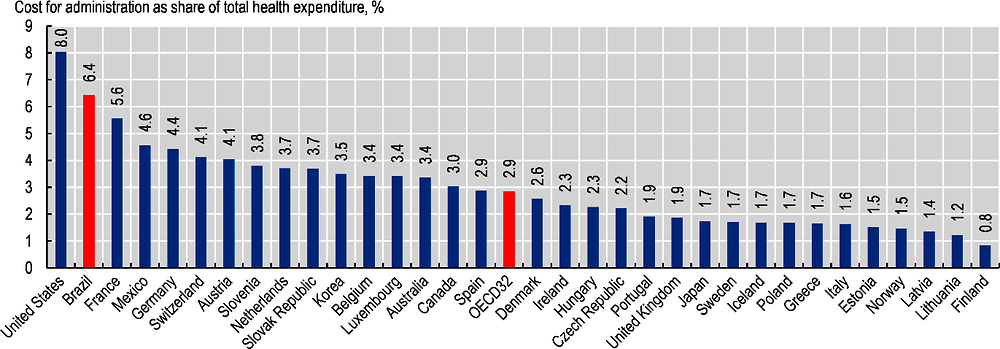
Analysing the composition of health spending from the perspective of the type of service reveals some particularities of the Brazilian health system. Such an analysis shows that Brazil allocates a lower proportion of health spending on inpatient care and long-term care and a higher proportion on outpatient care than on average across the OECD (Figure 3.3). The share of spending on administration (6% vs. 3%) is also higher than the OECD average. However, the fact that around 4% of health spending cannot be allocated to any service in Brazil affects the international comparability of these figures to a certain extent.
Public coverage of pharmaceutical costs in Brazil is much below the OECD average
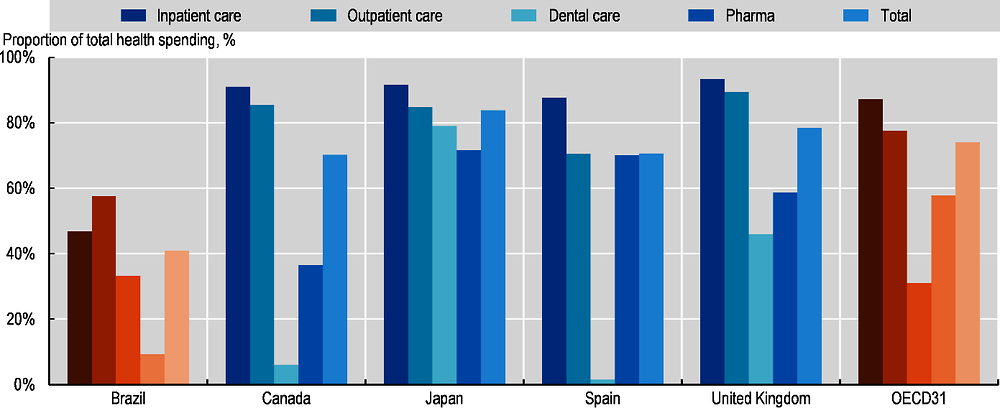
Combining information of payers of health care with the type of services can give an insight into the generosity of the publicly financed benefit basket of a country but also about public spending priorities. As to be expected, as a general rule, health services in Brazil are less comprehensively covered by public schemes than in most OECD countries (Figure 3.4). In Brazil, only around 47% of all inpatient costs are covered by public schemes compared to 58% for outpatient care. Across the OECD, public inpatient coverage is usually more comprehensive than for outpatient care (87% vs 78% on average). Brazil has a relatively high share of dental care costs covered (33%) – exceeding the OECD average (31%). On the other hand, only 9% of all retail pharmaceutical spending is financed by public schemes in Brazil. This share is far below any other OECD country (average 58%) and suggests a substantial gap in effective coverage.
3.2.2. How is health financing organised in Brazil?
A variety of financing schemes exist in Brazil that provide coverage against the costs of health care and access to services for all or some parts of the population. The public scheme under the organisation of SUS provides access to primary care, secondary care, medication and many other services, potentially for the entire population. Yet, although entitlement to services is universal, a good part of the population opts for not using SUS services and rely on private schemes (see Section 3.2.2). SUS is financed through a mix of revenues from the federal and state governments and municipalities that evolved over time. Among private schemes, voluntary private health insurance plans that predominantly duplicate coverage by SUS and gives access to a wider set of (mainly) private health providers is very popular in Brazil among particular population groups (see Section 3.2.2). In addition, charities and employers also provide access to health care, although typically limited in scope and target group. An important part of health spending remains financed directly by patients themselves out-of-pocket. Overall, the health financing arrangements in Brazil are complex.
Public scheme – Sistema Único de Saúde
The move towards universal health care coverage in Brazil began with the adoption of the Federal Constitution in 1988 stating that health care is a fundamental right and duty of the state and the subsequent establishment of the Sistema Único de Saúde (SUS) – the publicly funded health system. The key principles of SUS as laid out in Articles 196 to 198 of the constitution are universality, comprehensiveness, equity, decentralisation and social participation. Based on these principles, everyone in Brazil is entitled to comprehensive health services provided under SUS regardless of socio-economic circumstances or the ability to pay. The federation, the 26 states (plus the federal district) and the 5 570 municipalities have shared responsibilities for financing and management of SUS and the delivery of public services. The participation of the civil society in determining the strategic direction of SUS is enshrined in the constitution and is operationalised via regular health conferences and health councils on the federal, state and municipality level (see Chapter 2).
Services financed by SUS are delivered by a wide mix of private and public providers. In primary care, services are predominantly provided by publicly employed staff working in multi-disciplinary primary care teams. Outpatient specialist care is available in public clinics or hospital outpatient departments. Inpatient services are provided by public hospitals but private hospitals are also contracted by municipalities or states to provide services under SUS. In total, there are 345 000 health facilities registered in Brazil serving public and private patients.
The scope of health services offered under SUS is comprehensive without cost sharing for patients but there may be out-of-pocket payments for some prescribed pharmaceuticals obtained via the “farmacia popular” programme and for any other goods and services not included in the benefit package or obtained from providers outside the SUS network. While the entire population is entitled to receive services under the SUS, a non-negligible part of the population struggles with unmet health needs. Based on result of the Health Interview Survey 2019, nearly 14% of those who sought health care two weeks prior to the survey did not receive it (IBGE, 2020[3]). A particular problem is related to accessing specialist services resulting in long waiting times and unmet need (Castro et al., 2019[4]). A higher proportion (around 25%) forgo their right to treatment under SUS altogether and instead use private health insurance to obtain services or pay themselves. They mainly expect better access and higher quality from the private sector. However, for very costly and complex treatment such as organ transplant, HIV/AIDS treatment or access to high cost medication (not covered by private insurance) these patients frequently return to SUS to obtain these services.
The establishment and the roll-out of SUS is generally considered a success story in extending health care coverage to disadvantaged population groups that previously did not have access to health care services and SUS therefore contributes to reducing inequalities in access to care and improving health outcomes. Part of this was achieved by putting a focus on reorganisation and strengthening of primary care (Couttolenc and Dmytraczenko, 2013[5]). Yet, problems with care co-ordination, low quality of services and inefficiencies are frequently mentioned in the context of SUS (Couttolenc and Dmytraczenko, 2013[5]).
Private scheme – private health insurance
In 2020, around 22% of Brazilians (47 million) were covered by voluntary medical insurance to mainly duplicate health care coverage5 under the SUS, down from 25% in 2014 (Agência Nacional de Saúde Suplementar, 2020[6]). More than 700 entities and insurers offer this type of coverage (Agência Nacional de Saúde Suplementar, 2020[6]). There is a wide variety in the scope of services covered by the individual plans and in the legal modalities of the entities covering these services. Most cover ambulatory and hospital care but not pharmaceuticals or highly specialised treatment. In addition, more than 26 million Brazilians are covered by exclusively dental insurance plans6 which duplicate and supplement SUS coverage, a figure that nearly doubled in the last 10 years (Agência Nacional de Saúde Suplementar, 2020[6]).
Most health plans are employer-based group policies as a component of employment contracts where contributions are paid by employers but other individual or collective policies are also available. An important feature of the Brazilian private insurance system is that contributions are deductible from personal income subject to taxation,7 meaning that people with high income have a higher net tax gain. This is one of the reasons why the uptake of voluntary health insurance is much more prominent among richer population groups (Montaya Diaz and Sarti, 2020[7]). People with private coverage usually access private health providers including for profit and not-for-profit hospitals.
3.2.3. How sustainable is health spending in Brazil?
Similar to the situation in OECD countries, the health system in Brazil faces a number of challenges that can affect the sustainability of health care spending in the future. Population ageing will increase the demand for health and long-term care, as ageing is associated with an increase in chronic conditions. Compared to most OECD countries, Brazil is projected to age more rapidly. By 2050, 21.9% of the population is expected to be 65 years or older, up from 8.9% in 2017 (OECD, 2019[8]). This is a hike by 13 percentage points; across the OECD, the increase will only be around 10 percentage points, reaching 27% by the mid of the century. Growth in chronic conditions will also be exacerbated by rising obesity rates, physical inactivity of adults and children, and other unhealthy lifestyles which are already widespread in Brazil (see Chapter 5 and Chapter 6). Moreover, the rise in incomes increases population’s expectations, which puts an upward pressure on health spending, as does the technological progress. This will be amplified by reduced productivity gains in the health sector compared to other parts of the economy (the so-called “Baumol-effect”).
Health spending in Brazil is projected to increase substantially until 2040
Without taking into account any structural breaks due to COVID-19, the OECD health spending projection model suggests that – in the base-line scenario – health spending in Brazil will increase to 12.6% of GDP by 2040 (Figure 3.5). Compared to 2017 this is an increase of more than 3 percentage points – more pronounced than in most OECD countries. On average across the OECD, 10.8% of economic wealth will be allocated to health in 2040, 2 percentage points more compared to 2017. The projected increase in Brazil is also stronger than in Chile or Colombia where health spending is expected to reach 11.4% and 9.5% of GDP in 2040, respectively.
Rising health spending can also be expected under more favourable scenarios in Brazil. In case some ‘cost control’ policies are implemented, the health-to-GDP ratio is projected to rise to 12.4% of GDP; in case of more ‘healthy ageing’, the increase can be limited to 11.7%. If additional ‘cost pressures’ will occur, health spending is expected to grow further, reaching 13.3% by 2040. Significant increases in health spending, albeit below the OECD estimates, are also projected in other research work based on alternative projection models. Rocha et al., for example, project health spending to reach 12.2% of GDP by 2045 in their baseline scenario (Rocha, Furtado and Spinola, 2019[9]).
In summary, the OECD health spending projection model has two key messages for Brazil:
the health spending to GDP ratio in Brazil will increase further, even under the most favourable scenario;8 and
the expected increase of this ratio will be higher in Brazil than in most OECD countries.
In light of these findings, there are basically four possible options (that could also be used in combination) to address the increasing health financing needs in Brazil, and they will be discussed in detail in the following subsections:
Increasing public health spending without compensation from lower spending elsewhere, thus raising total government spending (Section 3.3.1).
Prioritise health spending within the existing overall government spending envelope (Section 3.3.2).
Rely more on private spending (Section 3.4).
Find efficiency gains in the health sector (Section 3.5).
3.3.1. Brazil has limited fiscal space to substantially increase total government spending
The recent development of public spending on health in Brazil -but also total public spending more broadly needs to be seen in the context of the challenging economic and fiscal situation of the country in the last decade.9 After overall strong economic performance in the first decade of the millennium, GDP growth started to slow down in 2012, followed by a deep recession in 2015 (-3.5%) and 2016 (-3.3%). This also affected the fiscal position of the country and led to a substantial increase of the government debt-to-GDP ratio. It stood at 76% in 2019, and closed the year 2020 at 90% as a result of the different measures taken to tackle the health and economic impact of COVID-19 (OECD, 2020[11]). The debt ratio is expected to increase further in the mid-term unless an ambitious structural reform package is implemented (OECD, 2020[11]).
In addition, the level of public spending in Brazil (41% of GDP in 2019) is around the OECD average (40%) but much higher than in countries with a comparable level of development. In Chile (26%) and Mexico (27%) but also India (29%) and China (34%), the shares are substantially below the value seen in Brazil (Figure 3.6). Over time, this proportion has increased until 2015 in Brazil, when it reached 43%. It has gone slightly down since.
When analysing the structure of public spending in Brazil, the most important categories are social benefits (accounting for 39%), followed by education, health and interest payments (OECD, 2020[11]). Social benefits have also been the spending area recording the highest increase since 2012. Besides that, a large array of tax expenditures in the form of tax exemptions, special regimes or special rates significantly reduce Brazil’s tax revenues.
Against this background, a number of initiatives have been taken by the federal government to improve fiscal outcomes, while stabilising and reducing public sector debts. A key element of this strategy was the adoption of an expenditure ceiling in 2016, limiting the growth of primary federal government expenditure to inflation. This overall budget ceiling also has also an impact on public health spending.
Frequent changes to the financing rules of SUS have been the norm since its inception and affect the delicate composition of funding from municipalities, states and the federation (Box 3.1). With the current mechanism in place (as defined by Constitutional Amendment 95, CA95), in 2017, the federal government financed around 43% of all SUS spending, the municipalities 31% and the states 26% (Vieira, Piola and de Sá e Benevides, 2019[12]). However, there is concern that the current mechanism is ill-suited to take account of future health spending needs and will result in a considerable shortfall of funding. For example, some research suggest that the implementation of CA95 could lead to a loss of an accumulated BRL 415 billion in federal financing for SUS over 20 years compared to the previously existing financing regime (Vieira and de Sá e Benevides, 2016[13]; Massuda et al., 2018[14]). The National Treasury also estimates that the projected health financing needs will, under different scenarios, outgrow the minimum federal spending floor which could potentially lead to problems of underfunding (Tesouro Nacional, 2018[15]). In an evaluation of what it takes to safeguard universal health coverage in Brazil by 2030, and taking into account health inflation and changes in the age structure of the population, the Federal Court of Accounts projects a significant funding deficit at the federal level in 2030 (Tribunal de Contas da União, 2020[16]).
As set out in the Federal Constitution of 1988, health is a responsibility of the state and services provided under the SUS are financed collectively by the federation, the states, municipalities and other sources. However, since its inception the financing of SUS was contested and a number of legal changes and constitutional amendments attempted to make the financing less volatile but other consideration also played a role. A number of researchers believe that SUS has been structurally underfunded from the beginning with the latest financing reforms aggravating the situation -particularly from the side of the federation (Massuda et al., 2018[14]; Castro et al., 2019[4]).
