Screening, survival and mortality for breast cancer
Breast cancer is the most frequent cancer among women across EU countries, with more than 400 000 cases diagnosed each year across EU countries (see indicator “Cancer incidence” in Chapter 3). The main risk factors for breast cancer are age, genetic predisposition, oestrogen replacement therapy, and lifestyle factors including obesity, physical inactivity, nutrition habits and alcohol consumption.
Most European countries have adopted breast cancer screening programmes as an effective way for detecting the disease early (OECD, 2013; IARC, 2017). However, due to recent progress in treatment outcomes and concerns about false-positive results, over-diagnosis and overtreatment, breast cancer screening recommendations have been re-evaluated in recent years. WHO now recommends organised population-based mammography screening for women aged between 50 and 69 in EU countries, if specific criteria are met such as whether women are able to make an informed decision based on the benefits and risks of mammography screening. Other criteria are related to quality assurance and monitoring and evaluation mechanisms (WHO, 2014).
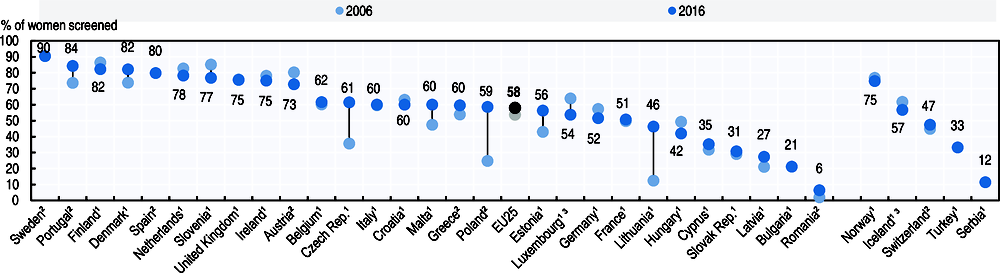
The proportion of women in the EU aged 50-69 who have been screened for breast cancer within the past two years is lowest in Romania, Bulgaria and Latvia, and highest in Nordic countries (Sweden, Finland and Denmark) and Portugal (Figure 6.19). On average across EU countries, the proportion of screened women increased from 54% to 58% between 2006 and 2016. A large increase has occurred in some countries that had a low screening rate a decade ago, such as Lithuania, Poland and the Czech Republic. However, breast cancer screening rate has decreased substantially over the past decade in several countries, likely due partly to concerns over potential harms related to mammography screening, although a number of studies have found that the benefits overweigh the potential risks (IARC, 2015).
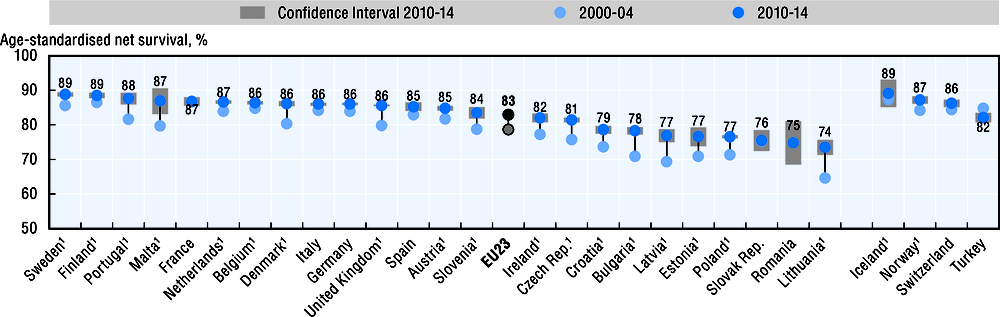
Breast cancer survival reflects early diagnosis as well as effective treatment. All Western European countries have attained five-year net survival of at least 80%, but survival is still lower in several Central and Eastern European although it has increased in recent years (Figure 6.20).
Over the last decade, the five-year net survival improved from 79% to 83% on average across EU countries. Net survival increased particularly rapidly in Bulgaria, the Czech Republic, Estonia, Latvia and Lithuania, converging towards the level of other EU countries. In the Czech Republic, survival improved following the introduction of a breast cancer screening programme and a National Cancer Control Programme in the early 2000s (OECD, 2014). Survival also increased strongly in Denmark, Malta, Portugal and the United Kingdom.
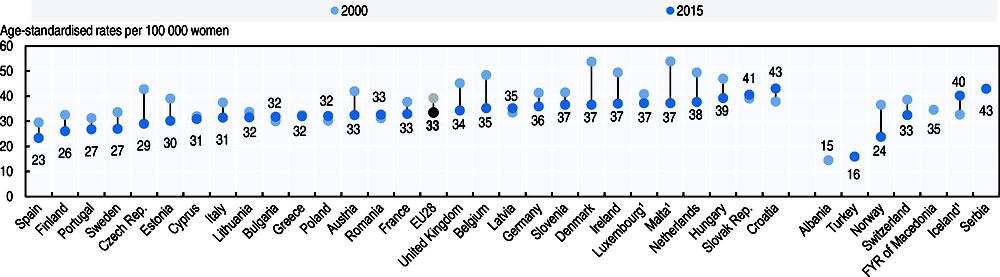
Mortality from breast cancer has fallen in most EU countries since 2000. On average across EU countries, the age-standardised rates of mortality from breast cancer fell from 39 to 33 per 100 000 women per year between 2000 and 2015 (Figure 6.21). Particularly strong reductions occurred in Denmark and Malta, although these countries still have higher age-standardised mortality rates. Croatia is one of the few EU countries where breast cancer mortality rate has increased since 2000 and now has the highest mortality rates of all EU countries.
Screening coverage and survival are defined in the indicator “Screening, survival and mortality for cervical cancer”. Survival estimates for breast cancer are based on the International Classification of Diseases for Oncology (ICD-O-3 C50.0-C50.6 and C50.8-C50.9). See indicator “Mortality from cancer” in Chapter 3 for the definition of cancer mortality rates. Mortality from breast cancer is based on ICD-10 C50.
References
IARC (2015), “IARC Handbooks of Cancer Prevention: Benefits of mammography screening outweigh adverse effects for women aged 50-69 years”, Press release No. 234, Lyon, www.iarc.fr/en/media-centre/pr/2015/pdfs/pr234_E.pdf.
IARC (2017), Cancer Screening in the European Union – Report on the implementation of the Council Recommendation on cancer screening, European Commission, Brussels, https://ec.europa.eu/health/sites/health/files/major_ chronic_diseases/docs/2017_cancerscreening_2ndreport implementation_en.pdf.
OECD (2013), Cancer Care: Assuring Quality to Improve Survival, OECD Publishing, Paris, https://doi.org/10.1787/9789264181052-en.
OECD (2014), OECD Reviews of Health Care Quality: Czech Republic 2014: Raising Standards, OECD Publishing, Paris, https://doi.org/10.1787/9789264208605-en.
WHO (2014), WHO Position Paper on Mammography Screening, WHO, Geneva.