Chapter 1. Promoting mental health in Europe: Why and how?
Good mental health is a critical part of individual well-being, and the foundation for happy, fulfilled, productive lives. However, this chapter finds that more than one in six people across EU countries had a mental health problem in 2016. Living with mental ill-health means that individuals are less able to succeed at school and work, are more likely to be unemployed, and may suffer worse physical health. For some, mental illnesses lead to premature mortality: over 84 000 people died of mental health problems and suicides across EU countries in 2015.
The economic costs of mental illness are also significant. This chapter estimates total costs related to mental ill-health at more than 4% of GDP – or over EUR 600 billion – across the 28 EU countries in 2015. EUR 190 billion (or 1.3% of GDP) is direct spending on health care, another EUR 170 billion (1.2% of GDP) is spending on social security programmes, while a further EUR 240 billion (1.6% of GDP) is caused by indirect costs in the labour market, driven by lower employment rates and reduced productivity due to mental illness.
The heavy economic, social and individual burden of mental illness is not inevitable, and more must be done to prevent and treat mental disorders, and to foster good mental health. The latter part of this chapter explores some effective ways by which European countries are promoting mental well-being and preventing mental illness, and identifies critical gaps where more action is needed.
Introduction
Good mental health is a critical part of individual well-being, and the foundation for happy, fulfilled, productive lives. Mental ill-health, meanwhile, will affect everyone at some point in their lives – whether experiencing mental illness themselves, or as a family member, friend or colleague of someone living with a mental disorder. Mental ill-health can affect women and men of all ages and backgrounds. Without effective prevention and treatment, mental illnesses can have profound effects on people’s ability to carry out their daily lives and often result in poorer physical health. The impact of poor mental health can affect people throughout their lifetime. Children and adolescents with poor mental health have worse educational outcomes and job opportunities. Adults with mental health problems are less productive at work and more likely to be unemployed. Elderly people with mental problems are more likely to be isolated and be less active in their community.
Mental health problems cover a wide range of illnesses, including disorders such as mild or moderate anxiety and depression, drug and alcohol use disorders, and severe disorders such as severe depression, bipolar disorders and schizophrenia. Comorbidity of mental disorders and physical illnesses, and multiple mental health problems, is common. Some mental disorders may affect individuals for only a short time, while others affect individuals their entire life. Mental health problems often result from a complex interplay of many factors, including genetic, social and economic factors, and can be provoked or worsened by behavioural and environmental factors such as alcohol and drug abuse, poverty and debt, trauma, or physical ill-health.
The burden of mental health problems in Europe is very high, both in terms of morbidity and mortality. Tens of millions of people across the EU experience at least one mental health problem at any point in time, and tens of thousands die each year either directly from mental health disorders or from suicide (which in many cases are linked to mental health problems, although other factors can also play a role). The economic burden, too, is significant. This chapter estimates total costs related to mental ill-health at more than 4% of GDP – or over EUR 600 billion – across the 28 EU countries in 2015. EUR 190 billion (or 1.3% of GDP) is direct spending on health care, another EUR 170 billion (1.2% of GDP) is spending on social security programmes, while a further EUR 240 billion (1.6% of GDP) is caused by indirect costs in the labour market, driven by lower employment rates and reduced productivity due to mental illness.
In response to the health and economic impact of mental illness, European countries are taking actions to both prevent and treat mental illness when it occurs. The economic, societal and individual burden of mental illness is not a foregone conclusion – many interventions exist which can lessen the impact of mental ill-health. While the latter part of this chapter focuses mainly on effective interventions to prevent mental illness and promote mental well-being, improving access to early diagnosis, care and treatment for mental health conditions when they arise remains critical.
Carefully chosen and well-implemented actions to promote better mental health and prevent mental ill-health can lead to significant benefits over time, for individuals and their families, for society, and for economies. Cost-effective and sometimes even cost-saving interventions can help strengthen the mental well-being and resilience of mothers and infants, school-age children, workers, and older populations.
The widely used definition established by the WHO emphasises the positive dimension that “mental health is a state of well-being in which the individual realises his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her community” (WHO, 2001). The terms mental health and mental well-being in this chapter draw on this WHO definition of positive mental health.
Mental illness is the loss of mental health due to a mental disorder. Mental disorders are defined as those reaching the clinical threshold of a diagnosis according to psychiatric classification systems including disorders such as depression, anxiety, bipolar disorder and schizophrenia. In this chapter, mental illnesses will generally comprise all those included in Chapter 5 of the International Classification of Diseases (ICD-10) on mental and behavioural disorders with the exception of dementia (which is considered, along with Alzheimer’s disease, the main form of dementia, as a neurological disorder). The broad terms “mental ill‐health”, “mental illness” and “mental health problems” are used interchangeably and refer to mental disorders but also include psychological distress, i.e. symptoms or conditions that do not reach the clinical threshold of a diagnosis within the classification systems but which can account for significant suffering and hardship, and can be enduring and disabling.
Mental illness affects tens of millions of Europeans every year
Mental health problems affect about 84 million people across EU countries
Although there are significant gaps in information about the prevalence of mental health problems across EU countries, all available evidence suggests that mental health problems affect tens of millions of Europeans every year. The data currently available from population-based surveys are often limited to a few specific mental health disorders, or specific age groups. However, the Institute for Health Metrics and Evaluation (IHME) provides estimates of the prevalence of a wide range of mental health disorders across all age groups based on a wide variety of data sources and a set of assumptions
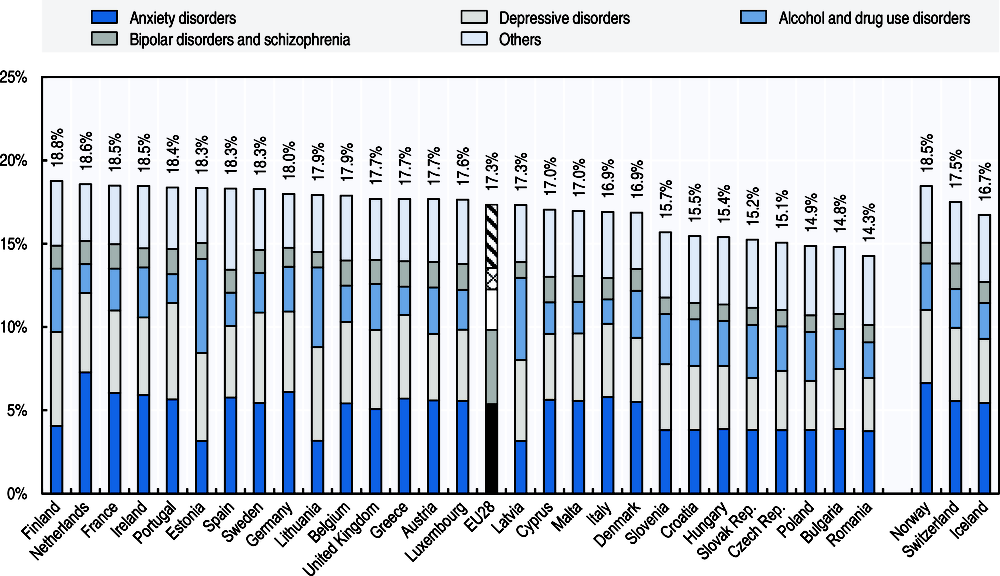
According to the latest IHME estimates, more than one in six people across EU countries (17.3%) had a mental health problem in 2016 (Figure 1.1) – that is, nearly 84 million people.1 The most common mental disorder across EU countries is anxiety disorder, with an estimated 25 million people (or 5.4% of the population) living with anxiety disorders, followed by depressive disorders, which affect over 21 million people (or 4.5% of the population). An estimated 11 million people across EU countries (2.4%) have drug and alcohol use disorders. Severe mental illnesses such as bipolar disorders affect almost 5 million people (1.0% of the population), while schizophrenic disorders affect another estimated 1.5 million people (0.3%).
By country, the estimated prevalence of mental health disorders is highest in Finland, the Netherlands, France and Ireland (with rates of 18.5% or more of the population with at least one disorder), and lowest in Romania, Bulgaria and Poland (with rates of less than 15% of the population). Some of these cross-country differences may be due to the fact that people living in countries with greater awareness and less stigma associated with mental illness, as well as easier access to mental health services, may be diagnosed more easily or may be more likely to self-report mental ill-health. In many countries, there is still strong stigma associated with various mental health problems, and in some countries this stigma sits alongside a still-widespread belief that it is better to simply avoid talking about mental illness (Munizza et al., 2013).
Several mental illnesses are more common amongst women, including anxiety disorders, depressive disorders and bipolar disorders. Some of these gender gaps may be due to a greater propensity of women to report these problems. However, one exception is drug and alcohol use disorders, which are more than two times more likely to occur in men than women on average across EU countries (IHME, 2018).