Initially, the Constitutional Act of Transitional Provision (ADCT) foresaw that at least 30% of the Social Security Budget should be allocated to health with the participation of states and municipality not being specified. However, this funding commitment by the federation was difficult to maintain throughout the 1990s. The Constitutional Amendment 29 of 2000 identified minimum “floors” for the federation, the states and the municipalities for the financing of SUS, which brought more funding stability. According to the CA29, the federation should dedicate at least its 1999 value increased by 5% in 2000, and after that annually adjusted with nominal GDP growth. The states and municipalities should dedicate at least 12% and 15%, respectively, out of their own revenues to health. The Constitutional Amendment 86 of 2015 changed the financing obligations of the federation again. Investment floors were tied to the Federal Current Net Revenues (RCL). The percentage of RCL allocated to health was supposed to gradually increase from 13.2% in 2016 to reach 15% in 2020. However, Constitutional Amendment 95 in 2016 introduced further changes due to fiscal pressures and generally froze primary federal expenditure until 2036. For health spending, the stipulations from CA95 meant moving the 15% minimum allocation from RCL forward to 2017 but pegging future annual increases of this minimum floor to inflation until 2036.
There was a wide variation in states fulfilling their commitments as laid out in CA29, with a number of them not meeting the 12% minimum floor in the years 2004 to 2012. After the introduction of Complementary Law 141/2012, which foresaw penalties for non-compliance, adherence went up. Due to increased decentralisation and demand pressure, in all states the municipalities complied with their minimum spending obligations in the years since 2004. In 2017, municipalities allocated on average 22.5% of their own revenues to health, substantially above the 15% minimum requirement (Vieira, Piola and de Sá e Benevides, 2019[12]).
Overall, the frequent changes in the financing mechanism led to a greater involvement of the states and municipalities in the financing of SUS over time. Between 1995 and 2015, the share of municipalities increased from 16% to 31% and the states’ share from 21% to 26%. Consequently, the proportion of SUS funded from the federation decreased from 63% to 43%. However, for all three levels of government, health spending increased in real terms, for municipalities by around 8% per year on average (Vieira, Piola and de Sá e Benevides, 2019[12]).
Sources: Piola and Diniz Barros (2016[17]), “O financiamento dos serviços de saúde no Brasil” http://bvsms.saude.gov.br/bvs/publicacoes/sistema_saude_brasil_organizacao_financiamento.pdf; Mendes and Funcia (2016[18]), “O SUS e seu financiamento”.
While one option to meet future health spending needs (as identified in Section 3.2.3) is to allow for an increase in overall public spending, this possibility seems less likely in the short and medium-term given the current fiscal challenges in Brazil and the need to continue the path of adjustments to ensure overall fiscal sustainability. The discussion mainly focuses on the federal government but it seems unlikely that the states or municipalities would be in a position to drastically increase their absolute spending for health to meet future funding needs.
3.3.2. There is potential to make health a higher priority in government spending
An alternative or complementary option to make more public funds available to meet future health spending needs is to give health spending a higher priority within total public spending, i.e. compensating rising health spending with cuts or efficiency gains elsewhere. Given the current economic climate in Brazil, this seems to be a more viable option than a general increase of public spending. Indeed, comparing health spending from public sources with total government expenditure suggests that Brazil devoted less of its public budget to health (10.5%) than most OECD countries in 2019, well below the average of 15.3% (Figure 3.7).
There appear to be at least four areas in particular where potential savings could be generated of which some could be reallocated to the funding of SUS:10 (i) reducing tax expenditures and ineffective subsidies; (ii) improving the effectiveness of social transfers, (iii) managing high payroll expenses and (iv) revisiting the preferential tax treatment of some particular actors in the health system.
The OECD Economic Survey of Brazil 2020 highlighted a number of areas for potential savings that would not prevent Brazil from attaining key policy objectives. Subsidies and tax expenditures have risen to 4.8% of GDP. A number of these, like the SME tax regime, the Manaus Free Zone or income tax exemptions for private health and education services could be reconsidered and adjusted. On the whole, a reduction of subsidies and tax expenditures on the order of 2% of GDP appears feasible.
Similarly, some social programmes in Brazil are not very well targeted or very costly with limited impact to reduce inequalities (OECD, 2020[11]). Better targeting could enhance the impact of the social benefit system while reducing spending. In this context, progress has been made to improve the sustainability of the pension system by raising the effective retirement age and making pensions more progressive. However, an important additional step to make pension payments -but also some other programmes such as survivor pension- more sustainable would be to change their indexation rule, away from the development of the minimum wage, which has increased much more rapidly than real per capita income. Interestingly, these benefits – unlike the social transfers programme “Bolsa Familia”, which does not have automatic adjustments – predominantly benefit people who are not poor. As a consequence, readjusting the mechanism of calculating some social benefits could be achieved without being detrimental to disadvantaged population groups.
A second issue where substantial savings for the public purse could be generated is related to public employment. International comparison suggests that public sector staff costs are extremely high and that substantial wage premiums exist for federal employees compared to the private sector (OECD, 2020[11]). Moreover, public salaries have outgrown earnings in the private sector recently. Changing annual salary adjustment rules and revising entry salaries could generate much needed fiscal space to strengthen public health spending. The potential savings of managing the high payroll expenses could be in the area of 2% of GDP.
Finally, an issue that is more directly related to health is the preferential tax treatment of certain expenses of some actors in health sector. This refers for example to tax deductibility of private health insurance premiums and direct out-of-pocket expenses for health care services, as well as to tax exemptions for some health care providers and other instruments.
In total, the tax expenses in the area of health were estimated at BRL 41.3 billion in 2019 (Receita Federal, 2018[19]), representing 13.5% of all forgone taxes or 0.6% of GDP. Among all waived taxes in health, medical expenses and insurance premium for individual health care plans that can be deducted from incomes subject to personal income taxation (IPRF) accounted for more than one-third (BRL 15.5 billion), tax savings from corporate income tax (IPRJ) –for the purchase of health insurance by employers – for around BRL 5.6 billion. Important tax exemptions also related to non-profit health organisations (BRL 3.6 billion) that have exemptions from corporate income taxation (IPRJ) and federal social contribution levied on business revenue (COFINS) -and from social security contributions (BRL 6.8 billion), under the conditions that they provide at least 60% of their activity for SUS. Finally, the production and sale of selected pharmaceuticals (identified through a positive list) is exempted from COFINS and PIS (contribution to unemployment insurance). Together, they account for tax savings of BRL 6.7 billion. Taken together, the sum of all tax expenditure in health equated roughly with one-third of the entire federal budget for SUS in 2019.
The personal income tax exemptions are highly regressive as they depend on the individual tax rate. Moreover, 90% of Brazilians have incomes below the threshold where they would pay income taxes and only around one-quarter of Brazilians are subscribed to private health plans, while most of the population relies on the public health system. In 2017, medical expenses of around BRL 70 billion were declared. Out of the BRL 12.8 billion resulting tax savings, 75% benefited people in the highest income tax bracket of 27.5% (Tesouro Nacional, 2018[15]). In the Brazilian context, it is important to understand that there is no legal ceiling for tax deductibility of medical expenses. Moreover, with some few exceptions (e.g. medication), all health expenses including cosmetic surgeries carried out outside of the country qualify for deductibility. This is exceptional, even in Brazil. For other non-health expenses, such as for education, deductibility ceilings exist.
While preferential tax treatments of health care goods and services also exist in OECD countries, the extent to which they are used in Brazil seems remarkable in terms of volume and raises questions about their appropriateness. Phasing out the tax deductibility for health expenses and insurance premiums from personal income taxation for individuals alone would provide fiscal space in the area of 0.2% of GDP. The tax advantages for non-profit health providers (which also includes ‘social organisations” managing public facilities) also seem abundant. Health providers can gain non-profit status and profit from the ample tax advantages if they commit to dedicate 60% of their activity to SUS patients. Reviewing some of these advantages and carefully assess whether they improve efficiency in service provision could also be an option. While preferential tax treatment in the area of health service provision exist in many OECD countries (e.g. health services are exempted from value-added tax; reduced value-added tax for pharmaceuticals), exempting non-profit providers from social security contributions for their employees seems exceptional.
In case no additional or insufficient public funding can be generated to finance projected future health spending growth, the fallback option is to rely on private financing – either via private health insurance or directly by households as out-of-pocket payments. That being said, the share of private financing in Brazil is relatively high already (see Section 3.2) and any future increases may exacerbate already existing inequalities in the country. The share of voluntary private health insurance in total health spending stood at 30% in Brazil in 2019, much higher than the OECD average (5%) and far higher than any other OECD country.11 The proportion borne directly by patients out-of-pocket in Brazil (25%) is also above the OECD average (20%), but below values seen in Chile (33%), Greece (35%) or Mexico (42%).
3.4.1. The market for private health insurance is already very developed and has equity implications
Private health insurance predates the establishment of SUS, and the federal constitution of 1988 guarantees that private health insurance coverage can supplement automatic coverage under SUS.
The private health insurance market is well established and developed in Brazil. In September 2020, 47 million Brazilians had private medical coverage or “assistência médica” (22% of the population) and 26 million were covered by additional dental coverage.12 There is a wide variation of medical insurance plans depending on the types of services covered (e.g. “hospital and ambulatory”, “hospital only”, “reference”) as well as on the type of contract (e.g. “group insurance” via employer, “individual/family contract”). In addition, many different types of entities can offer private insurance coverage; this includes non-profit medical co-operatives, employers in the form of “autogestão” self-management, philanthropic organisations, networks of health providers or “medicina de grupo”, and health insurance companies. In 2019, 711 entities with beneficiaries were offering more than 36 000 plans for medical coverage in Brazil (Agência Nacional de Saúde Suplementar, 2020[6]). This means that the insurance market is very fragmented with many small operators: 6% of insurance entities cover 50% of insurance holders and more than 2/3 of all entities cover only 10% of beneficiaries (Agência Nacional de Saúde Suplementar, 2020[6]).
While coverage of private health insurance has been increasing over the last decades, it is correlated to the economic cycles with the number of beneficiaries going down during the last recession. Coverage is also unevenly distributed throughout the country. Rates are much higher in the more affluent states of the South-Eastern region (35%) than in the poorer Northern region (11%) (Agência Nacional de Saúde Suplementar, 2019[20]). In addition, a notable urban-rural divide in private insurance coverage can be observed in all states. Moreover, the health insurance market is characterised by very strong socio-economic inequalities in the uptake of private health insurance. In 2013, 64.7% of people in the highest income quintile had private coverage compared to only 5.5% among the poor (Montaya Diaz and Sarti, 2020[7]).
There seem to be at least three reasons why the share of people with private health insurance coverage has grown since the inception of SUS and is particularly prominent among the middle class and the well-off. Firstly, assumed lack of quality in the public SUS network also as a results of rapid expansion in the early 1990s and subsequent underinvestment. Secondly, a historical tradition of purchasing services on the private market as part of employment contracts and thirdly, the tax deductibility of private insurance premiums (Piola and Diniz Barros, 2016[17]).
Overall, the Brazilian private health insurance market is different from those in OECD countries with similar health system characteristics, in particular those with universal residence-based entitlements mainly financed via taxation. In countries like the United Kingdom, Australia, Ireland, New Zealand or Spain duplicate private coverage is also popular but appears to be much more limited to particular services with private providers, in particular for choosing inpatient and outpatient services in private hospitals. However, while the shares of population coverage are similar to those seen in Brazil, this sector is, from a financing perspective, much less important in those countries (Figure 3.8). Most likely, this reflects the fact that people with voluntary PHI coverage generally use public services and only resort to private insurance for a very narrow band of (hospital) activities. The case of Brazil seems exceptional in the sense that a quarter of the population broadly forgo their constitutional right to seek free public health care.
Consequently, the market for private health insurance is already more developed in Brazil than in most OECD countries. Without changing the current configurations of this market, a further extension of private insurance coverage does not seem to be desirable from an equity perspective. A further uptake in private coverage -or a further extension of the benefit packages leading to higher premiums- can represent an ‘additional drain’ of scarce public funds resulting in rising inequalities unless tax exemptions policies are changed. It is also unclear whether more spending on private coverage would contribute to improving efficiency and health system performance overall as high private coverage can lead to overutilisation of costly procedures and exams. For example, in 2019 the number of magnetic resonance imaging exams (MRI) per privately insured person in Brazil (179 per 1 000) (Agência Nacional de Saúde Suplementar, 2021[8]) was 2.3 times higher than that average MRI per population in the OECD (79 per 1 000) and considerably above the rate of Austria (148 per 1 000), which was the highest in the OECD in that year.
3.4.2. Further increase in out-of-pocket spending can lead to an increase in number of people experiencing financial hardship
A final possibility to meet projected health spending increases would be to leave more financing responsibilities to private households. In fact, this is the fallback option if no other funding alternatives are found. As seen before, the level of out-of-pocket spending as a share of total health spending in Brazil (25%) is above the OECD average (20%) but lower than in some OECD countries and many other countries in the Latin American region. Yet as a share of GDP (2.4%), direct payments from households are comparably high in Brazil. When analysing the composition of out-of-pocket payments, it can be seen that two-thirds of all direct spending is related to the costs of pharmaceuticals in Brazil. Compared to OECD countries, this is a very high share and signals lack of effective coverage in this area.
The structure of out-of-pocket spending in Brazil can be explained by the nature of the benefit package in SUS and other system characteristics. SUS offers, implicitly, a comprehensive benefit package in primary care, hospital care and other services, which does not require any cost sharing. For pharmaceuticals, a positives list of essential medicines has been defined which are available free of charge or with some limited co-payments under certain conditions. However, these may not be available when needed and patients may have to resort to self-paying medicines. Moreover, private health insurance contracts exclude outpatient pharmaceuticals, which require those people that forgo SUS coverage to pay for these goods themselves. In addition, beyond pharmaceuticals, SUS coverage excludes a number of private providers that may be contacted by patients for quicker access.
The problem with high overall out-of-pocket costs is that they, in general, affect poor and disadvantaged population groups more than others (WHO Regional Office for Europe, 2019[21]). For these groups, high direct costs for health care goods and services are more likely to represent a financial burden. For this reason, the United Nations decided to measure progress towards universal health coverage by monitoring the incidence of households that experience “catastrophic” health expenditure as an indicator for financial protection (WHO and World Bank, 2019[22]).
