Preterm birth and low birth weight
Preterm birth (i.e. birth before 37 completed weeks of gestation) is the leading cause of neonatal death during the first four weeks of life (days 0-28), and the second leading cause of death in children under 5 (see indicator “Under age 5 mortality” in Chapter 3). Many survivors of preterm births also face a lifetime of disability, including learning disabilities and visual and hearing problems as well as long-term development. But preterm birth can be largely prevented. Three-quarters of deaths associated with preterm birth can be saved even without intensive care facilities. Current cost-effective interventions include kangaroo mother care (continuous skin to skin contact initiated within the first minute of birth), early initiation and exclusive breastfeeding (initiated within the first hour of birth) and basic care for infections and breathing difficulties (WHO, 2013; see indicator “Infant mortality” in Chapter 3). Preterm birth rates can be also reduced if women, particularly adolescents, have better access to family planning and increased empowerment, as well as improved care and nutrition during pregnancies (see indicator “Family planning” in Chapter 4).
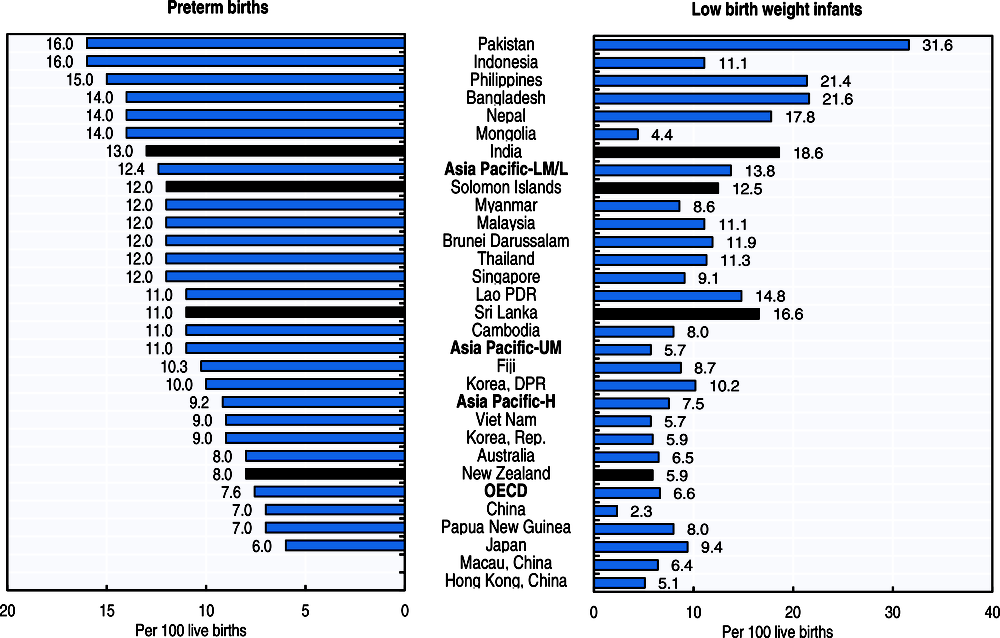
An estimated 15 million babies were born preterm worldwide and over 1 million babies died from preterm birth complications in 2015 (WHO, 2018a). In the Asia-Pacific region, India, China, Pakistan, Indonesia, Bangladesh and the Philippines have a particularly large number of preterm births and they accounted for almost half of the preterm births globally. Across Asia-Pacific countries and territories, 11 babies out of 100 were born preterm on average in 2014 but the rate varies across countries, ranging from 6 in Japan to 16 in Pakistan and Indonesia (Figure 4.3, right panel). Sri Lanka and China have halved the rate in a recent decade through a national focus on improved obstetric and neonatal care, and the systematic establishment of referral systems with higher capacity of neonatal care units and staff and equipment (March of Dimes, Save the children, WHO, 2012).
Overall, it is estimated that 15% to 20% of all births worldwide are low birth weight, representing around 20 million births a year. In 2012, the World Health Assembly endorsed the Comprehensive implementation plan on maternal, infant and young child nutrition, which specified a set of six global nutrition targets. One of those targets aims to a 30% reduction in low birth weight by 2025.