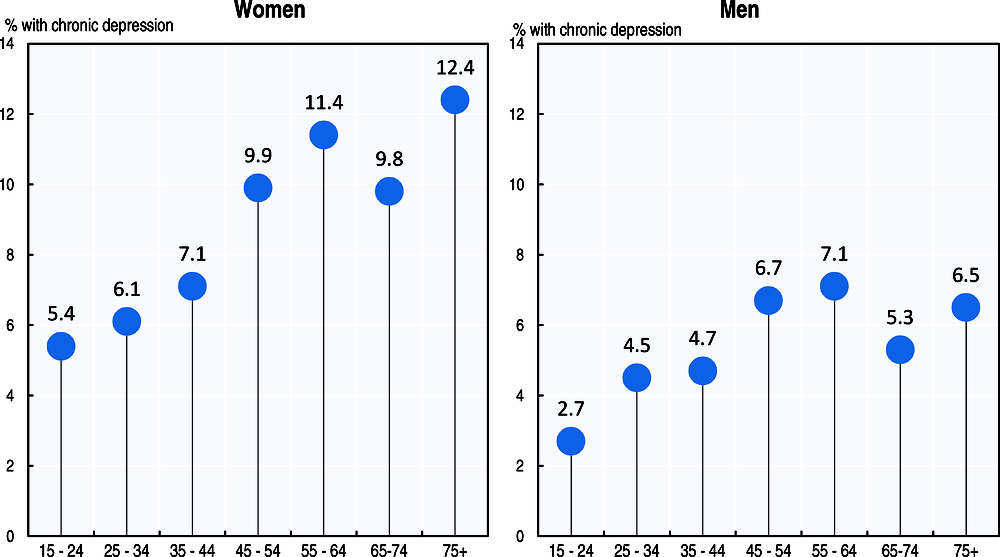
Data from the 2014 European Health Interview Survey confirm a substantial gender gap in self-reported chronic depression, with more than one in twelve women (8.8%) indicating they experience chronic depression, compared with one in nineteen men (5.3%). The prevalence of chronic depression increases steadily with age among both women and men, and is particularly high in middle age (Figure 1.2). At age 55-64, more than 11.4% of women and 7.1% of men reported being chronically depressed across the EU as a whole in 2014. These rates decrease between the age 65 and 74, and then increase again in older ages. This increase in older ages may be partly explained by the fact that depression is often associated with poor physical health, frailty, perceived financial strain and lower social support (Grundy, van den Broek and Keenan, 2017).
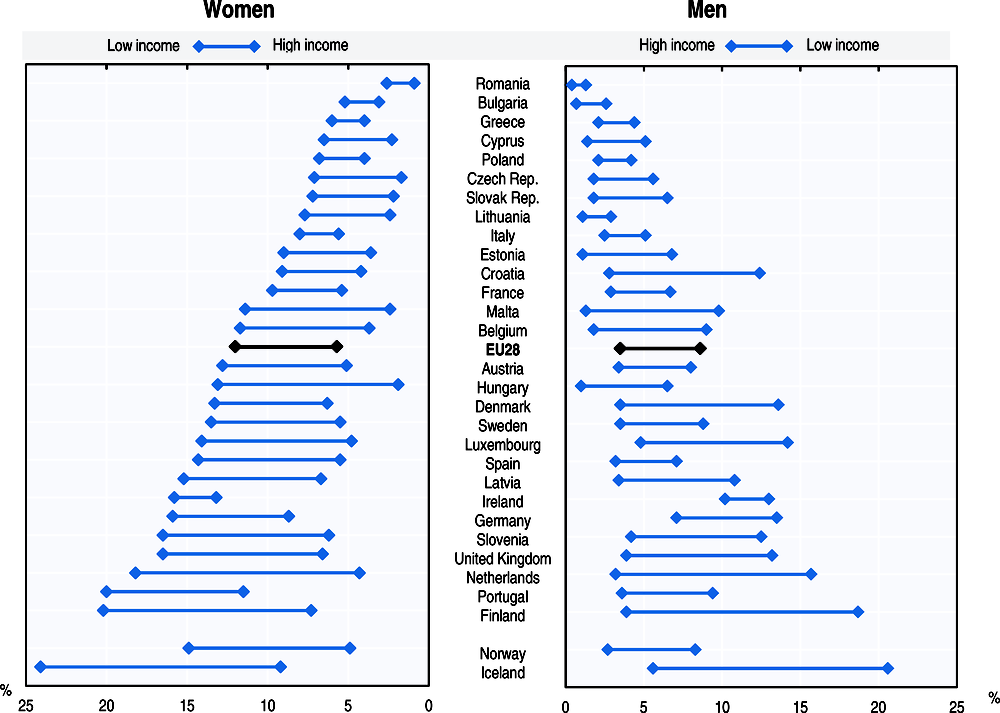
By level of education, people with at most lower secondary educational attainment are almost two-times more likely to report chronic depression compared to those with higher educational level. This is also the case for people in low-income groups. On average across EU countries, women and men living in the lowest income group are more than two times more likely to report chronic depression than those in the highest income group (Figure 1.3).
People who are employed generally report lower levels of depression than those who are not, and people with a mental disorder are more likely to be unemployed (OECD, 2015). People with depression or other mental health problems often see improvement in their condition after finding work, as their labour-force status increases their self-esteem and sense of worth in society, and losing a job generally contributes to worsened mental health (OECD, 2018).
A considerable number of children experience mental health problems which, unless they receive appropriate care and support, may have a lasting effect throughout their lives. Evidence suggests that many mental disorders begin at adolescence or even younger; most studies find that roughly half of all lifetime mental disorders start by the mid-teens (Kessler et al., 2007).
A 2010 study found that in five of the six EU countries covered (Bulgaria, Germany, Lithuania, the Netherlands and Romania), 10% to 15% of children aged 6-11 years old experience at least one mental health or behavioural disorder (i.e. conduct disorder, emotional disorder, hyperactivity or inattention disorder). Italy is the only country where prevalence was less than 10%, but about 8% of children still had a mental or behaviour disorder (Kovess-Masfety et al., 2016).
Mortality related to mental health problems and suicides is substantial
Over 84 000 people died of mental health problems and suicides across EU countries in 2015, and this is an under-estimation as many people with mental health problems also die prematurely because of higher rates of physical health problems and chronic diseases that are not properly treated. “Excess mortality” for mental disorders – the gap between the mortality rate of the general population and the mortality rate for people with a mental disorder – is huge. For example, excess mortality amongst women who have been diagnosed with schizophrenia is above 6 in Finland, Norway and Sweden (OECD, 2018). Persons with severe mental illness die 10-20 years earlier than the general population (Liu et al., 2017; OECD, 2014; Coldefy and Gandré, 2018).