Data included in the financial protection monitoring report of WHO and World Bank suggest that financial hardship due to health care costs is an issue in Brazil (WHO and World Bank, 2019[22]). In 2008, 25.6% of Brazilian households reported that health care costs represented more than a tenth of total household consumption/income and 3.5% reported that it represented a quarter of total consumption/income; these shares were much higher than in nearly all OECD countries and above the average of the Latin American region. However, other studies have found that catastrophic health spending in Brazil was not more problematic compared to other Latin American countries (Roa, 2016[23]). Yet, regardless of the exact proportion of households facing catastrophic health spending, the strong correlation between the overall level of out-of-pocket spending in a country and the proportion of household experiencing financial hardship has been widely established (WHO Regional Office for Europe, 2019[21]). Hence, a policy decision that leads to an increase in cost sharing or decrease in coverage will most likely raise the percentage of the population facing financial hardship as a result, especially among the poor. Alternatively, it may also lead to an increase in delayed or forgone care if people are no longer able to afford services (WHO Regional Office for Europe, 2019[21]).
Therefore, from an equity perspective, letting people bear more health care costs themselves will eventually lead to a further worsening of health inequalities in a country that is already facing serious inequality issues. There are also questions to what extent increasing out-of-pocket spending is efficient. In many instances, private providers charge higher prices for the same services that are provided publicly without a clear difference in quality. For this reason, a deliberate increase in the share of health spending financed out-of-pocket does not seem to be a desirable option.
A final possibility to address the projected increase in health spending is to generate efficiency gains and reduce wasteful spending within the health sector. Getting “more value for money” could soften the emerging spending pressures by making sure the right intervention is carried out in the right setting, by using the most cost-effective and evidence-based input mix to treat diseases and by limiting the diversion of financial resources in the health system that are not used for promotion of health, prevention of diseases and the treatment of patients. Across the globe, around 20% of health spending can be considered “wasteful” in the sense that if some services accounting for these costs would not occur, it would make no difference to health outcomes of patients (OECD, 2017[24]).
3.5.1. The Brazilian health system is widely perceived as being inefficient
Previous work in comparing potential for efficiency gains internationally has found that there is a particular scope for improvement in Brazil. Quantifying possible gains in health-adjusted life expectancy using data envelopment analysis techniques based on data by World Bank and WHO, the OECD Economic Survey of Brazil 2015 found that more than five years of life expectancy could be gained through efficiency improvement while maintaining current per-capita health expenditure (OECD, 2015[25]). This was more than in any OECD country. The potential for efficiency gains in the Brazilian health system has also been analysed in other studies. The World Bank, for example, estimated total potential savings of around 0.62% of GDP until 2026 in five distinct areas of health with either neutral or positive effects on equity (World Bank, 2017[26]). In calculating the spending requirements needed to reach the Sustainable Development Goals (SDGs), Flamini and Soto estimate that the health sector has room for savings of up to 2.5% of GDP by 2030 through higher spending efficiency without compromising quality (Flamini and Soto, 2019[27]).
Improving efficiency and performance are important health system goals and they have been included in initiatives of recent and current administrations in Brazil. In this context, the current multi-annual Health Plan (“Plano Nacional des Saúde 2020-23”) highlights, for example, the need to improve contracting of public service to raise efficiency in the management of SUS, a better integration of primary and secondary care, enhanced co-operation on a regional level, or a wider application of electronic tools. Previous initiatives preceded this, such as the introduction of Health Technology Assessment (HTA) in SUS and the creation of the National Commission for the Incorporation of Technologies in the Unified Health System (CONITEC) in 2011. The introduction of financial incentives to improve access to service as part of the “Previne Brasil” strategy was also geared to raise health system performance.
3.5.2. OECD has developed a framework to discuss wasteful spending across the entire health system
These initiatives and ambitions notwithstanding, there is still the perception that more can be done to find better value for money. In Brazil, as well as in all other countries, inefficiencies can be found in every aspect of the health system and the OECD has developed a comprehensive framework to systematically analyse potential sources of inefficiencies, its drivers and root causes, and discusses what can be done about it (OECD, 2017[24]). Wasteful clinical care covers instances when patients do not receive the right care, for example inappropriate or low value care. It also includes preventable clinical adverse events. Operational waste occurs when care could be produced using fewer resources within the system while maintaining the benefits. Examples include situations where lower prices could be obtained for the inputs purchased, or where costly inputs are used instead of less expensive ones with no benefit to the patient. Governance-related waste pertains to the use of resources that do not directly contribute to patient care, either because they are meant to support the administration and management of the health care system and its various components, or because they are diverted from their intended purpose through fraud, abuse and corruption. This basic framework will also be used in the subsequent assessment of potential sources of inefficiency in Brazil (Figure 3.9).
Typically, all actors of the health system contribute to wasteful spending but the degrees differ. Not satisfied with the outcome, patients may ask for redundant repeat examination. Clinicians may choose an unnecessary costly treatment procedure even if a cheaper alternative exist. System managers may contract service providers at a higher price than necessary and the regulator may be responsible for ineffective and costly administrative hurdles in health delivery planning.
The remaining part of this section will identify some areas of potentially wasteful spending and efficiency gains in Brazil across the entire health system, including primary health care, secondary and hospital care, pharmaceuticals, long-term care, and administration and governance.
3.5.3. Primary health care is a key component of SUS, but it still does not deliver its full potential
The introduction of SUS has been accompanied by several initiatives to strengthen primary health care
Since its inception, a strong focus of SUS was to strengthen the role of primary health care and move away from a health system that was historically very hospital-centred. In 1994, the Family Health programme was established which set standards on the composition of teams of health care professionals including general physicians, nurses, nurse assistants and community health workers providing a wide range of services, such as acute care, health promotion, chronic disease management and maternal and child health care (Castro et al., 2019[4]). These teams became the key element of primary health care in SUS but problems with staffing slowed down the expansion of this care model. To address problems in access, especially in rural areas, the “Mais Médicos” programme was adopted in 2013, which led to the temporary recruitment of around 18 000 additional doctors, mainly from abroad. While being successful in increasing access to primary health care in some disadvantaged areas (Gonçalves et al., 2019[28]), the programme is currently phased out and is replaced by the “Médicos pelo Brasil” programme. This initiative seeks to centralise recruitment for doctors for disadvantaged communities and to strengthen the professional development opportunities of these newly hired doctors.
A strategy to improve efficiency in primary health care and expand access was the ‘Previne Brasil’ initiative introduced in 2020. This initiative marked an important shift in the calculation method how federal funds are transferred to the municipalities to purchase primary care services but also increased overall federal resources for primary health care. Under SUS, the federal government has financed roughly one-third of total primary health care costs, with the remaining part being funded predominantly by municipalities (61%) (Ministério da Saúde/Fundação Oswaldo Cruz, 2018[29]).13 Prior to the ‘Previne Brasil’ strategy, the federal transfers to municipalities were composed of a fixed and variable capitation component, a voluntary pay-for-performance bonus based on the National Programme for Improving Primary Care Access and Quality (PMAQ) and payments for the direct provision of services through community health workers and “Mais Médicos” programme. The ‘Previne Brasil’ strategy recalibrated the capitation payments to better take account of differences in health care needs across municipalities, streamlined the pay-for-performance indicators and revisited the strategic actions to be financed by the federation (OECD, 2021[30]). An important change in ‘Previne Brasil’ is that capitation payments are only made for people registered with Family Health Teams which should incentivise municipalities to further engage in this delivery form. While it is too early to conduct an overall evaluation of this programme, the number of people registered with Family Health Teams has increased substantially, reaching 127 million by November 2020 (OECD, 2021[31]).
Analysing the composition of overall health spending in an international context, can help assessing whether a country makes spending on primary health care a priority. In 2019, Brazil dedicated around 16% of its financial resources to “basic health care services” – defined as general outpatient care, dental care, home-based curative care and preventive activities,14 a share similar to the OECD average (Figure 3.10).
Despite these achievements, performance of primary health care can be further strengthened
Comparing efficiency levels in primary care across municipalities in Brazil, the World Bank identifies possible efficiency gains of 37% (World Bank, 2017[26]). There is hence significant potential to expand service provision using the same amount of resources. Other issues that should be addressed include limited service accessibility and shortcomings in the co-ordination between primary and secondary care.
Lack of availability of doctors can lead to unmet needs and the 2019 Health Interview Survey has shed some light on this. In 2019, around 14% of all Brazilians who sought health care in the two weeks prior to the survey did not receive it (IBGE, 2020[3]). Particularly relevant for primary care is the fact that 21% of all Brazilians with diagnosed diabetes did not received medical care in the 12 months prior to the survey (IBGE, 2020[32]). Interestingly, while there is little statistical variation for unmet need of this kind across states, rurality or income (IBGE, 2020[33]), differences in quality of care appear to exist. Diabetic patients have a higher likelihood of complications (as measured in hospitalisations) in the North-East than in the South-East and this probability is systematically higher for those where household income is at the minimum wage or below than those with more than three times minimum wage (IBGE, 2020[34]).
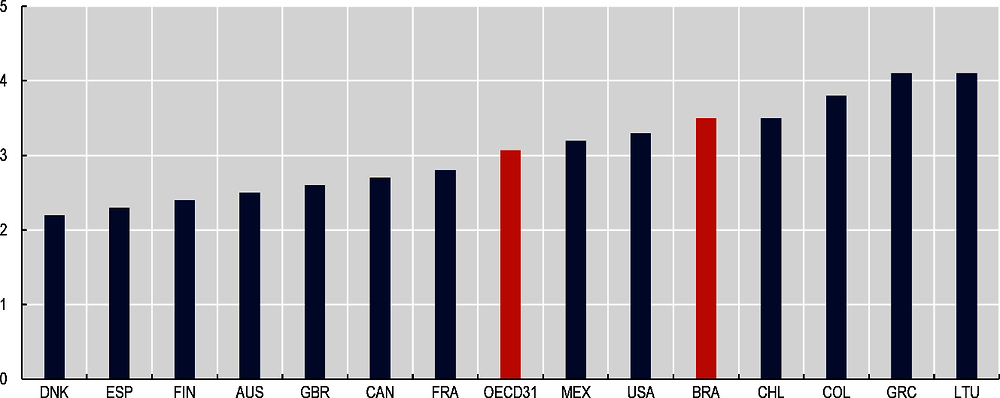
Some of this unmet need will be related to the availability of doctors. While substantially increasing over the last decades, the number of doctors in Brazil is still lagging behind the OECD average. In 2017, around 2.2 physicians per 1 000 population were registered in Brazil (Scheffer and al., 2018[35]). This compares with 3.5 practicing physicians15 across the OECD (OECD, 2019[8]). Similar to most OECD countries, there is a wide geographic disparity in the availability of physicians in Brazil, also reflecting socio-economic differences. In municipalities with less than 5 000 inhabitants, the overall physician density is only 0.3 on average; for municipalities with more than 500 000 inhabitants the ratio stands at 4.3 (Scheffer and al., 2018[35]). Because specialists are more likely to practice in agglomerations, the unbalanced spatial distribution of health professionals is somewhat less pronounced when looking at generalists (i.e. registered doctors without specialisation) only. Nevertheless, significant differences still exit. On a state level, the generalist per 1 000 population ratio ranges from 0.4 in Maranhão in the North-Eastern region to 1.6 in Rio de Janeiro. A high geographical variation of health professionals can suggest an inefficient allocation of resources leading to unmet need and a lower quality of care in underserved regions and to overprovision of services in other parts of the country.
Experience from OECD countries informs that different strategies help redress the geographical imbalance of doctors (OECD, 2016[36]). A first approach tries to address the issue in the long-run by targeting future doctors during their medical education. This can be done by providing scholarships or preferred access to students who commit to practice in rural areas or communities for a defined period of time after graduation, as is the case of Australia, Japan, Canada, England and Chile (OECD, 2021[31]). For current professionals, there is a “stick and carrot” approach. Many OECD countries use financial incentives, either one-off or wage-related, to attract physicians to practice in rural or disadvantaged areas. In Canada and Denmark, some of these policies are in place. On the other hand, a few countries, including Germany, some provinces in Canada and Norway, restrict the place where doctors can practice. In Germany, self-employed doctors are not allowed to set up their practice and serve public patients in a catchment area that is considered ‘overserved’ based on a patient-to-doctor ratio. At any rate, addressing the regional imbalance of doctors, in particular for general practitioners, requires careful and coherent workforce planning. On a national level, this has so far been largely absent in Brazil (OECD, 2021[31]).
There could be potential to get more primary health care activity with existing resources
Interestingly, the substantial increase in the number of doctors in Brazil did not necessarily translate in a commensurate increase in primary care activity under SUS. The ratio of annual consultations for primary care registered under SUS divided by the total population stood at 2.2 in 2019, up from 2.0 in 2000 but below the value of 2014 (2.8)16 (Ministry of Health, 2020). While this figure should not be confused with the average number of consultations per person, the fact that this ratio increased by only 10% over the last two decades while the number of doctors grew by more than 50% should be analysed in more detail. It could mean that many newly graduated doctors do not want to pursue a career in primary care but it could signal some inefficiencies in care provision.
One issue that may explain the reduced growth in primary care consultation and associated problems in accessing SUS services17 is the wide-spread use of ‘dual practice’ which means that many physicians split their time between public and private patients. Recent regulation in Brazil prohibits doctors to have more than two jobs in the public sector, however, there is still the option to take on additional tasks in the lucrative private sector. A recent study finds that 51% of all doctors in Brazil work under dual-practice arrangements, 27% only in the private sector and only 22% exclusively in SUS (Miotto et al., 2018[37]). It also shows that those working solely in the public sector tend to be younger, less experienced and more likely to earn less than those in the private sector or in dual practice. Dual practice is also common in many OECD countries and can create problems to reduce service access of public patients if not properly regulated and monitored (Mueller and Socha-Dietrich, 2020[38]). Countries that have recently taken measures to increase physician’s time to treat public patients include Ireland and Israel. Part of their strategies include a pay raise for public doctors that forgo the option to work in the private sector.
A consequence of wide-spread application of dual practice can be absenteeism of doctors during regular working hours from their public jobs (Socha and Bech, 2011[39]). Recent research suggests that this may be an issue in Brazil. Analysing time use of 47 physicians working across 27 Family Health Teams in 12 municipalities indicate that they are absent from work during shifts in around a third of the time on average (dos Sanots Matsumoto, 2018[40]). This phenomenon is also a concern in some OECD countries but literature on this topic mentions the difficulty to clearly disentangle dual practice from poor overall management as the source of absenteeism (Socha and Bech, 2011[39]). That said, whether publically employed doctors perform their contractual work duties is clearly something that should be monitored closely. More analysis is needed to assess whether this is a common phenomenon in Brazil. If it is, the implementation of consistent monitoring tools could be an instrument to improve output and system performance.
