Financial hardship and out-of-pocket expenditure
Where health systems fail to provide adequate financial protection, people may suffer financial hardship from paying for health care, or simply not have enough money to pay for health care. As a result, lack of financial protection can reduce access to health care, undermine health status, deepen poverty and exacerbate health and socio-economic inequalities. On average across OECD countries, just over one-fifth of all spending on health care comes directly from patients through out-of-pocket (OOP) payments (see indicator “Financing of health care” in Chapter 7). People experience financial hardship when the burden of such OOP payments is large in relation to their ability to pay. Poorer households and those who have to pay for long-term treatment – such as medicines for chronic illness – are particularly vulnerable.
The share of household consumption spent on health care provides an aggregate assessment of the financial burden of OOP expenditure. Across OECD countries in 2019, about 3% of total household spending was on health care goods and services, from around 2% or below in New Zealand, France, Slovenia, Luxembourg, Colombia and Turkey to more than 5% in Korea and Switzerland (Figure 5.8).
Health systems in OECD countries differ in the degree of coverage for different health goods and services (see indicator “Extent of health care coverage”). Pharmaceuticals and other medical goods made up the main OOP expense for people in 2019, followed by spending on outpatient care (Figure 5.9). These two components typically account for almost two-thirds of household spending on health care. Average household OOP spending on dental care (14% of spending on health) and long-term health care (12%) can also be high. Inpatient care plays only a minor role (9%) in the composition of OOP spending. During the COVID-19 pandemic, countries have tried to ensure that diagnosis, testing and appropriate care for COVID-19 patients are affordable – notably in countries where segments of the population remain without coverage (OECD, 2021[6]).
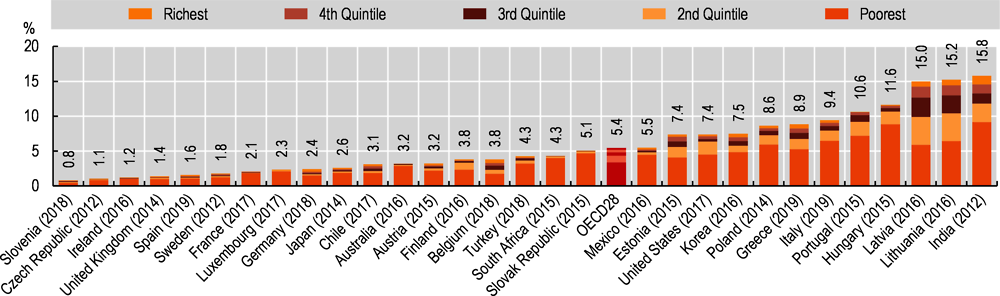
The indicator most widely used to measure financial hardship associated with OOP payments for households is incidence of catastrophic spending on health (Cylus, J., Thomson and Evetovits, 2018[8]). This varies considerably across OECD countries, from fewer than 2% of households experiencing catastrophic health spending in Sweden, Spain, the United Kingdom, Ireland, the Czech Republic and Slovenia, to over 10% of households in Lithuania, Latvia, Hungary and Portugal (Figure 5.10). Across all countries, poorer households (those in the lowest consumption quintile) are most likely to experience catastrophic health spending, despite the fact that many countries have put in place policies to safeguard financial protection.
Countries with comparatively high levels of public spending on health and low levels of OOP payments typically have a lower incidence of catastrophic spending. However, policy choices are also important, particularly around coverage policy (WHO Regional Office for Europe, 2019[9]). Population entitlement to publicly financed health care is a prerequisite for financial protection, but not a guarantee of it. Countries with a low incidence of catastrophic spending on health are also more likely to exempt poor people and frequent users of care from co-payments; use low fixed co-payments instead of percentage co-payments, particularly for outpatient medicines; and cap the co-payments a household has to pay over a given time period (as, for example, in Austria, Ireland and the United Kingdom).
Out-of-pocket (OOP) payments are expenditures borne directly by a patient where neither public nor private insurance cover the full cost of the health good or service. They include cost-sharing and other expenditure paid directly by private households, and should also ideally include estimations of informal payments to health providers.
Catastrophic health spending is an indicator of financial protection used to monitor progress towards universal health coverage. It is defined as OOP payments that exceed a predefined percentage of the resources available to a household to pay for health care. Household resources available can be defined in different ways, leading to measurement differences. In the data presented here, these resources are defined as household consumption minus a standard amount representing basic spending on food, rent and utilities (water, electricity, gas and other fuels). The threshold used to define households with catastrophic spending is 40%. Microdata from national household budget surveys are used to calculate this indicator.