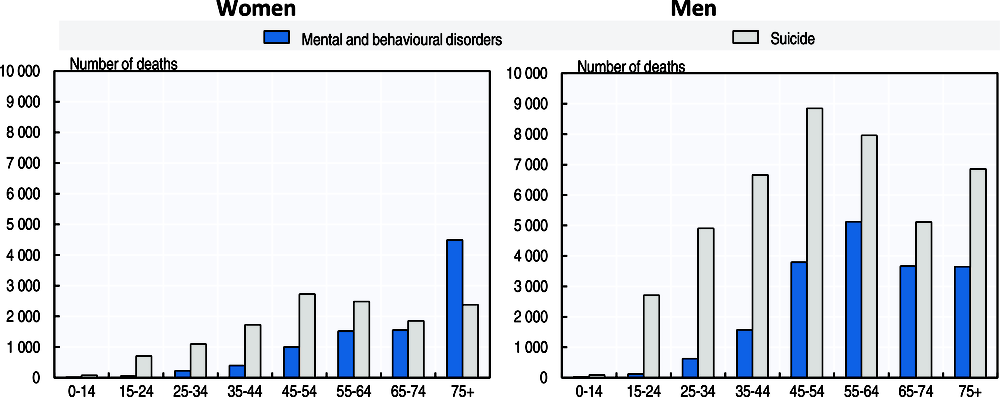
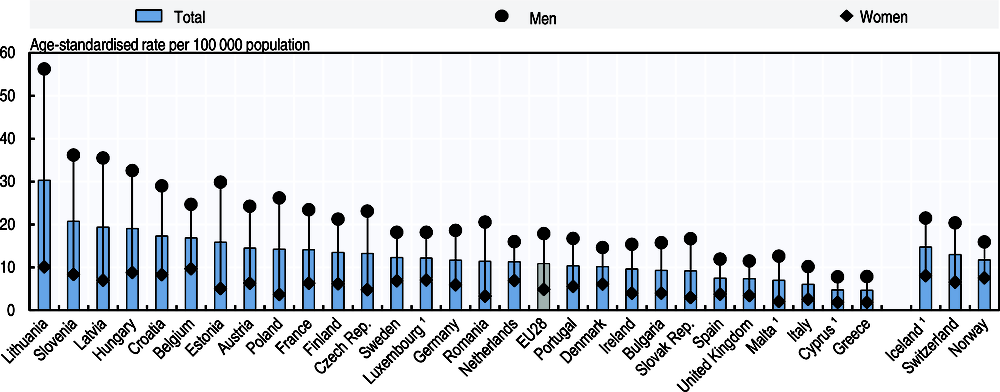
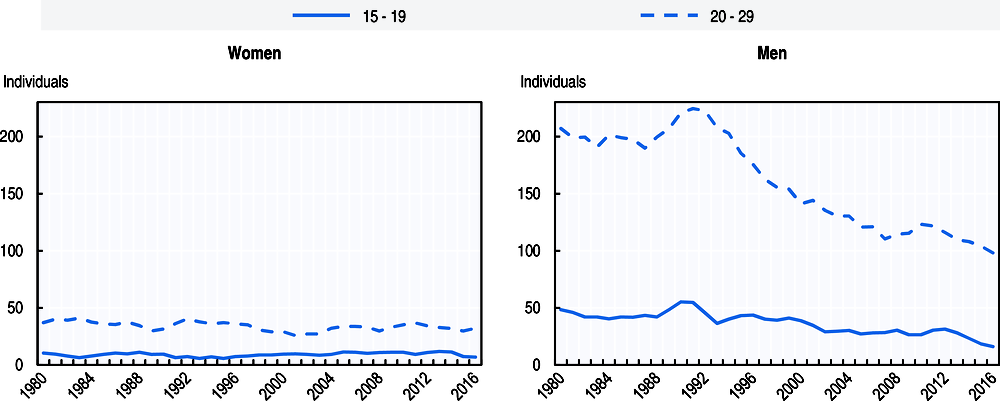
Of the 84 000 deaths directly related to mental health problems and suicides, most of these deaths were among men, mainly because of higher suicide rates among men (Figure 1.4). Some 43 000 men in EU countries died from suicide in 2015, compared with 13 000 women. However, the gender gap in suicide attempts is much smaller or even reversed in some countries, because women often use less fatal methods. For example, in France, while the completed suicide rate is more than three times greater among men than women, hospital discharge rate for suicide attempts was 52% greater among women in 2015 (Observatoire national du suicide, 2018). Many different factors may explain why some people are led to attempt or complete suicide, including major life events (such as the death of a loved one, a divorce or employment loss), social isolation, or socioeconomic or cultural context. However, a high proportion of people who have survived a suicide attempt or died from suicide have experienced a mental health disorder (Hoven, Mandell and Bertolote, 2010; Cavanagh et al., 2003; WHO, 2014). A cross-national analysis based on the WHO World Mental Health Surveys found that a wide range of mental disorders increased the odds of experiencing suicidal thoughts, and a smaller number of disorders increased the odds of acting on such thoughts (Nock et al., 2009).
The number of suicides increases steadily with age among both men and women, reaching a peak among 45-64 years-olds (Figure 1.4). Between ages 65 and 74 the number of suicides decreases at least slightly.
By country, the suicide rate among the population of all ages is highest, by far, in Lithuania, with (age-standardised) rates of 30 deaths per 100 000 population in 2015. Slovenia, Latvia and Hungary also have high rates at around 20 deaths per 100 000 population, which is almost two times greater than the EU average (11 per 100 000 population). The lowest rates are reported in Southern European countries (Greece, Cyprus, Italy, Malta and Spain) (Figure 1.5). Some caution is required in interpreting suicide rates as these may reflect, at least in part, differences in recording practices. On average across all countries, the suicide rate among men was 3.7 times greater than among women. This gender gap was largest in the four countries with the highest rate, but also in Estonia, Poland and Romania.
Despite the relatively low absolute number of suicides among younger age groups, suicide is nonetheless one of the leading causes of death among adolescents and young adults. Some 3 400 young people age 15-24 died from suicide in EU countries in 2015, making this the main cause of death in this age group after road traffic injuries. Young people are more likely to attempt suicide if they have a family history of alcohol and drug abuse disorders, have access to firearms, and experience difficult life events at school or at home (McLoughlin, Gould and Malone, 2015). However, it is heartening to note that suicide rates among teenagers have decreased by 20% on average across EU countries between 2000 and 2015. There has been a notable decrease in Finland, reflecting the success of suicide prevention campaigns targeting this age group (see Box 1.5).
The costs of mental health problems exceed 4% of GDP
The total costs of mental health problems on EU economies are huge, highlighting the need for greater efforts to prevent mental ill-health and to provide timely and effective treatments when it occurs. Besides the costs on health care systems, mental health problems also result in substantial costs in terms of social security benefits as well as negative labour market impacts in terms of reduced employment and productivity. This section provides estimates of the direct and indirect costs related to mental illnesses across EU countries, using different data sources and based on a set of explicit assumptions where necessary (see Box 1.2).
In 2015, the overall costs related to mental ill-health are estimated to have exceeded 4% of GDP across the 28 EU countries. This equates to more than EUR 600 billion. This total breaks down approximately into the equivalent of 1.3% of GDP (or EUR 190 billion) in direct spending on health systems, 1.2% of GDP (or EUR 170 billion) on social security programmes, and a further 1.6% of GDP (or EUR 240 billion) in indirect costs related to labour market impacts (lower employment and lower productivity). Despite these costs being considerable, they are still a significant under-estimate, as several additional costs have not been taken into account. These include, in particular, social spending related to mental health problems, such as higher social assistance benefits and higher work-injury benefits, and the higher cost of treating a physical illness if the patient also has a mental illness. In addition, some of the indirect impacts of mental health problems on labour market participation such as reduced employment rates or working hours for informal caregivers taking care of people with mental health problems or the impact on co-workers, have not been taken into account.
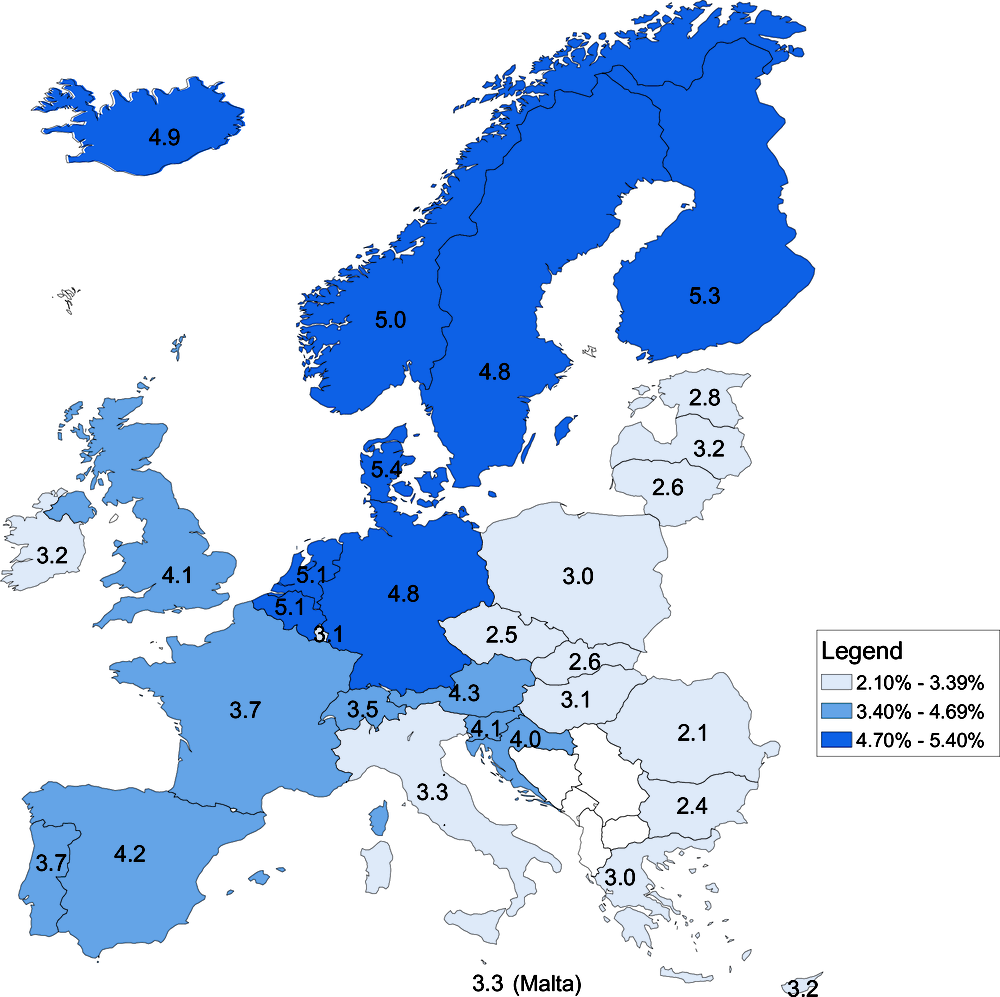
By country, the estimated costs related to mental health problems range from 2% to 2.5% of GDP in Romania, Bulgaria and the Czech Republic, to over 5% of GDP in Denmark, Finland, the Netherlands and Belgium (Figure 1.6). These variations are mainly driven by the share of people reporting mental health problems (which may be under-estimated in countries where there is a strong stigma associated with mental health problems) as well as differences in the social security benefits provided to people with mental health problems (in terms of paid sick leave benefits, disability benefits and unemployment insurance benefits), and different levels of spending on mental health care services.