Primary health care is still fragmented and problems in co-ordination of care across service levels persist
The latest Health Information Survey highlights the fragmentation of primary health care delivery. For example, around 50% of the diabetic population identified basic health units (‘unidade básica de saúde’) as their last contact to the health system, 11% used public speciality units in hospitals, 6% public urgent care units and 30% private practices or clinics (IBGE, 2020[32]). There is a clear socio-economic gradient to this: While basic health units were the most recent provider of diabetes care for around 60% or more of people from poorer household, these facilities are key health providers for only 15% or less of rich households (IBGE, 2020[41]). Difference in primary health care utilisation patterns and patient experience among elderly Brazilians was found in recent research (Macinko et al., 2018[42]). Those with private health plans (not using SUS) report fewer problems in terms of access, care co-ordination, continuity of care and provider co-ordination than those using SUS-Family Health Teams. Most problems are encountered by patients who use SUS but do not consult Family Health Teams.
The latter examples show that despite ongoing progress to further the roll-out of the Family Health Strategy, many Brazilians still use other providers as their regular point of care for chronic conditions. On the one hand, most people with private health insurance coverage do not use SUS at all and resort to private practices. Yet even for those without private coverage, a good part of them use public speciality units or emergency departments for provision of chronic services. This is inefficient since these types of conditions are best treated in primary care settings (OECD, 2020[43]). To further promote the Family Health Strategy more financial support may be needed, in particular in disadvantaged rural areas. In addition, out-of-hours options for primary care units should be further elaborated as in the “Saúde na Hora” programme, so that people with acute conditions do not need to resort to emergency care units. Moreover, cancer screening and preventive activities such as health check-ups should receive greater attention within primary care (OECD, 2021[31]). These are “good value for money” as these interventions reduce more costly treatment later.
In several OECD countries (including, for example, Chile, Portugal, Italy or Norway), strong gatekeeping systems are seen as a way to ensure that patients receive the best possible care for their conditions and to achieve greater appropriateness and co-ordination of care (OECD, 2020[43]). Further development of primary health care in Brazil could also entail to give GPs a stronger ‘gatekeeping’ role whereby they control and orient the patient’s entry into secondary care. This implies that patients have to register with primary care physician or practices and GPs control access to secondary care with a referral system.
Related to ‘gate-keeping’ is the need to strengthen the co-ordination of care across the health systems, also to address the long waiting times for visits to specialists or diagnostics. Historically, co-ordination between different care levels has been relatively weak in Brazil. To address these issues, the Federal Ministry of Health has established guidelines for the organisation of thematic Health Care Networks (“Redes de Atenção à Saúde – RAS”) in 2010 within the scope of SUS. This initiative seeks to integrate service provision through technical, logistical and management support across primary, secondary and tertiary care as well as ancillary services. At the moment, networks exist for prenatal care and childbirth, urgent care and emergencies, psychosocial care, for people with disabilities, and for people with chronic conditions, but the centrality of primary care in these networks is unclear.
Integrated care models can be successful in improving continuity of care leading to better outcomes but require information sharing across care levels and evidence based care pathways. However, the thematic integrated care network operate within the complex and rigid existing SUS planning and management environment and funding principles. This could be a barrier to a successful roll-out of health care network. Within the OECD, countries have embarked on different pathways to operationalise the integration of care (OECD, 2016[44]). In the United States and Germany, for example, providers joined into “Accountable Care Organisation” (ACO) where they are collectively responsible for patients in a defined catchment area. These ACO receive a virtual budget for a wide range of services and they are incentivised by shared savings contracts with payers to co-ordinate care across different levels efficiently. They can keep part of the savings if they keep total costs below the virtual budget if they meet pre-defined quality criteria. Other good examples for care integration exist in the Basque country of Spain and as primary health care networks in the United Kingdom (OECD, 2021[31]).
3.5.4. Inefficiencies persist in outpatient specialist and hospital care
The Brazilian hospital sector has a lot of excess capacity in normal times but distribution is uneven
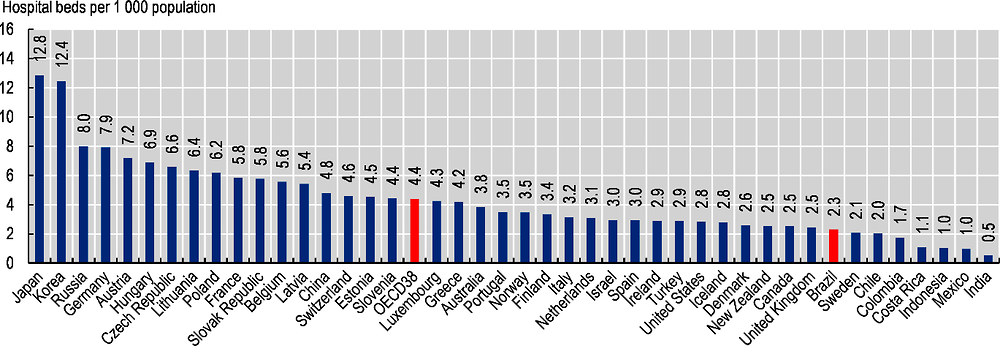
Overall, Brazil had approximately 474 000 hospital beds in 2019, around the value seen in 2007 but down from 501 000 in 2010. This equates with 2.3 beds per 1 000 population, around half of the OECD average (Figure 3.11). Nevertheless, the bed density is similar to some European countries such as Denmark (2.6), the United Kingdom (2.5) and Sweden (2.1) and above other countries in Latin America, such as Chile (2.0), Colombia (1.7) or Costa Rica (1.1). As in many OECD countries, in Brazil, too, there is some variation in bed availability within the country. On a state level, the density of hospital beds varies by a factor of 2, ranging between 1.5 beds per 1 000 population in the Northern state of Amapá and 2.9 beds in the Southern state of Rio Grande do Sul (Brazilian Ministry of Health, 2020).
An important difference between Brazil and OECD countries appears to be the level of activity. In 2019, there were 58 hospital discharges per 1 000 inhabitants in Brazil (Brazilian Ministry of Health, 2020), about one-third of the activity levels seen across the OECD and only one-fifth of the hospitalisation rate seen in Germany or Austria. The low number in Brazil also reflects the fact that the country has a relatively young population. Yet, there are more discharges per population in Brazil than in Colombia or Mexico.
As a result of the very low inpatient activity, the occupancy rate of hospital beds in Brazil is far below all OECD countries highlighting a lot of excess capacity in normal times (not considering peaks in demand associated with the COVID-19 pandemic). Only around 52% of hospital beds were used on average for treatment at any given day in 2019. This share has been slowly increasing recently but is still far below the OECD average of 76%. In Costa Rica, Israel, Ireland and Canada average occupancy rates are above 85%, which is broadly considered to be the limit for safe occupancy for patients in some countries (OECD, 2012[45]).
The very low occupancy rate of hospital beds in Brazil suggests a lot of scope of potential efficiency gains and has been the focus of numerous national and international efficiency analyses. Due to the large number of very small hospitals in Brazil, the 2019 World Bank report finds a staggering average inefficiency of 71%, highlighting substantial scope to expand service provision with existing resources. Based on this model, outpatient hospitals services could be increased by 140% and admissions by 79% while keeping expenditure constant if efficiency was maximised. Alternatively, the same level of results in hospitals could be achieved with 34% less spending, generating savings around BRL 12.7 billion (World Bank, 2017[26]). Unsurprisingly, the report finds that inefficiencies are much more pronounced in small municipalities and mainly driven by hospitals with less than 100 beds.
In a performance assessment of public hospitals, the Brazilian Federal Court of Accounts also found ample evidence of inefficient service provision (Tribunal de Contas da União, 2020[46]). Applying the same method as the World Bank but differentiating by hospital type, the results of this assessment indicate further that efficiency increases with hospitals size but no difference across regions. Interestingly, the report also finds that (i) public hospitals under direct administration are less efficient than those under indirect administration; (ii) hospitals under management of the states are more efficient than those managed by either municipalities or the federation; and (iii) that public hospitals managed by “social organisations” (Organizações Sociais de Saúde) have a better efficiency score than other public hospitals. For the latter finding, however, it is important to note that this may also be due to selection bias and the fact that OSS-managed hospitals are nearly three times bigger than the average public hospital (151 beds vs. 61 beds).
The way inpatient delivery is planned for SUS contributes to excess capacity
Even considering that the COVID-19 pandemic has shown that some easily mobilised inpatient reserve capacity can be advantageous under exceptional circumstances, the low efficiency in the hospital sector in Brazil has adverse effects.18 From a purely economic perspective, the simple solution to improve efficiency in the hospital sector would be to close many small hospitals. In reality, this is more complicated. In areas with very low population density, alternative treatment facilities may be hundreds of kilometres away. In addition, from a political economy perspective, mayors and municipal health secretaries have little to gain from a closure of existing health facilities as this would not be appreciated by voters. A more feasible approach could be a conversion of some small hospitals in rural areas into more intermediate health facilities that can treat urgent cases and patients with acute care needs for a limited period of time. This should be accompanied by a strengthening of transport opportunities to better equipped general hospitals in urban centres for patients requiring urgent inpatient care for a sustained period of time. This model could also be tied in with the roll-out of tele-health applications to help triage patients, distinguishing those who need immediate transport to general hospitals from those who can be treated locally.
On how to find the right balance between efficient acute care provision and accessibility in rural areas, lessons can be learned from some OECD countries with similar spatial challenges. In Canada, all provincial and territorial Medicare plans are expected to provide uniform access to hospital care also in rural and remote areas (Marchildon, Allin and Merkur, 2020[47]). They achieve this by extensive referral patterns involving medical transportation from rural and remote areas to tertiary care hospitals in urban areas. This involves a wide network of road- and air-based emergency medical services. In Australia, some states and territories have developed multi purpose health service (MPHS) as a service for flexible care. It is an amalgamation of services including acute hospital care, residential aged care, community health, home community care and other health related services and generally established in populations not large enough to support a separate hospital, residential aged care and community care services (Queensland Government, 2018[48]). An alternative concept popular in Finland is to embed an inpatient ward into primary health care facilities of municipalities (Keskimäki et al., 2019[49]). These GP-led facilities are typically equipped with 30-60 beds. In recent years, these facilities have taken a more active role in rehabilitation and cancer care. Around half the beds are used for acute and chronic care each.
The existence of many small hospitals leading to the described efficiency issues appears to be also the result of the current mode of hospital planning in Brazil. Law 8080/1990 gives municipalities a central role in planning and management of SUS services, in co-operation with states and health regions. Yet municipalities differ vastly in size and also in the capacity to perform complex managing tasks, such as the operation of secondary and tertiary care facilities. In a number of OECD countries, hospital planning is delegated to a higher governmental level. In Australia, the administration and performance of public hospitals is the responsibility of the states and territories as system managers. In Canada, provincial ministries are responsible for major new capital (e.g. hospitals) and some infrastructure planning (Marchildon, Allin and Merkur, 2020[47]). This is also the case in some social insurance-based health systems. In Germany, for example, hospital planning is carried by the 16 ‘Länder’ while most public hospitals are owned by municipalities. Thus, Brazil could consider moving hospital planning competencies to another government level, be it the states, “health regions” or “macroregions” (see Section 3.5.5). What needs to be in place are clear federal guidelines stipulating transparent planning processes and accountability.
There are few incentives for better performance in inpatient care delivery
The hospital landscape in Brazil is diverse. Public hospitals can be owned by the federal government, the states and municipalities and may be managed directly by system managers or employed hospital managers. The management of public hospitals may also be outsourced to private “Social Organisations” (OSS). In addition, state or municipal health managers also contract private non-profit and for-profit hospitals for service delivery under SUS. The latter two types of hospitals will also cater for private patients that either use their insurance coverage or pay directly. Overall, in 2019, public hospitals and private not-for-profit hospitals each accounted for around 38% of all hospital beds, with the remaining 24% provided by private for-profit hospitals.
In line with the diverse hospital landscape, the current form of financing specialist and inpatient activity in Brazil is very complex and differs across states and municipalities. On average between the years 2010-14, SUS financing for inpatient care was to 39% made from federal sources, to 48% from the states and to 13% from municipalities (Ministério da Saúde/Fundação Oswaldo Cruz, 2018[29]). Most of the federal resources to finance activities of medium and high complexity (Média e Alta Complexidade- MAC) are transferred to states and municipalities and the transfers are subdivided into different components: (i) fee-for-service payments based on a national price list for procedures; (ii) incentives related to national policies; (iii) and a global budget for a set of activities. Municipalities and states have to complement the federal FFS funding. In some states, additional incentive payments related to state priorities exist. Finally, there may be performance bonuses made to hospitals at the discretion of the contracting state or municipality manager.
The current mechanism to purchase hospital services does not appear to incentive improving hospital performance. The transfers from the federal government to states and municipalities are partially based on historic budgets and payment by procedure through a national fee schedule (SIGTAB) which, however, is updated only irregularly, mainly for high costs procedures in the context of ‘judicialisations’. As a result, the fee schedule sends distorted price signals and payments do not necessarily reflect resource use. Hence, an efficient resource allocation between different hospitals becomes challenging. Some hospitals may receive insufficient funding for the services they provide. Generally, FFS payments also encourage hospitals to provide more procedures than necessary.
To improve technical efficiency, many OECD countries have introduced prospective case-based payment systems based on Diagnosis-Related Groups (DRG) to pay for hospital activity (OECD, 2016[44]). For the operationalisation of this mode of payments, patients are grouped into different patient groups reflecting the resource-intensity of the treatment taking into account diagnosis and other factors – called DRG. Different weights are associated with the various DRGs reflecting average treatment costs. After discharge, the hospital receives a payment reflecting the weight of the DRG. Alternatively, DRGs can also be used for the allocation of hospital budgets. In this case, hospitals budgets are defined via the sum of DRG weights (or ‘case-mix’) reflecting the difference in complexity of cases across hospitals. Depending on how DRGs are used, they can incentivise hospital managers to reduce costs per patient, increase the revenue per patient and increase the number of patients (Quentin et al., 2011[50]). To avoid any possible skimping of care, quality of care should be monitored. For an accurate calculation of average resource use per patient, hospital cost accounting systems need to be in place. Brazil could explore options to move towards such a patient classification model and to use it to pay for service provision. There is a wealth of experience in the use of DRGs in OECD countries and how to adapt existing classifications to national circumstances. The existing hospital datasets in Brazil on procedures could serve as a good starting point; what seems to be missing so far is detailed costing information.