Low birth weight occurring from restricted foetal growth or preterm birth is also an important determinant of child health as it is associated with greater risk of poor health, death or disabilities (UNICEF and WHO, 2004). Low birthweight is the result of many factors but largely preventable. Mothers’ risk factors include poor nutritional status or a low body-mass index (BMI), low socioeconomic status or minority race, being a young mother, smoking or exposure to second hand smoke, excessive alcohol consumption, and history of in-vitro fertilisation treatment and low weight births.
On average, 11 newborns out of 100 had low weight at birth across Asia-Pacific countries and territories (Figure 4.3, left panel). There is a significant regional divide between countries in eastern Asia (such as China, the Republic of Korea and Mongolia) and southern Asia (Bangladesh, India, Nepal, Pakistan and Sri Lanka). China has the lowest low birth weight rate at 2.3% while Pakistan reported a rate of 31.6%. China achieved reductions in low birthweight through rapid and sustained economic growth over recent decades and also through improved access to food in many provinces.
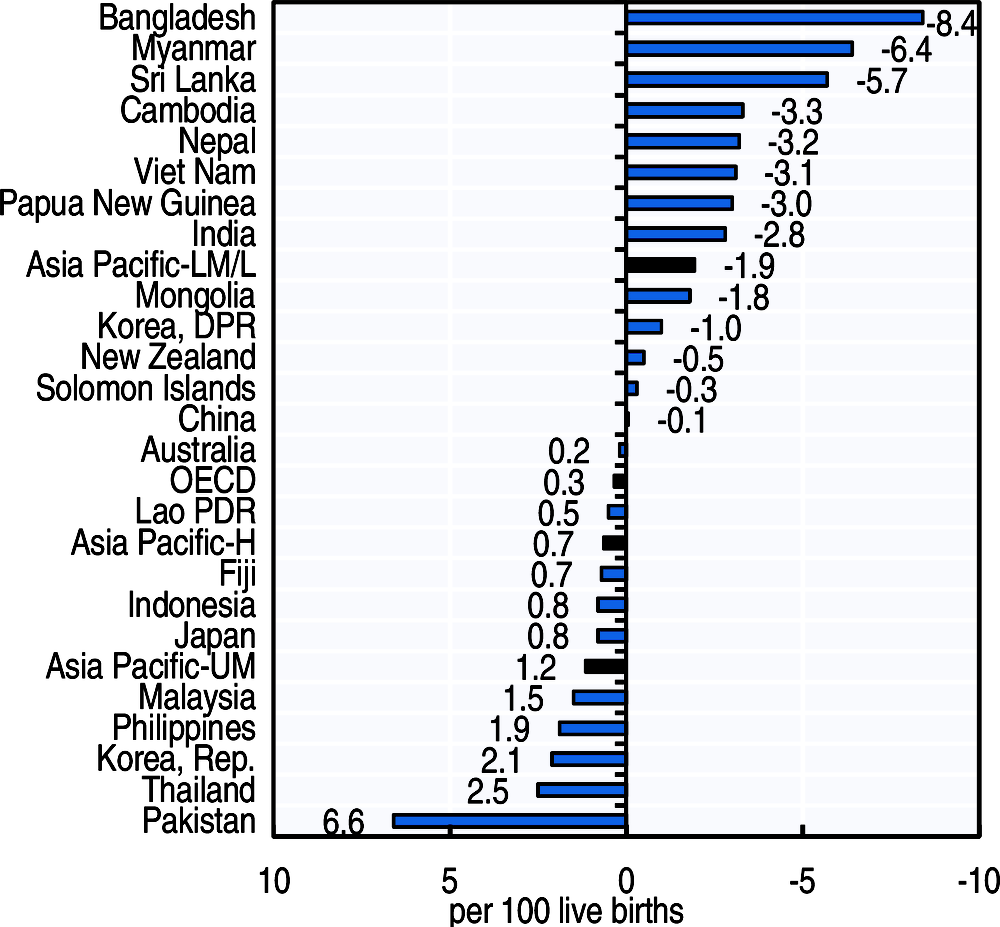
Two infants less are low weight at birth in 100 live births in lower-middle and low income Asia-Pacific countries in 2014 as compared to 2000, while two infants more are low weight at birth in 100 live birth in the Republic of Korea, Thailand and six infants more in Pakistan in 2014 compared to 2000 (Figure 4.4). A substantial decline in the rate of low birth infants was observed in Bangladesh, Myanmar and Sri Lanka.