Table 1.2 below summarises the different categories of direct and indirect costs that have been considered in the analysis in this chapter, along with the main data sources used. The direct costs include both those borne by health care systems to provide treatments to mental health problems and additional social security spending, including paid sick leave benefits, disability benefits and unemployment insurance benefits. The indirect costs relate to the labour market impact of mental health problems, and include both lower employment rates for people with mental health problems and lower productivity due to higher absenteeism and lower productivity when at work (“presenteeism”).
Estimates of direct health care costs are based on a selection of mental health conditions contained in a previous study on the cost of disorders of the brain in Europe (Gustavsson et al., 2011). The original cost estimates have been extrapolated to 2015 using recent health spending data and updated macroeconomic data. Overall estimates have also been corroborated with country-specific health expenditure by disease studies such as the Eurostat Health Expenditures by Diseases and Conditions study in 2016. The assumption has been made that the share of mental health spending remained constant between 2010 and 2015.
The main data sources for the estimates on social security benefits are the Eurostat Database, the European Working Conditions Survey, and national data sources. The following assumptions have been made to fill data gaps on the share of social security spending related to mental health problems for countries that did not have the required data readily available: 1) 20% of paid sick leave benefits are related to mental health problems, based on the available evidence from Sweden (OECD, 2012); 2) 37% of disability benefits are related to mental health problems, based on the available evidence from six countries (Austria, Belgium, Denmark, Netherlands, Sweden, United Kingdom) (OECD, 2015) and 3) 15% of unemployment insurance benefits are related to mental health problems, based on the evidence from the same group of six countries that about 30% of people on average who are receiving unemployment insurance benefits also report some mental health problems, but assuming that mental health problems are the leading cause for unemployment for half of these people only.
The labour market impact of mental health problems draws also on the Eurostat Database and the European Working Conditions Survey. The approach used to measure the negative employment effect of mental health problems is to assume that people with mental health problems would have had the same employment rate as the rest of the population, and earn the same salary, using the median wage in the economy. The productivity effect is measured by looking at both absenteeism and “presenteeism”. The latter is based on a study that has found that both blue-collar and white-collar workers experiencing mental ill-health are about 6% less productive than those without such problems (Hilton et al., 2008). The assumption is made that this lower productivity at work is reflected in lower wages.
The costs throughout the analysis are expressed in euros without any adjustment for variations in the cost of living (no adjustment for purchasing power parity).
Direct costs of mental health problems on health systems and social security benefits
A sizeable share of health spending goes towards mental health problems
Spending on the provision of mental health services is estimated to have accounted for about 13% of health spending across EU countries in 2015. This is less than spending on circulatory diseases – the number one cause of mortality in the EU – but similar to spending on cancer care in many countries.
This equals 1.3% of GDP or around EUR 194 billion of direct health care spending on a broad range of mental health conditions across the EU. This covers spending on the health services and goods related to the prevention, diagnosis and treatment of mental health disorders (including physician visits, hospitalisations and pharmaceuticals).
This spending reaches an estimated 1.4% of GDP in Germany and the United Kingdom. At the lower end, in addition to Luxembourg at 0.8% and Ireland at 0.9%, Lithuania, Bulgaria, Romania and the Slovak Republic are all estimated to have spent less than 1% of GDP on direct health care services for mental health.
Mental health problems result in much higher sickness benefits, disability benefits and unemployment insurance benefits
The direct costs of mental ill-health extend well beyond the health system; mental illness leads to substantial additional spending in many social security programmes, including paid sick leave benefits, disability benefits and unemployment insurance benefits.
Expenditure on disability benefits accounts for the bulk of mental health-related social spending. It is estimated that mental health problems accounted for EUR 112 billion in disability benefits across the EU as a whole in 2015 (or 0.76% of GDP). Paid sick leave benefits related to mental health problems accounted for another EUR 28 billion (or 0.19% of GDP) in 2015, whereas unemployment insurance benefits were estimated to add another EUR 29 billion (or 0.20% of GDP).
As already noted, these estimated costs of mental health problems on social spending are an under-estimation as they do not include the cost of other social programmes, such as social assistance benefits or lone-parent benefits.
Indirect costs of mental health problems on employment and productivity
Beyond the direct costs to health systems and social security benefits, mental ill-health also contributes to substantial indirect costs, primarily related to reduced labour market participation and productivity. These indirect costs include not only lower employment rates for people with mental health problems, but also reduced productivity due to higher absenteeism and lower productivity at work (often referred as “presenteeism”). These costs add up to over EUR 240 billion or 1.6% of GDP across EU countries in 2015.
Lost income and employment due to mortality from mental health problems and suicide is estimated at EUR 22 billion per year across EU countries
Over 50 000 premature deaths among the working-age population (people aged 25-64) were due to mental health problems and suicide across EU countries in 2015. Assuming that all those people who died prematurely would have been employed until age 65 at the same employment rate as the rest of the population, the associated potential loss for the economy is estimated to be about 640 300 potentially productive life years across EU countries. Assuming that these people would have earned the median income in each country, this amounts to EUR 22 billion in potential income loss each year, or 0.15% of GDP across the EU as a whole.
This loss in income as a share of GDP was particularly large in Slovenia, Belgium, Latvia and Lithuania, mainly because of higher suicide rates.
Lost income due to lower employment rate of people with depression is estimated at EUR 176 billion per year across EU countries
Living with mental health problems has an impact on people’s daily lives, including their ability to work. Mental health problems often impede an individual’s ability to participate in the labour market which can lead to a “vicious” circle whereby the longer people are out of work, the more damaging the consequences are for their mental health (OECD, 2014).
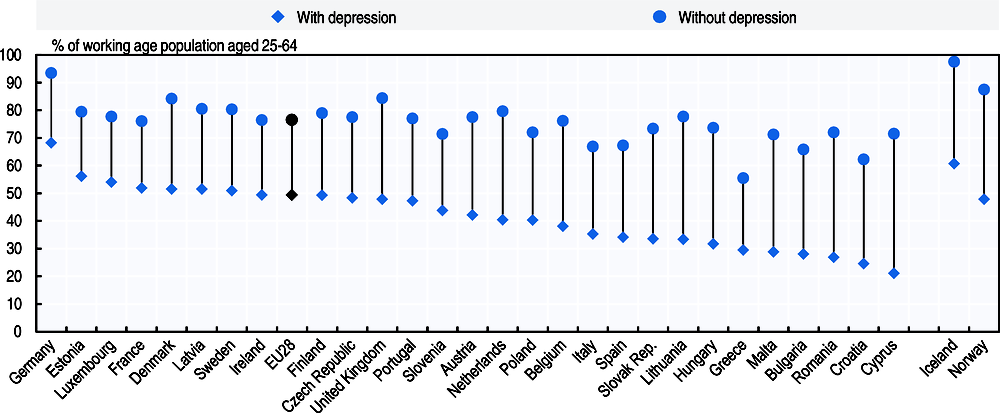
The analysis here only focuses on the labour market impact of depression, as it is the only mental health problem considered in the last wave of the European Health Interview Survey in 2014. Figure 1.7 shows that people reporting chronic depression have much lower employment rates than the rest of the population. Only about half of the population aged 25-64 reporting chronic depression were in employment, compared with over three-quarter (77%) among those who do not report chronic depression on average across EU countries. This employment gap is particularly large in Cyprus, Croatia, Malta, Romania and Bulgaria, although this may partly be due to small sample sizes in EHIS. The cost of this lower employment rate related to chronic depression is estimated at about EUR 176 billion in 2015, representing an amount equivalent to 1.2% of GDP across EU countries as a whole.
Higher absenteeism and lower productivity at work amongst people with mental health problems is estimated to cost about EUR 42 billion in EU countries
Even when people with mental health problems are working, the cost of mental health problems for employees and employers in terms of greater absenteeism and lower productivity at work is high. Reduced working hours and more days of absence from work are estimated to cost about EUR 19 billion or an amount equivalent to 0.13% of GDP across EU countries in 2015.