The provision of low value care remains an issue in Brazil
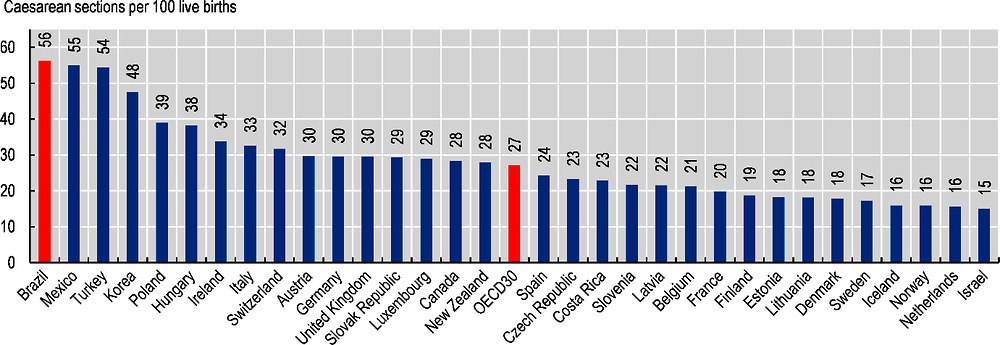
Brazil also encounters issue with wasteful clinical spending. One example of health services that are of low value are double examinations or costly procedures that may not be clinically necessary. Caesarean sections can fall into the latter category. While they can save the lives of mother and infant for medically indicated reasons, these surgical procedures can cause complications leading to disability and deaths especially if carried out in facilities that lack capacity to conduct safe surgery. Based on a systematic review, the WHO concludes that C-section rates above 10% are not associated with reductions in maternal and new-born mortality rates at the population level (WHO, 2015[51]). Brazil is one of the leading countries for these types of intervention. In 2019, birth via C-section accounted for 56% of all life births in Brazil with some significant variation across the country – ranging from 35% in the Northern state of Roraima to 67% in the Central-Western state of Goiás (Secretaria de Vigilância em Saúde, 2021[52]). The share in Brazil is above that of any OECD country and more than twice the OECD average (Figure 3.12). In many European countries and Israel, the proportion is below 20%. The high and growing number in Brazil suggests that other factors than medical indication play an important role in the decision making of delivery. This may be due to cultural differences in patient expectations, availability of midwives and nurses, medical practice but also financial incentives for health providers. There is also some international evidence that private hospitals tend to perform more caesarean sections than public hospitals (OECD, 2019[8]).
Reducing the C-section rate is an objective in Brazil and included in the National Health Plan 2020-23. Some OECD countries have also taken measures to address the trend of increasing C-sections. In Australia, for example, a number of states have developed clinical guidelines and required reporting of hospital caesarean section rates, including investigation of performance against the guidelines. These measures have discouraged variations in practice and contributed to slowing down the rise in Caesarean sections (OECD, 2019[8]). A few countries including France, the United Kingdom and Korea have introduced financial incentives to reduce the use of unnecessary caesarean sections, for example by reducing the price gap or aligning the prices between normal delivery and C-section that hospitals can charge (OECD, 2014[53]). Brazil should consider these regulatory options to curb down C-section rates but could also intensify efforts to raise awareness of this issue among young women.
More generally and going beyond C-sections, encouraging patient-provider conversation about whether certain treatments are adequate can be one way to reduce low value care. This is the focus on the Choosing Wisely® campaign, an initiative led by clinicians that began in the United States in 2012 and which has since then spread to several other countries, including Brazil (OECD, 2017[24]). This initiative provides an evidence-based list of “do not do’s” across multiple medical specialties to help identify inappropriate care that is of little value to patients. The recommendations included in these lists cover many different clinical areas, for example under which conditions expensive imaging test for lower back pain are unjustified or when antibiotics should not be prescribed.
An important tool to improve health care quality and reduce unnecessary care is the establishment of evidence-based clinical practice guidelines and monitoring their compliance. Recent research suggest that while important progress has been made in Brazil in the development of these guidelines in recent years, many still lack transparency and methodological rigour and do not necessarily follow international standards (Colpani et al., 2020[54]). High geographical variation in medical practices in a country can signal inefficient care provision and low adherence to clinical guidelines. To monitor variation in health care activity that may not be medically justified, many OECD countries including Australia, Canada, the United Kingdom and the United States have developed atlases (OECD, 2017[24]).
3.5.5. Access to medication can be problematic in Brazil
SUS provides access to a range of essential medicines based on a positive list (known by the acronym ‘Rename’) which is updated annually after assessment by CONITEC once financing is agreed upon by the tripartite commission (CIT).19 The 2020 list includes 921 items financed by the three levels of government.
These medicines are clustered into various groups according to the financing mechanism applied. The ‘basic component’ of pharmaceutical assistance (CBAF) covers medicines and other medical inputs for conditions related to primary care. The ‘strategic component’ (CESAF) refers to pharmaceuticals for control of specific diseases that have a potential endemic impact, frequently related to situations of social vulnerability (e.g. tuberculosis, malaria, HIV). The ‘specialised component’ (CEAF) covers medications used to treat more specialised clinical conditions, mainly high cost chronic illnesses. The CBAF medicines are co-financed by all three levels of government. The federation makes transfers to the municipalities based on population size, adjusted for the human development index of the municipality. States and municipalities also have to contribute to this programme. Purchase and dispensing are the responsibility of the municipalities (Ministry of Health, 2019[55]). CESAF pharmaceuticals are purchased by the Federal Ministry of Health and distributed to the states, who, in turn, are responsible for dissemination across their territories (Ministry of Health, 2019[55]). The financing of CEAF medicine is more complex as they are subdivided into three groups, of which some are exclusively financed by the federation, some only by the states, and some by all three levels of government (Ministry of Health, 2019[55]).
There are several dispensing channels for medication in Brazil, mainly public and private pharmacies. Since 2004, the Farmácia Popular programme provides access to free and subsidised pharmaceuticals under SUS. Under this programme, people can obtain medication for hypertension, diabetes and asthma without cost-sharing. For some other pharmaceuticals, for example to treat dyslipidaemia, Parkinson’s disease or osteoporosis, co-payments are required, with governmental subsidies set at 90% of the reference price. More than 31 000 pharmacies (including private pharmacies) in 79% of municipalities participate in this programme and the programme has shown to reduce hospital admissions and mortality due to hypertension and diabetes (OECD, 2015[25]). Beyond the Farmácia Popular programme – and depending on the municipality – patients may also obtain pharmaceuticals from their basic health care units (free of charge) or from private pharmacies (at their own costs).
Despite the diversity of distribution channels and the comprehensiveness of the positive list of essential medicines under SUS, there are problems in accessing medications in Brazil. Results of the 2019 Health Interview Survey highlighted that 15% of those who received a prescription for medication during their last medical consultation were not able to obtain all prescribed items (IBGE, 2020[3]). The survey also provides information on where people obtained their medication. Interestingly, on average, only around 30% of all people who were issued a prescription at their last medical visit used the public service (IBGE, 2020[3]), ranging from 42% among the poorest population group to 7% among the well-off. This low proportion of public service use among the poor is remarkable as it could suggest that they resort to private pharmacies (at their own expenses) to acquire their medication due to lack of alternatives. This conclusion is in line with previous research on this topic. Comparing prices, affordability and availability of 50 essential pharmaceuticals in Southern Brazil, Bertoldi et al. found less than expected public sector availability of generics or ‘similares’20 requiring patients to go more frequently to private pharmacies where medication is more readily available, but prices higher (and not covered by SUS) (Bertoldi et al., 2012[56]). In addition, their research stressed that prices in Brazil for brands, generics and ‘similares’ were higher than international reference prices. Thus, poor availability in public facilities and comparatively high prices help explain why pharmaceuticals comprise the largest share of out-of-pocket spending in Brazil (see Section 3.2), albeit being theoretically covered under SUS.
Accessing medication can be an issue in Brazil and better procurement may help
Given the size of the country, ensuring access to essential medicines at all times for everyone is a logistical challenge in Brazil. However, the way purchasing is organised may exacerbate this problem and there appears to be some room for efficiency gains. While making municipalities responsible for procurement for ‘basic’ medication (CBAF) may allow them to better respond to local population needs, it also leads to a higher degree of fragmentation of the purchasers market. With one-fifth of municipalities having fewer than 10 000 inhabitants, many do not have the capacity to adequately engage in such a complex activity and lack the size to be in a strong position to negotiate prices with manufacturers. While many ‘purchaser consortia’ among municipalities (and even states, for specialised medications) exist, pharmaceutical procurement responsibilities for SUS pharmaceuticals could be reconsidered all together. For medication in the CBAF category, procurement could be generally delegated to states or the federation. Alternatively, Brazil could develop national negotiations or public bidding processes for CBAF medicines on a federal level where municipalities would purchase directly medicines from (nationally) contracted manufactures for the (nationally) agreed price. Procuring pharmaceuticals in the largest possible quantities to achieve economies of scale – both in centralised and decentralised health systems- is among the principles of good pharmaceutical procurement of WHO (WHO, 1999[57]). These principles also highlight that the performance of local procurement should be monitored closely as decentralisation may threaten the appropriate selection of drugs, and the potential for discounts through bulk purchases, quality assurance and accountability. The Brazilian Federal Court of Account also sees decentralisation as a challenge for pharmaceutical procurement and has issued some guidelines to improve purchasing for the different levels of government (Tribunal de Contas da União, 2018[58]).
There is room for greater use of unbranded generics
Medical goods (including pharmaceuticals) are a substantial cost component of overall health spending in Brazil (20%) and can be a financial burden for both governments and people. Generally, the development of generic markets is an opportunity to increase efficiency in pharmaceutical spending. Underutilisation of generic drugs can be a substantial source of inefficiency as generics have the same therapeutic effects as branded alternatives but are typically much less expensive.
In Brazil, the development of the generic market has progressed rapidly since the Generic Medicines Law was passed in 1999. The law required tests for bioequivalence of generic products for marketing authorisation that made the requirements for market entry in Brazil relatively strict compared to those in other Latin American countries (Massard da Fonseca and Shadlen, 2017[59]). The legal change led to a decrease in the market share of originator drugs and price reductions for originator products and ‘similares’ (which already existed before 1999) in the ten years following the introduction of this law (Bertoldi et al., 2019[60]). In 2019, the generic market share in the retail market in Brazil stood at 78% by volume, well above the OECD average of 52%, while at 69% of all retail pharmaceutical sales by value, which was nearly three times the OECD average (26%) (Figure 3.13). However, it is important to note in this context that the majority of the generics used in Brazil -as in most Latin American countries- are similares.21 Similares are copies of off-patent products using a trade name instead of the name of the molecule. In Brazil, most simliares can be understood as ‘branded generics’ as they have to prove bioequivalence for renewal of registration since 2003 (this is not necessarily the case in other Latin American countries). Their prices are usually higher than those of non-branded generics. In contrast, in OECD countries, branded or unbranded generics do not make a major cost difference, mainly because health systems provide coverage for them irrespective of this classification. This also implies that price differentials between originator and generic medicines (including branded) are smaller in Latin American countries than across the OECD.
While the use of unbranded generics is relatively high in Brazil compared to other Latin American countries (OECD/The World Bank, 2020[61]), there appears to be some scope to rein in pharmaceutical spending. In a comparison of prices for pharmaceuticals in six Latin American countries between 2010 and 2015, Álvarez and González found that, on an aggregate level, those seen in Brazil were higher than those in Argentina, Chile, Colombia, Mexico and Peru, for both ex-manufacturer and retail prices (Álvarez and González, 2020[62]). This ranking is confirmed when looking at prices for unbranded generics. Above-average international prices for unbranded and branded generics in Brazil were also found by Bertoldi et al. (Bertoldi et al., 2012[56]). Earlier research suggests that generic prices (branded and unbranded) in Brazil were above those seen in the United States, France and Spain and on the same level as in Canada and in the United Kingdom (Danzon and Furukawa, 2008[63]). The comparably high prices for generics may partly be explained by the way prices are set. While a generic drug entering the market needs to be at least 35% below the price of the originator product, there are no regular price updates required once authorisation is issued (Bertoldi et al., 2019[60]). As a result, the price of a generic may actually exceed that of the originator drug. Moreover, the 35% difference is not applicable to branded generics (Bertoldi et al., 2019[60]), and prescriptions for branded generics are currently exempt from substitution to unbranded generics (Massard da Fonseca and Shadlen, 2017[59]).
More regular revisions of maximum prices of generics and increasing the scope of substitution to include similares with proven bioequivalence could be ways for Brazil to rein in overall pharmaceutical spending and improve affordability among disadvantaged population groups. Expanding campaigns to educate prescribers and patients on the interchangeability of generics could also be an option since studies suggest that there is lack of confidence in the quality of generics and confusion how to differentiate between originator, similar and generic products (Massard da Fonseca and Shadlen, 2017[59]). The government tried to address this in 2014 by proposing to add the label “EQ” to the packaging of interchangeable products, also hoping that this would increase competition and thereby reduce prices. Yet this proposal was not enacted, giving in to industry concerns that the “EQ” symbol would send a message to patients to ignore branded medicines (Massard da Fonseca and Shadlen, 2017[59]).
3.5.6. Brazil will face a challenge to cope with future long-term care needs in the context of an ageing society
Brazil will go through a fundamental demographic transition in the next decades that will have an impact on the health and social system. By 2050, the share of the population being 65 years or older is projected to rise to 21.9%, the proportion of the elderly with 80 years or more to 6.5% (OECD, 2019[8]). This transition will not only increase the number of patients with chronic conditions such as diabetes but will also raise the number of people with long-term care needs – i.e. those who need help to perform activities of daily living (ADL) and/or instrumental activity of daily living (IADL).22 Even now, these needs are already visible in Brazil. According to the 2013 Health Information Survey, 6.8% of the elderly had functional limitations that require ADL support while 17.3% needed help with IADL (Ministerio da Saúde, 2018[64]).
Reviewing the evidence of long-term care policies in Latin-America and the Caribbean, a report by the Inter-American Development Bank finds that comprehensive long-term care policies in the region are basically non-existing at the moment, with very limited regulation or public provision of long-term care services (Bloeck, Galiani and Ibarrarán, 2017[65]). To satisfy the long-term care needs of the elderly and dependent population groups, Brazil mainly relies on informal care provision by family members and relatives. The formal long-term care sector in Brazil is still underdeveloped and fragmented. The Ministry of Health is responsible for elderly health and has developed a National Health Policy for the Elderly (PNSPI) in 2006, with the priority to promote, maintain and recover the autonomy of elderly in the context of comprehensive primary health care. However, recent research suggests that the implementation of this policy still faces a number challenges in municipalities including lack of specific actions, limited accessibility and lack of training for health professionals (Damaceno and Chirelli, 2019[66]). The Ministry of Citizenship (formerly Ministry of Social Development), on the other hand, is responsible for policies regarding long-term care facilities (‘Instituição de Longa Permanência para Idosos’) but the role of the state in this area is limited to providing shelter for the poor (Ministerio de Saúde, n.d.[67]). A survey from 2009 found more than 3 500 registered residential facilities with around 100 000 residents representing around 1% of elderly population. Two-thirds of the facilities were run by non-profit organisation and only 7% were public. On average, only 20% of costs were covered from public financing with most of the remaining part by patients themselves (Garcez-Lemell and Deckers Lemell, 2014[68]).