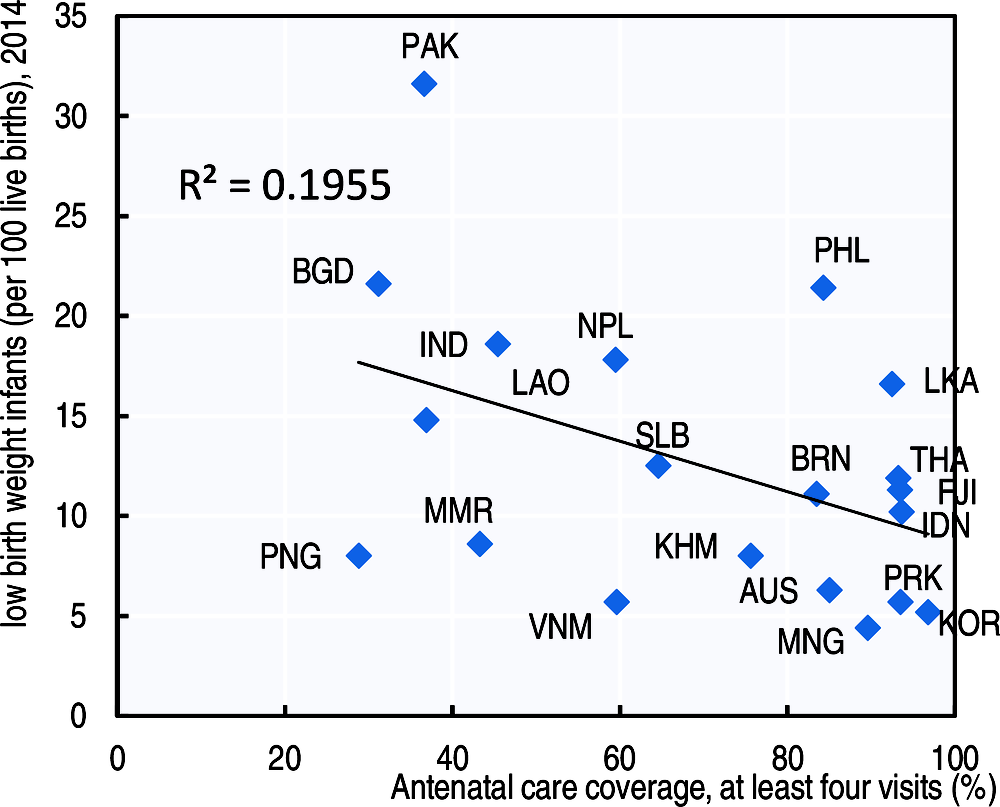
Antenatal care can help women prepare for delivery and understand warning signs during pregnancy and childbirth. Higher coverage of antenatal care is associated with higher birth weight, suggesting the significance of antenatal care over infant health status across countries (Figure 4.5).
Preterm birth is defined as babies born alive before 37 weeks of pregnancy are completed. There are sub-categories of preterm birth based on gestational age: extremely preterm (less than 28 weeks); very preterm (28-32 weeks); moderate to late preterm (32-37 weeks).
Low birthweight is defined by the World Health Organization as the weight of an infant at birth of less than 2 500 grams (5.5 pounds) irrespective of the gestational age of the infant. This figure is based on epidemiological observations regarding the increased risk of death to the infant and serves for international comparative health statistics.
In developed countries, the main information sources are national birth registers. For developing countries, low birthweight estimates are primarily derived from mothers participating in national household surveys, as well as routine reporting systems (UNICEF and WHO, 2004).