Even when at work, people with mental health problems do not always function to their full or usual abilities and may be less productive – what is often referred as “presenteeism”. Based on the finding that workers experiencing mental ill-health are about 6% less productive than those without such problems (Hilton et al., 2008), and assuming that lower productivity is reflected in lower wages, the cost of this loss of productivity is estimated at almost EUR 23 billion in 2015.
The high direct and indirect costs of mental illness should not be seen as a foregone conclusion. Greater and more effective investment in mental health promotion and treatment could help substantially reduce many of these costs and help more people realise their full potential.
Actions to promote mental health and prevent mental illness in Europe
The substantial costs of mental health problems make a clear case for increasing efforts to promote good mental health and prevent mental illness, as well as to identify the signs and symptoms of mental illness early, and improve the management and treatment of mental health problems when they occur. More and more European countries are ensuring they have comprehensive policies in place. Several countries (e.g. Belgium, the Czech Republic, Finland, France, Hungary, Ireland, Italy, the Netherlands, Slovenia, Spain, Portugal and the United Kingdom) have a specific plan or policy document addressing mental health promotion and prevention.
Mental health promotion or prevention policies are designed to promote mental health in schools and workplaces, to prevent suicide, to improve the mental well-being of older people, or detect mental distress early on. As awareness of mental illness improves, and stigma around mental illness falls, more people may also seek help when they experience mental illness.
Several international strategies have also supported a greater focus on addressing mental health issues. The 2015 Recommendation of the OECD Council on Integrated Mental Health, Skills and Work Policy (2015) (see Box 1.3) aims to foster mental well-being and improve awareness of mental health conditions by encouraging activities that promote good mental health as well as help-seeking behaviour when mental illness occurs. The European Framework for Action on Mental Health and Wellbeing (European Commission, 2016), too, focused on the effective implementation of policies and interventions contributing to promotion of mental health and the prevention and treatment of mental disorders, including through integration of mental health in all policies and multi-sectoral cooperation. The importance of including mental health promotion is echoed in the activities of the EU-Compass for Action on Mental Health and Wellbeing (see Box 1.4). The WHO Comprehensive Mental Health Action Plan 2013-2020 (WHO, 2013) emphasises integrated and coordinated prevention, promotion, care and support including via the implementation of a multi-sectoral strategy that combines universal and targeted interventions for promoting mental health and preventing mental disorders.
Recognising that mental ill-health demands interventions that are cross-sectoral in scope and complementary in nature, in 2015 the OECD Council published the OECD Recommendation of the Council on Integrated Mental Health, Skills and Work Policy (OECD, 2015). This recommendation is a sign that governments in OECD countries understand that good policies can make a significant difference when it comes to preventing mental illness at all ages, including in youth and adolescence, in supporting those experiencing mental illness to stay in the workplace and supporting those who have left employment to return to the labour market.
The OECD Recommendation gives a series of guidelines to address the impact of mental ill-health on employment, education, health and social outcomes. These guidelines, which all OECD signatories are expected to follow, encourage countries to seek to “promote mental well-being, prevent mental health conditions, and provide appropriate and timely services which recognise the benefits of meaningful work for people living with mental health conditions”.
The EU-Compass for Action on Mental Health and Wellbeing drove the collection, exchange and analysis of information on policy and stakeholder activities in mental health in European countries between 2015 and 2018. The Compass was a means of communicating information on the European Framework for Action on Mental Health and Wellbeing, as well as monitoring the mental health and well-being policies and activities of EU countries and non-governmental stakeholders. Main activities under the Compass included the identification and dissemination of good practices in mental health, collection of information on activities in mental health, and holding mental health workshops in each EU country and in Iceland and Norway.
The EU Compass generated a series of published good practice, annual reports, and consensus paper, especially around seven priority areas:
-
Preventing depression and promoting resilience (priority for 2016)
-
Better access to mental health services (priority for 2016)
-
Mental health at work (priority for 2017)
-
Mental health in schools (priority for 2017)
-
Preventing suicide (priority for 2017)
-
Providing community-based mental health services (priority for 2018)
-
Developing integrated governance approaches (priority for 2018)
Alongside governments, the Compass also engaged with businesses, educational institutions and civil society organisations on their role in implementing positive mental health initiatives. Engaged stakeholders, and policies collected from these stakeholders, are also available on the EU Compass web platform.
There are more than 100 prevention and promotion actions in place across the 28 European countries and 3 EFTA countries (with counting capped at one per life course category in each country). Actions were identified across different points across the life course including: prenatal, perinatal and infancy; children aged 2-10 years and their parents; children and young people aged 11-25 years; workplace mental health; unemployed populations; and older people. Actions were identified from an OECD survey of mental health promotion and prevention programmes, the WHO Mental Health Atlas 2017, and actions reported to the EU Compass 2016-2018, and supplemented with a literature review.
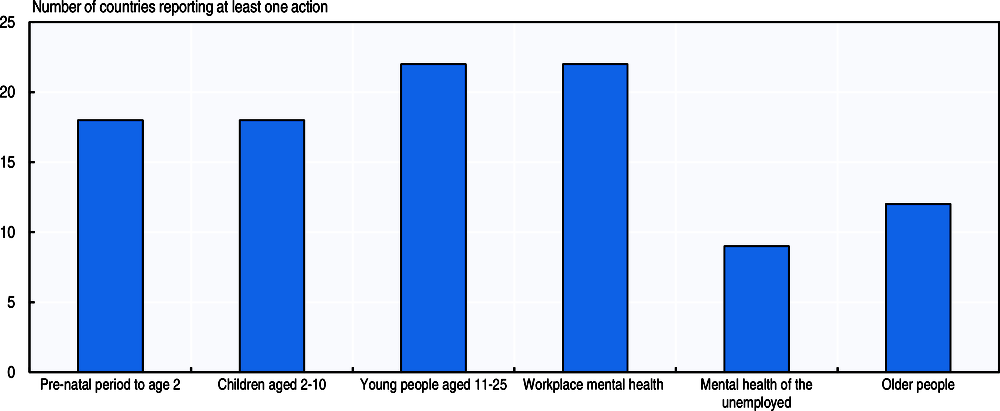
Figure 1.8 identifies countries reporting at least one action in a particular life course area. At least one prevention or promotion action was found in every European country. Targeted prevention or promotion programmes were found in all but four countries (Bulgaria, the Czech Republic, Malta and Romania). Generalised prevention and promotion programmes were also reported, for instance the Czech Republic was unable to divide programmes into target groups as programs supported by the Ministry of Health of the Czech Republic are mostly designed for all persons with mental illness.
It is clear from Figure 1.8 that the distribution of actions to promote mental well-being and prevent mental ill-health is uneven throughout the life course. 22 of 31 countries had actions in place targeting young people aged 11-25 and the actions targeting the workplace, while 18 countries had actions targeting the prenatal to 2 years period, with the same number for children aged 2-10 years. However, actions to target the mental health of unemployed persons were reported or identified in the literature for only 9 countries, and actions targeting the mental health of older populations were reported or found in only 12 countries.
Preventing deaths by suicide
Though suicide remains a major cause of death, and still contributes significantly to mortality from mental illness (as discussed earlier in the chapter), longstanding national commitments to reducing suicide in European countries have helped to reduce the rate of suicide in most countries. On average, the number of deaths by suicide per 100 000 population fell from 12.5 in 2005 to 10.9 in 2015 (Eurostat, 2017). In some countries the falls were even more significant, albeit often from a higher starting rate. Between 2005 and 2015, deaths by suicide fell by more than 20% in almost half of all EU28 countries.
A range of measures are recognised as effective in reducing suicide, including restricting access to lethal means, raising awareness of suicide and suicide risk, improving access to mental health treatment, signposting to sources of help and protective measures in suicide “hotspots”, and tailored efforts to reduce suicide following hospitalisation, for example psychosocial assessment and good follow-up care (Hawton et al., 2016; Zalsman et al., 2016). Such approaches have helped some countries achieve significant falls in suicide rates (for instance Finland, see Box 1.5), even as all countries still continue to seek to prevent suicide more effectively.
In Finland, the rate of suicide has fallen by over 50% over the past 30 years. A significant driver of the reduction in suicide has been the fall amongst young men aged 20-29 (Figure 1.9). Nonetheless, death by suicide amongst young Finnish males remains high in comparison with other Nordic countries (Denmark, Norway, Sweden). Mental illness and alcohol dependence or abuse are significant causal factors (Titelman et al., 2013; Wahlbeck et al., 2011), but socioeconomic conditions have also had an impact.
Suicide prevention campaigns in Finland began in the 1980s, and led to a series of national suicide prevention programmes that ran during the 1990s. Finland’s strategy identified depression, access to mental health care, substance and alcohol abuse, and access to lethal means as central features. The strategy also led to the establishment of crisis phone lines for persons experiencing suicidal thoughts, and guidance to the media, for instance not reporting suicide methods (Patana, 2014; Korkeila, 2013). Recognition that suicide was particularly high amongst young men led to the development of the “Time Out! Back on the track” (Aikalisä! Elämä raitelleen) initiative in 2004, which promoted social inclusion amongst vulnerable men. Two-thirds of participants reported that the participation in the programme was worthwhile, while about 60% considered it had improved their life situation (Appelqvist-Schmidlechner et al., 2012).