Experiences from OECD countries highlight the value of a comprehensive strategy to meet the increasing long-term care needs by moving towards more formal care provision. A key element of such a strategy would be to reduce the reliance on family members to provide care. Sustaining such care arrangements will become increasingly difficult in the future with shrinking family size and growing labour force participation by women. These informal care arrangements also hamper economic growth and are associated with an increased negative impact on mental health of caregivers.
The models how professional long-term care at home are organised differ across OECD countries. In many cases, care professionals will be employed with dedicated home help providers that focus on the support with ADL, IADL and medical nursing care. Depending on the country, these providers may be managed by municipalities, non-profit organisation or private enterprises. For people with severe long-term needs or who lack an appropriate environment to be cared for at home, OECD countries attempt to provide a sufficient number of beds in residential long-term care facilities. These care arrangements can take different forms depending on the activity limitations of the elderly, ranging from assisted living facilities where care assistance is available on-sight to nursing homes that allow for 24-hour care provision for people with the severest form of activity limitations.
To ensure that these services are accessible to those with needs, the bulk of the cost of long-term care provision in OECD countries is financed by the government or social insurance schemes. On average, OECD countries allocated around 1.5% of their GDP (or the equivalent of USD 760 per capita) to long-term care in 2018 of which nearly four-fifths were covered by public schemes (OECD, 2020[69]). Yet, in some countries, important gaps in long-term care coverage still remain and recent research by the OECD highlight that the high costs for care can represent a significant financial burden for people with long-term care needs (Oliveira Hashiguchi and Llena-Nozal, 2020[70]).
Transitioning towards more formal long-term care provision will take time and is resource-intense but remaining unprepared for the demographic shift will be more costly in the long-run. Most OECD countries have used a phased approach by gradually introducing and increasing public long-term care benefits. Taking inspiration from developments in Chile, a first step for Brazil could be to better support family carers (with better training and respite care opportunities) while at the same time expanding day care facilities and rolling out home care. As a transitionary method to meet long-term care needs in Brazil, conditional cash transfers or vouchers for dependent people could be introduced, with which they can purchase LTC services from the public or private sector. In some OECD countries cash benefits allow beneficiaries to either purchase professional services or pass them on to their informal care-givers. However, when using these types of benefits, it should be monitored that it does not negatively affect labour force participation by women. At any rate, as a starting point, long-term care benefits should be more explicitly defined in Brazil with eligibility criteria based on ADL/IADL needs assessments, and the responsibilities between the Ministry of Health and Ministry of Citizenship should to be clarified.
3.5.7. Administration and governance of the system is complex and costly
As could be seen throughout the chapter so far, the administration and governance of the Brazilian health system is complex and resource-intense. Within the public sector, the management, planning and financing of SUS is shared across the three levels of government requiring extensive co-ordination across actors. This refers both to vertical co-ordination as seen by the tripartite inter-management committee (CIT) and the bipartite inter-management committees (BIT) on a state level but also to horizontal co-ordination between states (e.g. with the National Council of State Health Secretaries CONASS) and municipalities (e.g. with the National Council of the Municipal Health Secretaries CONASEMS). In addition, the Health Pact of 2006 has introduced new entities charged with institutionalising service delivery planning on a more regional level – the “health macroregions” (Macrorregiões de saúde) and the “health regions” (Regiões de saúde). These are composed of various neighbouring municipalities supported by the states. Moreover, there is also a huge number of standing bodies to safeguard civil society participation in all three levels of government, such as health conferences and health councils. In addition, there is a highly developed private sector – both from a payer and provider perspective – which adds to the complexity of governance but also health service delivery. While it is obvious that attempting to provide equitable access to high quality health care in a country such as Brazil – characterised by cultural diversity, a large geographic division and high social inequalities – requires substantial co-ordination, there appear to be some areas where administration could be streamlined and governance strengthened to improve effectiveness or costs reduced.
The administration of the complex Brazilian health system comes at a cost
The complexity of the management of the SUS and the strong role of the private health insurance market in Brazil results in a very high share of resources needed to administer the health system. In total, more than 6% of current health expenditure is used for governance and health system and financing administration.23 This share is higher than in nearly all countries of the OECD and more than twice its average (Figure 3.14). The fact that Brazil has an important private health insurance market explains partly why the country ranks very highly in an overall comparison since private health insurance is typically associated with much higher administrative costs than public schemes (OECD, 2017[24]). However, what is surprising in the case of Brazil is that for government schemes the share of administrative expenses is also substantial, standing at 5.7% of total government health expenditure. Other countries with mainly tax-financed system and residence-based entitlements such as the United Kingdom, Italy or the Scandinavian countries dedicate a much smaller proportion of their resources to the administration of the health system. A reasonable hypothesis why the share in Brazil is so high is that it reflects the complexity of SUS.
It should be made clear that expenditure for governance and health system and financing administration are not bad per se. Stewardship and oversight are needed to make sure that services are provided safely and effectively throughout the country. However, countries with high administrative costs should carefully weigh if they obtain corresponding benefits in return. In the case of Brazil, this is not obvious. It rather seems that the joint responsibilities across all three levels of government in the management of SUS contribute to a situation characterised by unnecessary complexity, redundant tasks and a lack of clarity and accountability. Moving forward, Brazil should map out and evaluate critically all processes related to the management and planning of SUS at all levels of government. This can contribute to identifying superfluous administrative procedures, can help streamline competencies for each level of government and can be the starting point for discussing changes in governance and responsibilities across the levels of government to increase efficiency and accountability in SUS. In that context, Brazil should also carefully review data requirements for improved service delivery planning in SUS. While existing knowledge gaps that have been identified should be addressed (Chapter 4), there also appears to be disconnect in the country between data availability and data usage by planning authorities and decision-makers. Improving data exchange and communication can prevent that Brazil becomes “data rich but information poor”.
Stronger focus on regionalised planning can overcome some inefficiency barriers
A key topic when reviewing management responsibilities in SUS is the role of municipalities. They are important actors in the financing and management of SUS as well as in service delivery planning in line with the principle of “decentralisation” on which SUS is based on. Yet the size of municipalities differs vastly across the country, which affects the capacity of municipal health officers to effectively organise and manage SUS. The existence of many small municipalities raises the question whether some of the SUS functions should not better be delegated from a local to a regional level.
The need for better regional co-ordination to improve service delivery planning has been realised in Brazil with the Health Pact of 2006 and with Law 7 508 of 2011. The latter provides guidelines for the establishment of “health regions” which are composed of a varying number of (neighbouring) municipalities within states. These “health regions” are defined in the multi-annual state health plan and have to combine at least primary care, urgent and emergency care, psychosocial care, specialised outpatient and hospital care and health surveillance. To organise care of medium and high complexity the regions should organise themselves in “macroregions”.24 On paper, it appear that the installation of such health regions can be a powerful tool to improve care co-ordination and efficient service provision and also facilitate the operation of health care networks. However, as of now, it does not seem that regionalisation has shown its full potential. One problem appears to be that these entities have no decision-making power, budget authority or human resources and rely entirely on municipal and state support. There may also be reluctance among state and municipality officials to delegate financing and planning competences to the health regions for fear of loss of influence. However, the strengthening of the roles and responsibilities of health regions appears to be a vital element to improve SUS performance.
Access to health services through courts are a drain on available resources
A specific challenge to the Brazilian health system is the fact that a high number of people resort to the judicial system to access health care at the expense of SUS.25 This is the case when people who have prescribed treatment or pharmaceuticals denied to them, invoke the Federal Constitution which stipulates that “…health is a right for all and duty of the state”. These so-called “judicialisations” have been growing constantly for many years and represent a considerable drain to the scare resources of SUS. Between 2010 and 2015, federal spending based on judicial decisions increased tenfold, reaching BRL 1 billion (Tribunal de Contas da União, 2017[71]) or roughly 1% of the federal health budget, mainly related to access to high cost medicine.26 At the state level, the aggregated costs for these cases seem to be even higher (Tribunal de Contas da União, 2017[71]).
Getting access to health care services, which are not deemed cost-effective based on judicial interventions, however, is problematic, both, from an efficiency and equity perspective. It is an inefficient use of resources because it complicates priority setting in health and runs against the purpose of HTA conducted by CONITEC. As an example, based on court rulings, a substantial amount of “judicial spending” in 2014 went on the drug Soliris®, which had not been granted market authorisation at the time and where annual treatment costs are estimated to be over BRL 1 million per person (Tribunal de Contas da União, 2017[71]). In addition, the high and growing number of court cases also put a strain on the judicial resources. By the end 2018, all pending health related court cases at all court levels in Brazil (including the “judicial cases”) amounted to over 2.2 million (Vieira, 2019[72]).27 Beyond preventing an efficient use of resources based on criteria such as cost-effectiveness, “judicialisation” is also a problem from an equity perspective since those who get access to health care based on court rulings are typically those who are able to pay for legal fees or know how to navigate the legal system – mainly the rich and the better educated.
For international observers, the magnitude of the problem and the fact that judges give favourable rulings for access to experimental treatment for not authorised medication on a regular basis seems puzzling, especially since the establishment of CONITEC was an important achievement for the Brazilian health system.28 By doing so, judges become de facto co-managers of the health budget. The Ministry of Health is also concerned about the rise in ‘judicialisations’ and has taken a number of measures to help judges make an informed decision. For example, a co-operation agreement was signed with National Council of Justice (CNJ) with the objective to provide advisory services to the different competent courts in the judicial system. While the legal system can play an important role in guaranteeing universal health care in many countries, courts in OECD countries typically do not systematically bypass standardised HTA processes but rather hold HTA agencies to account in case they find flaws in the assessment processes. A change in the judicial culture in Brazil seems critical for a solution to this problem. A recent analysis of judicialised court rulings finds that the establishment of CONITEC had little impact on courts’ tendency to rule in favour of patients (Wang et al., 2020[73]). In most cases, CONITEC decisions were simple ignored and not even cited in the ruling decisions. Making the concept of cost-effectiveness in the provision of SUS more explicit could also be an option to reduce the size of the problem but critics would argue that the current legal framework is already sufficient to reign in ‘judicialisations’.29
Budget issues prevail at federal and other government levels and raise questions whether they can accommodate changing priorities
The overall resources available to finance activity of SUS is decided on the three levels of government taking account of the relevant laws and constitutional amendments which, on the one hand, define the minimum spending floor for each governmental entity but, on the other hand, limit annual federal public spending growth to inflation. On the federal level, the overall budget is generally perceived as very rigid with 93% of spending mandated by law either through earmarking, indexation or mandatory spending floors (OECD, 2020[11]).
The executed federal budget on health in 2018 stood at around BRL 121 billion, financing around 42% of all SUS expenditure (SIGA Brasil, n.d.[74]). Due to the decentralised nature of the management of SUS around two-thirds of federal health spending refers to transfers to the states and municipalities to purchase health care goods and service. Most of these transfers are directed towards municipalities. Since 2007, the federal transfers are structured around six financing blocks (primary care, medium and high complexity hospital and outpatient care, health surveillance, pharmaceutical assistance, SUS management and investment), including subcomponents, with the individual transfers being determined by population size but for some blocks, such as primary care, other factors reflecting difference in needs also play a role. While some flexibility in the use of funds has been allowed for over the years, there is an issue at state and municipality level to reallocate earmarked federal funds for other purposes (dos Santos and de Luiz, 2016[75]). The current budgeting practice is also not conducive to the envisaged roles of the health networks and it is difficult to see how ‘health regions’ or ‘macro regions’ can play a bigger part in planning in the current environment without having some sort of budget autonomy.
More budget flexibility would make it easier to pursue policy priorities. In addition, there is a wide-spread use of amendments to the federal budget by parliamentarians as a tool to increase spending in their constituency. This practice undermines spending efficiency and transparency and makes local authorities depend on members of congress (OECD, 2020[11]). These spending items are also typically not audited. The fiscal implications of these amendments have been growing in recent years, with spending commitments reaching BRL 12.9 billion in 2019 (Portal da Transparência, 2019[76]). More than half of the committed amount stem from amendments in the area of health (BRL 6.7 billion) mainly for primary care or care in hospitals.
Substantial resources are diverted from health service delivery
The intentional misuse of funds and corruption is commonplace to differing degrees around the globe in many areas of public life and Brazil is no exception. In fact, Brazil had some major corruption scandals involving prominent public figures in the last decade. In 2020, Brazil ranks 94th of 180 countries in the perceived level of public sector corruption,30 much lower than nearly all OECD countries (Transparency International, 2020[77]). When it comes to health care, fraud and the diversion of funds can take different forms. Health providers and professionals may bill services to purchasers that they did not deliver, system managers may contract health providers at artificially high prices or divert health care goods for their own benefits and patients may offer bribes for health providers or professionals to ‘jump the queue’ for quicker treatment. This practice is problematic for a number of reasons. It is inefficient spending, frequently creates equity issues and undermines the trust of people in the public health system. In 2013, corruption in health was perceived to be more widespread in Brazil than on average across OECD countries (Figure 3.15). It was similar to the United States and Chile, but below Colombia, Greece or Lithuania (Transparency International, 2013[78]). On the other hand, it was much higher than in Denmark, Spain, Finland or Australia.
Since information on illegal activity its patchy at best, it is very difficult to quantify the problem. When looking at the population willing to engage in integrity violations, 5% of Brazilians reported having paid bribes in public clinics and health centres within 12 months in 2019, down from 7% in 2017 (Transparency International, 2019[79]). Among Latin American and Caribbean countries, this was a very low share. However, misuse of funds does not necessarily require the patient. Recent research estimated the total costs of fraud, corruption and misuse of funds in the health sector in Brazil to be around BRL 14.5 billion or 2.3% of total health spending (Instituto Ética Saúde, 2020[80]). Due to its complex nature that involves many actors at different levels of government, the misuse of fund may be more difficult to detect in SUS than in other health system. Indeed, in a 2017 report, the Federal Court of Accounts highlighted important deficiencies in the National Auditing System of SUS as an oversight instrument in municipalities and states (Tribunal de Contas da União, 2017[71]). It also noted that 55% of the federative entities that were audited did not implement SUS’ internal auditing component.
Brazil tries to address these issues. For example, to detect misuse of public funds the Comptroller General in Brazil conducts a substantial number of special audits each year. Between 2002 and 2018, the funds associated with irregularities amounted to BRL 23.8 billion, of which 28% (BRL 6.6 billion) were under the remit of the Ministry of Health (Controladoria-Geral da União, n.d.[81]).