At the end of 2017, the Finnish Parliament allocated EUR 300 000 in 2018 to develop a new national strategy to prevent suicide, which will be included in Finland’s new broader National Mental Health Strategy. This work will establish a network for coordinating suicide prevention, and improve the planning, implementation, monitoring and evaluation of suicide prevention measures (Finnish Government, 2017).
Some countries have also developed dedicated national suicide strategies, or included suicide prevention in their broader mental health strategy. A comparative study also found that nationwide suicide prevention programmes had a positive effect in helping to reduce suicide, especially those focused on reducing suicide amongst elderly and young populations (Matsubayashi and Ueda, 2011). For example, Austria began “Suicide Prevention Austria” (Suizidprävention Austria [SUPRA]) in January 2017, focused on national and regional coordination of suicide prevention strategies, developing media support for suicide prevention, research, and integration of suicide prevention into other health promotion activities (EU Compass Consortium, 2017).
Early life interventions to promote mental well-being
Efforts to ensure good mental health in the first few years of life are cost effective in terms of mental, physical, and social outcomes. Effective actions can start even before a child is born: poor maternal mental health – conditions such as anxiety, depression, post-traumatic stress and psychosis affecting some 10-20% of women in the perinatal period (Gavin et al., 2005) – have been associated with poorer physical and cognitive development (Ibanez et al., 2015), higher risk of pre-term birth, and lower birth weight (Jarde et al., 2016).
Many countries have programmes that focus on maternal health, infant health, promoting mental well-being in pre-schools, or parenting support. In England, clinical guidelines by NICE suggest that primary care providers discuss mental health and well-being with women upon first contact during the early postnatal period (National Institute for Health and Care Excellence, 2018). In 2017 the Baby-Mother-Father Perinatal Mental Disorders Service in Hungary developed a new official guideline in intersectoral cooperation, providing support for treatment of perinatal and postnatal depression, which has started as a pilot programme in one hospital (EU Compass for Action on Mental Health and Wellbeing, 2018).
Programmes which promote parenting skills and seek to improve parent-child relationships, often targeting vulnerable or at-risk children, can have a positive impact on the mental health of parents and children. In Germany, the “Early Help” initiative gives support to parents of children aged 0 to 3, delivered by family midwives and other professionals, and is available to all families with more intensive services available for cases requiring more support (McDaid, Hewlett and Park, 2017).
Promotion of good mental health in schools
Schools are an ideal setting for interventions to promote mental well-being as almost all children and young people in Europe spend a good part of their day in school settings. School-based interventions can benefit mental health, develop mental health literacy, as well as improve social and educational outcomes; long-term benefits include improved academic performance, better resilience, and better cognitive skills (Weare and Nind, 2011; Durlak et al., 2011). Investing in good mental health for school-aged children can reduce the risk of children dropping out of school or having a difficult school-to-work transition (OECD, 2015).
School-based programmes often take a universal approach, covering either the full school population or a specific age group (e.g. primary school children or secondary school children). A few countries have introduced programmes that target vulnerable or at-risk children or young people – for instance Finland, Norway or the United Kingdom (McDaid, Hewlett and Park, 2017). Interventions delivered in schools can include actions targeting teaching skills, promotion of positive mental health or well-being, programmes to improve mental health “literacy” and understanding of mental disorders, reduce stigma, or actions to prevent bullying and cyberbullying (see Box 1.6). General mental health promotion programmes are common, for example in Slovenia, the Slovenian Network of Health Promoting Schools which covers 324 schools (around 55%), adopted the theme of mental health promotion in 2015-16, developing a manual for teachers to promote mental health. Zippy’s Friends is a universal school-based programme adopted in 27 countries, including Denmark, Ireland and Lithuania, which helps young children to develop coping and social skills. An evaluation in Norway found that the programme had helped improve the classroom atmosphere, reduce bullying, and improve academic scores (Holen et al., 2013; Clarke, Bunting and Barry, 2014).
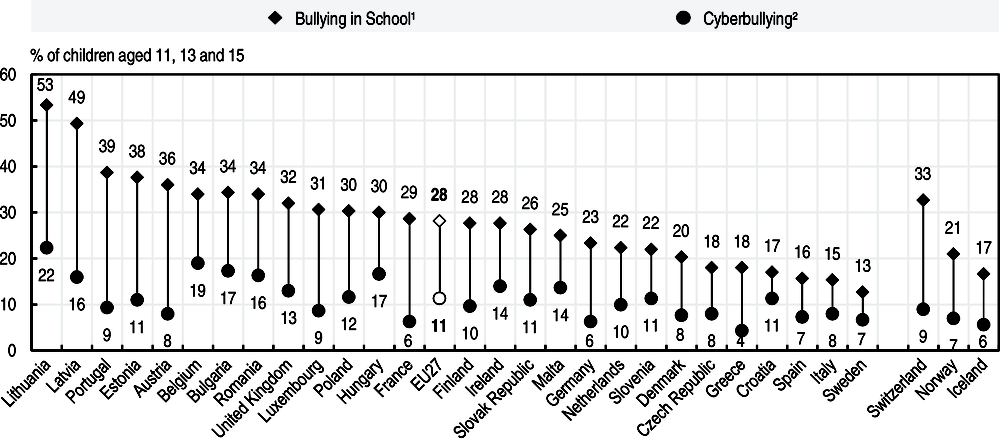
With the increasing ubiquity of the internet, social media and online platforms, the way people, and particularly young people, interact has dramatically changed. While technological developments offer children and young people new opportunities for personal development and growth, they also present challenges to health and well-being. Concern has been rising in particular about cyberbullying. Cyberbullying can include sending offensive messages or comments online, spreading rumours, excluding victims from online groups and other forms of harassment (OECD, 2017). Like bullying, exposure to cyberbullying has been related to a wide range of negative outcomes, including stress and suicidal thoughts (Kowalski et al., 2014), depression and anxiety (Fahy et al., 2016).
The Health Behaviour in School-Aged Children (HBSC) survey of 42 countries asked children about their experiences of bullying on the internet, and found that on average 11% of children aged 11, 13 and 15 reported having been cyberbullied at least once by message. Just over 3% of children reported having been cyberbullied by message at least 2-3 times a month. In all countries the rate of bullying in school was found to be significantly higher than the rate of cyberbullying.
Some interventions have been found as effective ways to counter cyberbullying, including school-based anti-bullying programmes, programmes including parent meetings, parent and child education, and teaching empathy and coping skills (Hutson, Kelly and Militello, 2018; Farrington and Ttofi, 2009) although the long-term effectiveness of these programmes is not clearly evidenced (Cantone et al., 2015).
Protecting and improving the mental health of the working-age population
Actions around mental health in the workplace – which 20 countries report having in place – include efforts to improve mental well-being, actions to support workers experiencing mental ill-health stay in work, and actions to facilitate return-to-work after a period of sickness absence. Such interventions can contribute to reducing some of the high economic costs related to mental illness noted earlier in the chapter and contribute to maximising productivity, opportunities and fulfilment for employees. The most economically effective interventions were found to be those targeting individuals rather than organisations (McDaid and Park, 2014; Hamberg-van Reenen, Proper and van den Berg, 2012).
Many European countries are using health and safety legislation and labour laws to safeguard and promote mental well-being at work. Austria, Belgium, Finland, France, Norway, and the Netherlands are using labour legislation to tackle psychosocial workplace risks. Finland and Lithuania require employers to assess and respond to mental stress and strain at work (McDaid, Hewlett and Park, 2017).
Workplace programmes can focus on the individual, or on an organisation-wide approach, for instance promoting mental health awareness amongst managers, changes to the physical working environment, and improving social relations at work. In Belgium prevention advisers give guidance to workplaces on psychological well-being, and support the preparation of risk assessment plans to minimise stress and violence at work (Samele, Frew Stuart and Urquia Norman, 2013). In the Netherlands the “SP@W: Stress Prevention at Work” aims to identify and deal with stress in the workplace through a learning network, a digital Occupational Stress platform, and roadmaps tailored to each individual company (EU Compass for Action on Mental Health and Wellbeing, 2017).
Few initiatives, though, were found to focus on improving the mental health of the unemployed, with actions reported or identified in the literature for only nine countries. This is despite strong evidence that unemployment is a strong risk factor for mental illness. As noted before, lost income due to lower employment rate of people with depression alone is estimated to amount to EUR 176 billion per year across EU countries, and these estimated costs would be even higher if other mental health disorders were included. Where they exist, many programmes focus on helping to reintegrate individuals who already had mental health problems, rather than supporting the mental well-being of unemployed persons (McDaid, Hewlett and Park, 2017). A few exceptions can be found. In a suburb of Athens, a centre for psychological support of the long-term unemployed was established in 2013, supported by the European Social Fund and Ministry of Health (Center of Psychosocial Support of Long-term Unemployed, 2016).
Given that unemployment is a strong risk factor for mental ill-health, it is important that policies to promote good mental health reach these more vulnerable populations.
Promoting good mental health among older people
As the European population ages – more than 18% of the European population is now over 65, and about 5% is over 80 – promoting healthy ageing is a growing policy priority (OECD, 2017). Mental well-being should be a key part of healthy ageing alongside physical health. There are key mental health risks linked to ageing, for instance around the sometimes-difficult transition from work to retirement, or related to physical illness and frailty. Social isolation, loneliness, and lower levels of contact with friends and family can also contribute to lower levels of mental well-being. Equally, older people commonly fall outside of social structures such as schools and workplaces where mental health promotion and illness prevention interventions are more common, as Figure 1.8 shows.
To promote mental well-being amongst older populations, interventions have focused on tackling some of the risk factors for mental illness, for example loneliness, and promoting activities that foster mental well-being, for instance through promoting social participation. Although evidence on the cost-effectiveness of interventions for the older population is limited, a systematic literature review including more than 10 countries found that participation in social activities, psychosocial educational interventions, intergenerational activities and volunteering, and some educational activities could help protect the mental well-being of older people (McDaid, 2015).
Though far fewer actions to promote the well-being of older people are found than for other parts of the life course, a number of countries are nonetheless intervening with actions primarily to reduce loneliness and isolation. In England, efforts to tackle loneliness amongst older people entailed identifying, signposting, and in some cases funding, of local activities such as lunch clubs, dance afternoons, befriending services, and sports groups (McDaid, Hewlett and Park, 2017). In Norway, government grants are awarded to local areas to create social activities with a social participation component, while in Iceland volunteers from the Icelandic Red Cross make weekly visits to older, ill, or isolated individuals.
Conclusions
Mental health problems represent a huge burden in terms of morbidity and mortality, and can have devastating consequences on the lives of people experiencing mental ill‐health, their friends, relatives and caregivers. More than one in six people across EU countries had a mental health problem in 2016, with an estimated 25 million people suffering from anxiety disorders, 21 million from depressive disorders, 11 million people living with drug and alcohol use disorders, almost 5 million people suffering from bipolar disorder, and schizophrenic disorders affecting an estimated 1.5 million people. For each of these individuals, mental illness will affect their daily lives, their relationships, their jobs, their physical health, their economic status and opportunities.
In some cases, mental ill-health leads not just to lives lived less fully, but also to lives lost prematurely: over 84 000 people died of mental health problems and suicides across EU countries in 2015. While mortality rates – driven primarily by deaths from suicide – vary considerably by gender and by country and have been falling over time in almost all countries, each of these deaths must be seen as a tragedy, and no European country can rest easy. The experience of European countries where deaths from suicide have been reduced so substantially are heartening, and offer policy lessons for other countries to follow.
The burden of mental illness, and the impact of lives lost from suicide and other causes related to mental ill-health, contribute to significant economic costs in Europe. This chapter estimates total costs related to mental ill-health to be equivalent to more than 4% of GDP. While around one-third of these costs are direct spending on health services, most of these costs relate to social security benefits and the indirect costs of mental ill-health in the labour market, driven by lower employment rates and reduced productivity due to mental illness.
Many European countries are taking action to prevent mental illness and to promote mental well-being. More than one hundred interventions to promote good mental health and protect populations from the negative impacts of mental illness were found across the EU, targeting all age groups. Measures are being adopted to promote well-being in schools and nurseries, with new parents, or in workplaces. Reducing stigma and increasing understanding of mental well-being are policy priorities. Furthermore, with improved population-level awareness and understanding of mental health, the stigma around seeking mental health care and talking about mental illness falls. Overcoming stigma and improving diagnosis rates can be expected, in turn, to contribute to more robust data on the true prevalence of mental ill-health.
As this chapter shows, mental ill-health is not distributed evenly across the population, and there are important age, gender and socio-economic differences in the burden of disease. Some groups are also less likely to be the target of promotion or prevention interventions. Supporting vulnerable groups, such as older people or unemployed people, is important to build more inclusive and active societies, but at present far fewer policies reach these groups. The dialectic relationship between distance from social structures and deteriorated mental well-being should also not be underestimated. Just as mental ill-health reduces the likelihood of being in employment, unemployment increases the risk of having poor mental health. Programmes that foster good mental health – reducing loneliness, encouraging social participation, building support structures – and interventions that can identify and respond to signs of mental distress, should be priorities for European countries.
The growing evidence base along with the significant burden of mental illness make clear that there is a societal case for introducing many such promotion and prevention programmes, but there is also a clear economic case for further investment in this area. Actions to prevent mental illness and promote good mental health can bring lifelong benefits to children and their families, workplace interventions can reduce absenteeism and presenteeism, and suicide prevention strategies can prevent tragic losses of life and potential.
The costs of mental illness are extremely high, the potential gains from strengthening mental well-being are significant, and the opportunities for promotion and prevention are far from exhausted. This chapter lays the grounds for a clear case: much more can and must still be done to promote mental well-being and prevent mental ill-health.
References
Appelqvist-Schmidlechner, K. et al. (2012), “Dissemination and implementation of the Time Out! Getting Life Back on Track programme – results of an evaluation study”, International Journal of Mental Health Promotion, Vol. 14/2, pp. 96-108, https://doi.org/10.1080/14623730.2012.703045.
Cantone, E. et al. (2015), “Interventions on bullying and cyberbullying in schools: A systematic review”, Clinical practice and epidemiology in mental health: CP & EMH, Vol. 11/Suppl 1 M4, pp. 58-76, https://doi.org/10.2174/1745017901511010058.
Cavanagh, J. et al. (2003), “Psychological autopsy studies of suicide: A systematic review”, Psychological medicine, Vol. 33/3, pp. 395-405.
Center of Psychosocial Support of Long-term Unemployed (2016), www.menoenergos-pepsaee.gr/index.php/en.
Clarke, A., B. Bunting and M. Barry (2014), “Evaluating the implementation of a school-based emotional well-being programme: A cluster randomized controlled trial of Zippy’s Friends for children in disadvantaged primary schools”, Health Education Research, Vol. 29/5, pp. 786-798, https://doi.org/10.1093/her/cyu047.
Coldefy, M. and C. Gandré (2018), “Personnes suivies pour des troubles psychiques sévères : une espérance de vie fortement réduite et une mortalité prématurée quadruplée”, Questions d’economie de la Santé, Vol. No. 237/September 2018, www.irdes.fr/recherche/questions-d-economie-de-la-sante/237-personnes-suivies-pour-des-troubles-psychiques-severes-une-esperance-de-vie-fortement-reduite.pdf (accessed on 14 September 2018).
Durlak, J. et al. (2011), “The Impact of Enhancing Students’ Social and Emotional Learning: A Meta-Analysis of School-Based Universal Interventions”, Child Development, Vol. 82/1, pp. 405-432, https://doi.org/10.1111/j.1467-8624.2010.01564.x.
EU Compass Consortium (2017), Good Practices in Mental Health and Well-Being, https://ec.europa.eu/health/sites/health/files/mental_health/docs/ev_20161006_co05_en.pdf.
EU Compass for Action on Mental Health and Wellbeing (2018), Annual Activity Reports of Member States and Stakeholders, EU Compass.
EU Compass for Action on Mental Health and Wellbeing (2017), Annual Activity Report of Member States and Stakeholders, EU Compass.
European Commission (2016), EU Framework for Action on Mental Health and Well-being.
Eurostat (2017), Eurostat Database, http://ec.europa.eu/eurostat/data/database.
Fahy, A. et al. (2016), “Longitudinal Associations Between Cyberbullying Involvement and Adolescent Mental Health”, Journal of Adolescent Health, Vol. 59/5, pp. 502-509, https://doi.org/10.1016/j.jadohealth.2016.06.006.
Farrington, D. and M. Ttofi (2009), “School-Based Programs to Reduce Bullying and Victimization”, Campbell Systematic Reviews, Vol. 6, https://doi.org/10.4073/csr.2009.6.
Finnish Government (2017), Ministry of Social Affairs and Health finances the Current Care Guideline for suicide prevention, https://valtioneuvosto.fi/en/article/-/asset_publisher/1271139/stm-rahoittaa-kaypa-hoito-suositusta-itsemurhien-ehkaisyyn.
Gavin, N. et al. (2005), “Perinatal depression”, Obstetrics & Gynecology, Vol. 106/5, Part 1, pp. 1071-1083, https://doi.org/10.1097/01.AOG.0000183597.31630.db.