There are different policy levers used in OECD countries to mitigate integrity violations in health addressing the different stakeholders (OECD, 2017[24]). One response is primarily organisational in the sense that it involves assigning responsibilities for detecting or tackling integrity violations in service delivery and financing to specific institutions. Depending on the country, these can be dedicated central or government programmes or institutions, or these responsibilities are delegated to public or private payers. In some instances fraud detection is very pro-active going beyond simple audits. The Belgian National Institute for Health and Disability Insurance, for example, uses data mining to detect integrity violations in service delivery and payment. To tackle inappropriate business practices, countries’ responses are typically regulatory in nature and consist of limiting or banning certain practices. The main domains where some countries have introduced regulation seek to limit self-interested referrals by health providers and the means by which the pharmaceutical industry is allowed to promote sales – including Sunshine regulations.31 In the last 15 years, a number of countries introduced specific and comprehensive legislation, notably France, Portugal, the Slovak Republic and the United States.
More clarity about the role of the private sector can improve health system performance
Traditionally, Brazil has an important private health sector predating the inception of SUS and the Federal Constitution of 1988 warrants the continuation of private service delivery and private health insurance. Private providers play a vital role to ensure access for SUS patients, in particular for inpatient care. In addition, private organisations are contracted to manage public hospitals or other facilities, and private health insurance can ‘supplement’ SUS coverage. However, the co-existence between a public and private sector is not without friction and can be a source of inefficiency.
Private “social organisations” (OSS) have become a popular tool among some SUS managers to operate public health facilities. By contracting out the management of a health facility to a private company, this option gives more flexibility in hiring staff. Some studies highlight that public facilities under OSS management have more activity or provide services at lower costs than those under direct management (World Bank, 2017[26]), but other research cannot rule out some selection bias when finding that OSS operate more efficiently (Tribunal de Contas da União, 2020[46]). However, OSS contract management seems to be challenging for SUS manager as audit courts have frequently highlighted the insufficiency of monitoring mechanism (dos Santos and Servo, 2016[82]).
The fact that some private hospitals treat SUS patients and private patients simultaneously can lead to reduced access for public patients and associated equity issues. This happens when hospitals (or hospital doctors) receive higher payments when treating private patients. Access problems for public patients were the reason why Ireland introduced a ban on this practice and promoted the clear separation between hospitals that treat public patients from those that treat private patients (Mueller and Socha-Dietrich, 2020[38]). One way to address this issue would be to define a fee schedule that is applicable to all payers. This is the case for example in Germany, where for inpatient treatment the DRG tariffs are identical for public and private patients and applied regardless of whether they are treated in public, private for profit or non-for-profit hospitals.32
The well-developed private health insurance market in Brazil has some peculiarities which distinguishes it from those in OECD countries. It provides mainly duplicate insurance to SUS coverage but de-facto it is used by many as a substitute insurance for SUS as the range of services covered by private plans can be extremely wide. This unclear role of private health insurance is accentuated by the fact that SUS can demand under certain conditions reimbursement of costs from private insurers in case patients use SUS services instead of their private insurance coverage (“ressarcimento ao SUS”). This is unusual compared to OECD countries with a tax-financed system and duplicate insurance. Brazil could benefit from an open discussion to clarify the role private health insurance should play within the health system. As already mentioned, the generous tax subsidies are highly regressive. Moreover, the co-existence of SUS and private insurance is also problematic for care integration. So far, there is very little communication or data exchange between providers (or schemes) in case patients move between treatment under SUS and private coverage. The introduction of a unique patient identifier and interoperability health records between SUS and private insurance would facilitate the co-ordination of care.
The implementation of SUS has been a success in Brazil by providing millions of people access to health services who did not have it previously. Yet, with population ageing and the associated raise in the number of patients with chronic conditions, the Brazilian health system will face increasing spending pressures to make sure future health care needs are met, even under the most optimistic scenario. The analysis of the Brazilian health system has shown that a mix of approaches can make health spending in Brazil more sustainable. The bottom line of this analysis is: Brazil needs to rebalance its public-private financing split by devoting more of its public resources to health but it also needs to spend better.
The chapter has shown that the public share in overall health spending in Brazil is very low compared to most OECD countries but an overall increase in government spending is unrealistic in the current economic climate in Brazil. However, a few possibilities exist to make more public spending available for health care without compromising the path towards fiscal recovery. New sources for health spending on the federal level could be generated by reallocating spending from other areas outside health towards SUS. This relates, for example, to adjusting indexation rules for some social programmes and public salaries. In a similar vein goes the proposal to limit the tax expenditure for health. A starting point would be to at least introduce a ceiling for the deductibility of health expenses and private health insurance premium payments from revenues subject to income/corporate taxation (or abolish it altogether). These savings should be reinvested into SUS.
On the other hand, there is a wide scope for potential efficiency gains in all areas of the health system. Ongoing efforts to strengthen primary health care should continue. This refers to the roll-out of the Health Family Teams and to putting primary care at the centre to co-ordinate health service delivery across levels of care. The “health networks” can play an important role in this concept.
Service delivery planning in hospitals should be rethought in Brazil. A high number of very small hospitals mainly in rural area cannot be operated efficiently. It is clear that people need access to acute care services but the question is whether this cannot be organised differently, by turning small hospitals into intermediate facilities and strengthening transport and tele-medicine options. More generally, payment systems for service delivery in hospitals could be reconsidered to incentivise provider performance.
While coverage to essential medicines under SUS is theoretically very broad, obtaining access is an actual issue for many people, also triggering high out-of-pocket costs. Here, the way purchasing is organised or price setting could be reconsidered.
To be better prepared for rising long-term needs associated with an ageing society, Brazil should start invest in more formal long-term care arrangements. Relying on informal workers will be increasingly difficult also hampering economic growth.
An overarching issue that Brazil needs to address is the immense complexity of operating SUS. This is reflected in the very high administration costs. Competences and responsibilities are frequently shared across levels of governments, however, it appears that they are not always clarified which affects accountability. This complexity permeates all levels of health care planning and operation. There seems to be potential to improve on this. One way forward is to increase efforts to implement “regionalisation” in planning. For this to be successful, the scope of the “health regions” could be widened by delegating some responsibilities from the municipalities to them, accompanied with direct funding and resources. Finally, the relationship between the public and private sector should be clarified.
References
[6] Agência Nacional de Saúde Suplementar (2020), Dados Consolidados da Saúde Suplementar, http://www.ans.gov.br/perfil-do-setor/dados-e-indicadores-do-setor.
[20] Agência Nacional de Saúde Suplementar (2019), Caderno de Informação da Saúde Suplementar: Beneficiários, Operadoras e Planos, http://www.ans.gov.br/images/stories/Materiais_para_pesquisa/Perfil_setor/Dados_e_indicadores_do_setor/total-cad-info-jun-2019.pdf.
[62] Álvarez, R. and A. González (2020), Análisis comparativo de los precios de los medicamentos en América Latina, https://www.cepal.org/es/publicaciones/45423-analisis-comparativo-precios-medicamentos-america-latina.
[56] Bertoldi, A. et al. (2012), “Is the Brazilian pharmaceutical policy ensuring population access to essential medicines?”, Globalization and Health, Vol. 8/6, https://globalizationandhealth.biomedcentral.com/track/pdf/10.1186/1744-8603-8-6.pdf.
[60] Bertoldi, A. et al. (2019), “The Brazilian private pharmaceutical market after the first ten years of the generics law”, Journal of Pharmaceutical Policy and Practice, Vol. 12, https://joppp.biomedcentral.com/articles/10.1186/s40545-019-0179-9.
[65] Bloeck, M., S. Galiani and P. Ibarrarán (2017), Long-Term Care in Latin America and the Caribbean? Theory and Policy Considerations, Inter-American Development Bank, https://publications.iadb.org/publications/english/document/Long-Term-Care-in-Latin-America-and-the-Caribbean-Theory-and-Policy-Considerations.pdf.
[50] Busse, R. et al. (eds.) (2011), Understanding DRGs and DRG-based hospital payment in Europe, Open University Press, https://www.euro.who.int/__data/assets/pdf_file/0004/162265/e96538.pdf.
[4] Castro, M. et al. (2019), “Brazil’s unified health sysytem: the first 30 years and prospects for the future”, Lancet, Vol. 394, pp. 345-56, https://doi.org/10.1016/S0140-6736(19)31243-7.
[54] Colpani, V. et al. (2020), “Clinical practice guidelines in Brazil – developing a national programme”, Health Research Policy and Systems, Vol. 18/69, https://doi.org/10.1186/s12961-020-00582-0.
[81] Controladoria-Geral da União (n.d.), Realizações na Auditoria de Tomada de Contas Especial, https://www.gov.br/cgu/pt-br/assuntos/auditoria-e-fiscalizacao/tomadas-de-contas-especiais/realizacoes.
[5] Couttolenc, B. and T. Dmytraczenko (2013), Brazil’s Primary Care Strategy, https://openknowledge.worldbank.org/handle/10986/13287.
[66] Damaceno, M. and M. Chirelli (2019), “The Implementation of Senior Health Care in the Family Health Strategy: The View of Professionals and Managers”, Ciência & Saúde Coletiva, Vol. 24/5, https://doi.org/10.1590/1413-81232018245.04342019.
[63] Danzon, P. and M. Furukawa (2008), “International Prices And Availability Of Pharmaceuticals In 2005”, Health Affairs, Vol. 27/1, pp. 221-233, https://doi.org/10.1377/hlthaff.27.1.221.
[40] dos Sanots Matsumoto, K. (2018), Parâmetros para dimensionamento de médicos na Estratégia de Saúde da Familia, Universidade do Estado do Rio de Janeiro.
[27] Flamini, V. and M. Soto (2019), “Doing More with Less: How Can Brazil Foster Development While Pursuing Fiscal Consolidation?”, IMF Working Paper, Vol. 236, https://www.imf.org/en/Publications/WP/Issues/2019/11/01/Doing-More-with-Less-How-Can-Brazil-Foster-Development-While-Pursuing-Fiscal-Consolidation-48540.
[68] Garcez-Lemell, L. and M. Deckers Lemell (2014), “Costs of elderly health care in Brazil: challenges and strategies”, MedicalExpress, Vol. 1/1, pp. 3-8, https://doi.org/10.593 5/MedicalExpress.2014.01.02.
[28] Gonçalves, R. et al. (2019), “Influence of the Mais Médicos (More Doctors) Program on health services access and use in Northeast Brazil”, Rev Saude Publica, Vol. 53/110, https://doi.org/10.11606/S1518-8787.2019053001571.
[33] IBGE (2020), 2019 Percepção do estado de saúde, estilos de vida, doenças crônicas e saúde bucal - Module Q - Tabela 3.17, https://www.ibge.gov.br/estatisticas/sociais/saude/9160-pesquisa-nacional-de-saude.html?=&t=resultados (accessed on 10 February 2021).
[41] IBGE (2020), 2019 Percepção do estado de saúde, estilos de vida, doenças crônicas e saúde bucal-Modulo Q- Tabela 3.18, https://www.ibge.gov.br/estatisticas/sociais/saude/9160-pesquisa-nacional-de-saude.html?=&t=resultados (accessed on 10 February 2021).
[34] IBGE (2020), 2019 Percepção do estado de saúde, estilos de vida, doenças crônicas e saúde bucal-Modulo Q- Tabela 3.25, https://www.ibge.gov.br/estatisticas/sociais/saude/9160-pesquisa-nacional-de-saude.html?=&t=resultados (accessed on 10 February 2021).
[3] IBGE (2020), Pesquisa Naciona de Saúde 2019- Informações sobre domicílios, acesso e utilização dos serviços de saúde, https://biblioteca.ibge.gov.br/visualizacao/livros/liv101748.pdf.
[32] IBGE (2020), Pesquisa Nacional de Saude 2019 : percepção do estado de saúde, estilos de vida, doenças crônicas e saúde bucal : Brasil e grandes regiões, IBGE, https://www.ibge.gov.br/estatisticas/sociais/saude/9160-pesquisa-nacional-de-saude.html?=&t=publicacoes.
[80] Instituto Ética Saúde (2020), Fraudes na Saúde geram prejuízo de mais de R$ 14,5 bilhões por ano no Brasil, estima Instituto Ética Saúde, https://eticasaude.org.br/Noticias/NoticiaDetalhe/355.
[83] Lima, S., C. de Brito and C. de Andrade (2019), “Health technology assessment in Brazil – an international perspective”, Ciênca saúde coletiva, Vol. 24/5, https://doi.org/10.1590/1413-81232018245.17582017.
[10] Lorenzoni, L. et al. (2019), “Health Spending Projections to 2030: New results based on a revised OECD methodology”, OECD Health Working Papers, No. 110, OECD Publishing, Paris, https://dx.doi.org/10.1787/5667f23d-en.
[42] Macinko, J. et al. (2018), “Primary care and healthcare utilization among older Brazilians (ELSI-Brazil)”, Revista de Saúde Pública, Vol. 52/2, https://doi.org/10.11606/S1518-8787.2018052000595.
[47] Marchildon, G., S. Allin and S. Merkur (2020), Canada: Health system review. Health Systems in Transition, WHO Regional Office for Europe, https://apps.who.int/iris/bitstream/handle/10665/336311/HiT-22-3-2020-eng.pdf.
[82] Marques, R., S. Piola and A. Roa (eds.) (2016), A provisão dos serviços e ações do SUS: participação de agentes públicos e privados e formas de produção/remuneração dos serviços, Ministerio de Saúde.
[23] Marques, R., S. Piola and A. Roa (eds.) (2016), Financiamento dos sistemas de saúde na América do Sul, Ministério da Saúde.
[17] Marques, R., S. Piola and A. Roa (eds.) (2016), O financiamento dos serviços de saúde no Brasil, ABrEs/Ministerio de Saúde/OPAS/OMS, http://bvsms.saude.gov.br/bvs/publicacoes/sistema_saude_brasil_organizacao_financiamento.pdf.
[18] Marques, R., S. Piola and A. Roa (eds.) (2016), O SUS e seu financiamento, ABrEs/Ministerio de Saude, PAHO.
[75] Marques, R., S. Piola and A. Roa (eds.) (2016), Transferências federais no financiamento da descentralização, ABrES, Ministero de Saude, PAHO.
[59] Massard da Fonseca, E. and K. Shadlen (2017), “Promoting and regulating generic medicines: Brazil in comparative perspective”, Pan-American Journal of Public Health, Vol. 41, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6612747/#B26.
[14] Massuda, A. et al. (2018), “The Brazilian health system at crossroads: progress, crisis and resilience”, BMJ Global Health, Vol. 3/e000829, https://doi.org/10.1136/bmjgh-2018-000829.
[64] Ministerio da Saúde (2018), Orientações Técnicas para a Implementação de Linha de Cuidado para Atenção Integral à Saúde da Pessoa Idosa, https://bvsms.saude.gov.br/bvs/publicacoes/linha_cuidado_atencao_pessoa_idosa.pdf.