Grundy, E., T. van den Broek and K. Keenan (2017), “Number of children, partnership status, and later-life depression in eastern and western Europe”, The Journals of Gerontology: Series B, https://doi.org/10.1093/geronb/gbx050.
Gustavsson, A. et al. (2011), “Cost of disorders of the brain in Europe 2010”, European Neuropsychopharmacology, Vol. 21/10, pp. 718-779, https://doi.org/10.1016/j.euroneuro.2011.08.008.
Hamberg-van Reenen, H., K. Proper and M. van den Berg (2012), “Worksite mental health interventions: A systematic review of economic evaluations”, Occupational and environmental medicine, Vol. 69/11, pp. 837-45, https://doi.org/10.1136/oemed-2012-100668.
Hawton, K. et al. (2016), “Psychosocial interventions following self-harm in adults: A systematic review and meta-analysis”, The lancet. Psychiatry, Vol. 3/8, pp. 740-750, https://doi.org/10.1016/S2215-0366(16)30070-0.
Hilton, M. et al. (2008), “Mental ill-health and the differential effect of employee type on absenteeism and presenteeism”, Journal of Occupational and Environmental Medicine, Vol. 50/11, pp. 1228-1243, https://doi.org/10.1097/JOM.0b013e31818c30a8.
Holen, S. et al. (2013), “Implementing a universal stress management program for young school children: Are there classroom climate or academic effects?”, Scandinavian Journal of Educational Research, Vol. 57/4, pp. 420-444, https://doi.org/10.1080/00313831.2012.656320.
Hoven, C., D. Mandell and J. Bertolote (2010), “Prevention of mental ill-health and suicide: Public health perspectives”, European Psychiatry, Vol. 25/5, pp. 252-256, https://doi.org/10.1016/J.EURPSY.2010.01.011.
Hutson, E., S. Kelly and L. Militello (2018), “Systematic review of cyberbullying interventions for youth and parents with implications for evidence-based practice”, Worldviews on Evidence-Based Nursing, Vol. 15/1, pp. 72-79, https://doi.org/10.1111/wvn.12257.
Ibanez, G. et al. (2015), “Effects of antenatal maternal depression and anxiety on children’s early cognitive development: A prospective cohort study”, PLOS ONE, Vol. 10/8, https://doi.org/10.1371/journal.pone.0135849.
IHME (2018), Global Health Data Exchange, www.healthdata.org/.
Jarde, A. et al. (2016), “Neonatal outcomes in women with untreated antenatal depression compared with women without depression”, JAMA Psychiatry, Vol. 73/8, pp. 826, https://doi.org/10.1001/jamapsychiatry.2016.0934.
Kessler, R. et al. (2007), “Age of onset of mental disorders: A review of recent literature”, Current Opinion in Psychiatry, Vol. 20/4, pp. 359-364, https://doi.org/10.1097/YCO.0b013e32816ebc8c.
Kessler, R. et al. (2007), “Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative”, World psychiatry: Official journal of the World Psychiatric Association (WPA), Vol. 6/3, pp. 168-76.
Korkeila, J. (2013), “2781 – Suicide prevention in Finland: Advances and perspectives”, European Psychiatry, Vol. 28, pp. 1, https://doi.org/10.1016/S0924-9338(13)77371-1.
Kovess-Masfety, V. et al. (2016), “Comparing the prevalence of mental health problems in children 6-11 across Europe”, Social Psychiatry and Psychiatric Epidemiology, Vol. 51/8, pp. 1093-1103, https://doi.org/10.1007/s00127-016-1253-0.
Kowalski, R. et al. (2014), “Bullying in the digital age: A critical review and meta-analysis of cyberbullying research among youth”, Psychological Bulletin, Vol. 140/4, pp. 1073-1137, https://doi.org/10.1037/a0035618.
Liu, N. et al. (2017), “Excess mortality in persons with severe mental disorders: A multilevel intervention framework and priorities for clinical practice, policy and research agendas”, World psychiatry: Official journal of the World Psychiatric Association (WPA), Vol. 16/1, pp. 30-40, https://doi.org/10.1002/wps.20384.
Matsubayashi, T. and M. Ueda (2011), “The effect of national suicide prevention programs on suicide rates in 21 OECD nations”, Social Science & Medicine, Vol. 73/9, pp. 1395-1400, https://doi.org/10.1016/j.socscimed.2011.08.022.
McDaid, D. (2015), Independence and Mental Wellbeing for older people.
McDaid, D., E. Hewlett and A. Park (2017), “Understanding effective approaches to promoting mental health and preventing mental illness”, OECD Health Working Papers, No. 97, OECD Publishing, Paris, https://doi.org/10.1787/bc364fb2-en.
McDaid, D. and A. Park (2014), “Investing in Wellbeing in the Workplace”, in Wellbeing, John Wiley & Sons Ltd, https://doi.org/10.1002/9781118539415.wbwell105.
McLoughlin, A., M. Gould and K. Malone (2015), “Global trends in teenage suicide: 2003-2014”, QJM, Vol. 108/10, pp. 765-780, https://doi.org/10.1093/qjmed/hcv026.
Munizza, C. et al. (2013), “Public beliefs and attitudes towards depression in Italy: A national survey”, PLoS ONE, Vol. 8/5, pp. e63806, https://doi.org/10.1371/journal.pone.0063806.
National Institute for Health and Care Excellence (2018), Antenatal and postnatal mental health: Clinical management and service guidance/Guidance and guidelines/NICE.
Nock, M. et al. (2009), “Cross-National Analysis of the Associations among Mental Disorders and Suicidal Behavior: Findings from the WHO World Mental Health Surveys”, PLoS Medicine, Vol. 6/8, https://doi.org/10.1371/journal.pmed.1000123.
Observatoire national du suicide (2018), Suicide : enjeux éthiques de la prévention, singularités du suicide à l’adolescence – 3e rapport/février 2018.
OECD (2018), Education indicators in focus #60: How is depression related to education?, OECD.
OECD (2017), PISA 2015 Results (Volume III): Students’ Well-Being, PISA, OECD Publishing, Paris, https://doi.org/10.1787/9789264273856-en.
OECD (2015), Fit Mind, Fit Job: From Evidence to Practice in Mental Health and Work, Mental Health and Work, OECD Publishing, Paris, https://doi.org/10.1787/9789264228283-en.
OECD (2015), Recommendation of the Council on Integrated Mental Health, Skills and Work Policy, OECD/LEGAL/0420, https://legalinstruments.oecd.org/en/instruments/334.
OECD (2014), Making Mental Health Count: The Social and Economic Costs of Neglecting Mental Health Care, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/9789264208445-en.
OECD (2012), Sick on the Job?: Myths and Realities about Mental Health and Work, Mental Health and Work, OECD Publishing, Paris, https://doi.org/10.1787/9789264124523-en.
Patana, P. (2014), “Mental Health Analysis Profiles (MhAPs): Finland”, OECD Health Working Papers, No. 72, OECD Publishing, Paris, https://doi.org/10.1787/5jz1591p91vg-en.
Samele, C., Frew Stuart and Urquia Norman (2013), European profile of prevention and promotion of mental health (EuroPoPP-MH).
Titelman, D. et al. (2013), “Suicide mortality trends in the Nordic countries 1980-2009”, Nordic Journal of Psychiatry, Vol. 67/6, pp. 414-423, https://doi.org/10.3109/08039488.2012.752036.
Wahlbeck, K. et al. (2011), “Outcomes of Nordic mental health systems: Life expectancy of patients with mental disorders”, British Journal of Psychiatry, Vol. 199/06, pp. 453-458, https://doi.org/10.1192/bjp.bp.110.085100.
Weare, K. and M. Nind (2011), “Mental health promotion and problem prevention in schools: What does the evidence say?”, Health Promotion International, Vol. 26/suppl 1, pp. i29-i69, https://doi.org/10.1093/heapro/dar075.
WHO (2018), Mental Health Atlas 2017, World Health Organization, Geneva.
WHO (2014), Preventing suicide suicide A global imperative, World Health Organization.
WHO (2013), Mental Health Action Plan 2013-2020, World Health Organization.
WHO (2001), “Mental health: Strengthening mental health promotion”, 220, World Health Organization.
Wittchen, H. et al. (2011), “The size and burden of mental disorders and other disorders of the brain in Europe 2010”, https://doi.org/10.1016/j.euroneuro.2011.07.018.
Zalsman, G. et al. (2016), “Suicide prevention strategies revisited: 10-year systematic review”, The Lancet Psychiatry, Vol. 3/7, pp. 646-659, https://doi.org/10.1016/S2215-0366(16)30030-X.
Note
← 1. These IHME estimates are lower than those previously reported by Wittchen et al. (Wittchen et al., 2011), partly because they do not include the prevalence of dementia.