[29] Ministério da Saúde/Fundação Oswaldo Cruz (2018), Contas do SUS na perspectiva da contabilidade internacional: Brasil 2010-2014, https://portalarquivos.saude.gov.br/images/pdf/2018/junho/22/CONTAS-DO-SUS.pdf.
[67] Ministerio de Saúde (n.d.), Saúde da pessoa idosa, https://www.gov.br/saude/pt-br/assuntos/saude-de-a-a-z-1/s/saude-da-pessoa-idosa.
[55] Ministry of Health (2019), Relação Nacional de Medicamentos Essenciais (RENAME) 2020, http://bvsms.saude.gov.br/bvs/publicacoes/relacao_medicamentos_rename_2020.pdf.
[37] Miotto, B. et al. (2018), “Physician’s sociodemographic profile and distribution across public and private health care: an insight into physicians’ dual practice in Brazil”, BMC Health Services Research, Vol. 18/299, https://doi.org/10.1186/s12913-018-3076-z.
[38] Mueller, M. and K. Socha-Dietrich (2020), “Reassessing private practice in public hospitals in Ireland: An overview of OECD experiences”, OECD Health Working Papers, No. 118, OECD Publishing, Paris, https://dx.doi.org/10.1787/111171d3-en.
[1] OECD (2021), OECD Health Statistics, OECD Publishing, Paris, https://dx.doi.org/10.1787/health-data-en.
[30] OECD (2021), Payment models in Primary Health Care in Brazil.
[31] OECD (2021), Primary Health Care in Brazil, OECD Reviews of Health Systems, OECD Publishing, Paris, https://dx.doi.org/10.1787/120e170e-en.
[69] OECD (2020), “Focus on Spending on long-term care”, OECD, Paris, https://www.oecd.org/health/health-systems/Spending-on-long-term-care-Brief-November-2020.pdf.
[11] OECD (2020), OECD Economic Surveys: Brazil 2020, OECD Publishing, https://doi.org/10.1787/250240ad-en.
[43] OECD (2020), Realising the Potential of Primary Health Care, OECD Health Policy Studies, OECD Publishing, Paris, https://dx.doi.org/10.1787/a92adee4-en.
[8] OECD (2019), Health at a Glance 2019: OECD Indicators, OECD Publishing, Paris, https://dx.doi.org/10.1787/4dd50c09-en.
[84] OECD (2018), Spending on Primary Care: First Estimates, https://www.oecd.org/health/health-systems/Spending-on-Primary-Care-Policy-Brief-December-2018.pdf.
[24] OECD (2017), Tackling Wasteful Spending on Health, OECD Publishing, Paris, https://dx.doi.org/10.1787/9789264266414-en.
[44] OECD (2016), Better Ways to Pay for Health Care, OECD Health Policy Studies, OECD Publishing, Paris, https://dx.doi.org/10.1787/9789264258211-en.
[36] OECD (2016), Health Workforce Policies in OECD Countries: Right Jobs, Right Skills, Right Places, OECD Health Policy Studies, OECD Publishing, Paris, https://dx.doi.org/10.1787/9789264239517-en.
[25] OECD (2015), OECD Economic Surveys: Brazil 2015, OECD Publishing, Paris, https://dx.doi.org/10.1787/eco_surveys-bra-2015-en.
[53] OECD (2014), Geographic Variations in Health Care: What Do We Know and What Can Be Done to Improve Health System Performance?, OECD Health Policy Studies, OECD Publishing, Paris, https://dx.doi.org/10.1787/9789264216594-en.
[45] OECD (2012), OECD Reviews of Health Care Quality: Israel 2012: Raising Standards, OECD Reviews of Health Care Quality, OECD Publishing, Paris, https://dx.doi.org/10.1787/9789264029941-en.
[61] OECD/The World Bank (2020), Health at a Glance: Latin America and the Caribbean 2020, OECD Publishing, Paris, https://dx.doi.org/10.1787/6089164f-en.
[70] Oliveira Hashiguchi, T. and A. Llena-Nozal (2020), “The effectiveness of social protection for long-term care in old age: Is social protection reducing the risk of poverty associated with care needs?”, OECD Health Working Papers, No. 117, OECD Publishing, Paris, https://dx.doi.org/10.1787/2592f06e-en.
[49] Policies, E. (ed.) (2019), Finland: Health system review, Health in Transition, https://apps.who.int/iris/bitstream/handle/10665/327538/HiT-21-2-2019-eng.pdf.
[76] Portal da Transparência (2019), Emendas Parlamentares, http://www.portaltransparencia.gov.br/emendas?ano=2019.
[48] Queensland Government (2018), Rural multi-purpose health services, https://www.health.qld.gov.au/clinical-practice/engagement/networks/rural-remote/rural-facilities/rural-mphs (accessed on 5 March 2021).
[19] Receita Federal (2018), Demonstrativo dos Gastos Tributários – PLOA 2019.
[9] Rocha, R., I. Furtado and P. Spinola (2019), Garantindo o Futuro da Saúde no Brasil: Neccesidades de Financiamento e Projeção de Gasatos.
[35] Scheffer, M. and E. al. (2018), Demografia Médica no Brasil 2018, Departamento de Medicina Preventiva da Faculdade de Medicina da USP, https://jornal.usp.br/wp-content/uploads/DemografiaMedica2018.pdf.
[52] Secretaria de Vigilância em Saúde (2021), Painel de Monitoramento de Nascidos Vivos, http://svs.aids.gov.br/dantps/centrais-de-conteudos/paineis-de-monitoramento/natalidade/nascidos-vivos/ (accessed on 22 January 2021).
[74] SIGA Brasil (n.d.), Saúde - Depesa Executada 2018, http://www9.senado.gov.br/QvAJAXZfc/opendoc.htm?document=senado%2Fsigabrasilpainelcidadao.qvw&host=QVS%40www9&anonymous=true&Sheet=shOrcamentoVisaoGeral.
[39] Socha, K. and M. Bech (2011), “Physician dual practice: A review of literature”, Health Policy, Vol. 102, pp. 1-7, https://doi.org/10.1016/j.healthpol.2010.10.017.
[15] Tesouro Nacional (2018), Aspectos Fiscais da Saúde no Brasil, https://www.tesourotransparente.gov.br/publicacoes/aspectos-fiscais-da-saude-no-brasil/2018/30.
[7] Thomson, S., A. Sagan and E. Mossialos (eds.) (2020), Private health insurance in Brazil, Cambridge University Press, https://doi.org/10.1017/9781139026468.
[77] Transparency International (2020), Corruption Perception Index, https://www.transparency.org/en/cpi/2020/index/bra.
[79] Transparency International (2019), Global Corruption Barometer, Latin America and the Caribbean 2019, https://www.transparency.org/files/content/pages/2019_GCB_LatinAmerica_Caribbean_Full_Report.pdf.
[78] Transparency International (2013), Global Corruption Barometer 2013, https://www.transparency.org/en/gcb/global/global-corruption-barometer-2013.
[46] Tribunal de Contas da União (2020), Hospitais públicos maiores, estaduais e da administração indireta tendem a ser mais eficientes - TC 015.993/2019-1, https://portal.tcu.gov.br/imprensa/noticias/hospitais-publicos-maiores-estaduais-e-da-administracao-indireta-tendem-a-ser-mais-eficientes.htm.
[16] Tribunal de Contas da União (2020), Sustenabilidade do Sistema Único de Saúde - TC 014.791/2019-6, https://portal.tcu.gov.br/imprensa/noticias/tcu-realiza-levantamento-sobre-a-sustentabilidade-do-sus.htm.
[58] Tribunal de Contas da União (2018), Orientações para aquisições públicas de medicamentos, República Federativa do Brasil, https://portal.tcu.gov.br/biblioteca-digital/orientacoes-para-aquisicoes-publicas-de-medicamentos.htm.
[71] Tribunal de Contas da União (2017), Relatório Sistêmico de Fiscalização - Saude 2015/2016.
[72] Vieira, F. (2019), Direito À Saúde No Brasil: Seus Contornos, Judicialização E A Necessidade Da Macrojustiça, https://www.ipea.gov.br/portal/images/stories/PDFs/TDs/td_2547.pdf.
[13] Vieira, F. and R. de Sá e Benevides (2016), “O Direito à Saúde no Brasil em Tempos de Crise Econômica, Ajuste Fiscal e Reforma Implícita do Estado”, Revista de Estudos e Pesquisas sobre as Américas, Vol. 10/3, https://doi.org/10.21057/repam.v10i3.21860.
[12] Vieira, F., S. Piola and R. de Sá e Benevides (2019), Vinculação Orçamentária do Gasto em Saúde no Brasil: Resultados e Argumentos, https://saudeamanha.fiocruz.br/wp-content/uploads/2019/10/td_2516.pdf.
[73] Wang, D. et al. (2020), “Health technology assessment and judicial deference to priority-setting decisions in healthcare: Quasi-experimental analysis of right-to-health litigation in Brazil”, Social Science & Medicine, Vol. 265, https://doi.org/10.1016/j.socscimed.2020.113401.
[51] WHO (2015), WHO Statement on Caesarean Section Rates, https://www.who.int/reproductivehealth/publications/maternal_perinatal_health/cs-statement/en/.
[57] WHO (1999), Operational principles for good pharmaceutical procurement, https://www.who.int/3by5/en/who-edm-par-99-5.pdf.
[22] WHO and World Bank (2019), Global Monitoring Report on Financial Protection in Health 2019, https://www.who.int/publications/i/item/global-monitoring-report-on-financial-protection-in-health-2019.
[2] WHO Global Heallth Expenditure Database (2020), , https://apps.who.int/nha/database.
[21] WHO Regional Office for Europe (2019), Can people afford to pay for health care? New evidence on financial protection in Europe.
[26] World Bank (2017), A fair adjustment : efficiency and equity of public spending in Brazil : Volume I : síntese (Portuguese), World Bank Group, http://documents.worldbank.org/curated/en/884871511196609355/Volume-I-síntese.
Notes
← 1. Public health financing refers to health spending by health care schemes with automatic or compulsory coverage.
← 2. 3% of all health spending in Brazil can currently not be allocated to any financing scheme.
← 3. The United States has also an important private insurance market but with the Affordable Care Act, the purchase of private coverage became compulsory as of 2014 (but this mandate was repealed in 2018).
← 4. But given that 3% of total health spending can currently not be allocate to a financing scheme, the real share of OOP spending may be higher.
← 5. Voluntary private duplicate insurance provides health insurance coverage for a range of services that are also available from public coverage but expands the list of (mainly private) providers. Supplementary insurance coverage provides access to services not covered by the public benefit package.
← 6. Dental services may also be included as one element of the medical insurance policies.
← 7. Employers can deduct the premium payments they make from corporate taxation.
← 8. The fact that under the “Healthy Ageing” scenario the projected health spending increase is much more limited makes a powerful argument to strengthen public health measures as discussed in Chapter 5 and Chapter 6.
← 9. If anything, the COVID-19 pandemic has amplified these challenges.
← 10. A recent public spending review of the World Bank has found many more areas where public funds could be used more efficiently (World Bank, 2017[26]) but listing them all here would go beyond the scope of this chapter.
← 11. The United States is not considered here since it is difficult to distinguish between compulsory and voluntary private insurance in that country.
← 12. There may be some overlap between the two population groups but medical coverage may also include dental coverage depending on the individual plan.
← 13. Figure refer to the average value of 2010-14.
← 14. Taken together, general outpatient care, dental care, home-based curative care and prevention are classified as “basic care” services in health spending statistics of the OECD. This can be taken as a proxy for primary health care (a more meaningful analysis would also take the location of service provision into account but limitations in international health spending data from Brazil does not allow for this analysis at the moment). At any rate, the international comparison of primary care spending is challenging due to differing notions of what services primary care entail as well as data issues (OECD, 2018[84]). Moreover, since 4% of all health services are unallocated in Brazil the share dedicated to basic care services may actually be higher.
← 15. For international comparisons, the number of practicing physicians is typically used. The number of registered physicians is overestimating the number of practicing physicians.
← 16. The ratio is calculated by dividing all primary care related consultations per year registered in SUS by the total population. The number of total medical consultations including GPs and specialists and the private sector for SUS users was estimated at 4.0 in 2017 by the Federal Court of Accounts (Tribunal de Contas da União, 2020[16]) with substantial variation across states.
← 17. This problem is, however, typically more pertinent in specialist care than in primary care.
← 18. It should be noted, however, that in most countries the bottleneck in treating severe COVID-19 cases was the availability of ICU beds, ventilators, oxygen and ICU staff and not regular hospital beds.
← 19. In addition, patients have access to pharmaceuticals that are used as part of an inpatient treatment. They are not included in ‘Rename’ and their costs are covered through the hospital budget.
← 20. Similares are copies of off-patent originator products that – depending on the country- may be approved without demonstration of bioequivalence and that can be marketed with a brand name. In Brazil, new similares have to prove bioequivalence since 2003 and they can hence be considered as branded generics.
← 21. In Brazil, in terms of volume, 34% of the market are unbranded generics and 44% branded generics (reflecting 28% and 41% of value, respectively)
← 22. ADL refer to activities such as getting out of bed, dressing, personal hygiene and moving around while IADL refer to activities such as shopping, cleaning the house or preparing meals.
← 23. This share may in fact even be higher since 4% of all health spending in Brazil are unallocated and may include some administrative activities.
← 24. At the moment Brazil has 438 health regions and 118 macroregions.
← 25. A high number of judicial cases, however, also exists for care in the private health sector.
← 26. Available data for more recent years suggest a decrease in the costs of “judicial spending” for pharmaceuticals in 2017 (Vieira, 2019[72]).
← 27. In this context, it should be highlighted that with nearly 1.4% of GDP, Brazil spends between three and six times the resources on its judiciary system than most European countries (OECD, 2020[11]).
← 28. Function and processes of CONITEC are similar to those seen by HTA authorities in Australia, Canada and the United Kingdom, countries generally considered as having advanced HTA processes (Lima, de Brito and de Andrade, 2019[83]).
← 29. Law 12 401/2011 creates CONITEC and defines its competence. Even Article 196 of the constitution could be interpreted in a way that the “right to health for all” is under reservation, since it also mentions “economic policies” as a lever to guarantee this right. Improving the cost-effectiveness of SUS resources is an example of an economic policy.
← 30. With the first place going to the country with the least perceived corruption.
← 31. Sunshine regulations consist of requiring that payments made by pharmaceutical and device industries to stakeholders in the health sector be systematically reported to authorities.
← 32. Private patients may however pay additional fees for better amenities or visits by the head of department.