Avoidable hospital admissions
Most health systems have developed a ‘primary level’ of care whose functions include health promotion and disease prevention, managing new health complaints, managing long-term conditions and referring patients to hospital-based services when appropriate. A key aim is to keep people well, by providing a consistent point of care over the longer-term, tailoring and co-ordinating care for those with multiple health care needs and supporting the patient in self-education and self-management.
Asthma, chronic obstructive pulmonary disease (COPD) and congestive heart failure (CHF) are three widely prevalent long-term conditions. Both asthma and COPD limit the ability to breathe: asthma symptoms are usually intermittent and reversible with treatment, whilst COPD is a progressive disease that almost exclusively affects current or prior smokers. Asthma may affect up to 334 million people worldwide (Global Asthma Network, 2014). About 3 million people died of COPD in 2015, which is equal to 5% of all deaths globally that year (WHO, 2016). CHF is a serious medical condition in which the heart is unable to pump enough blood to meet the body’s needs. CHF is often caused by hypertension, diabetes or coronary heart disease. Heart failure is estimated to affect over 26 million people worldwide resulting in more than 1 million hospitalisations annually in both the United States and Europe (Ponikowski et al., 2014).
Common to all three conditions is the fact that the evidence base for effective treatment is well established and much of it can be delivered at a primary care level. A high-performing primary care system, where accessible and high quality services are provided, can reduce acute deterioration in people living with asthma, COPD or CHF and reduce unnecessary admissions to hospital.
Figure 6.8 shows hospital admission rates for asthma and COPD together, given the physiological relationship between the two conditions. Admission rates for asthma vary 15-fold across countries with Italy, Mexico and Colombia reporting the lowest rates and Latvia, Turkey, and Korea reporting rates over twice the OECD average. International variation in admissions for COPD is 25-fold across OECD countries, with Japan and Italy reporting the lowest rates and Hungary and Ireland the highest rates. Combined, there is a lower 7-fold variation across countries for the two respiratory conditions.
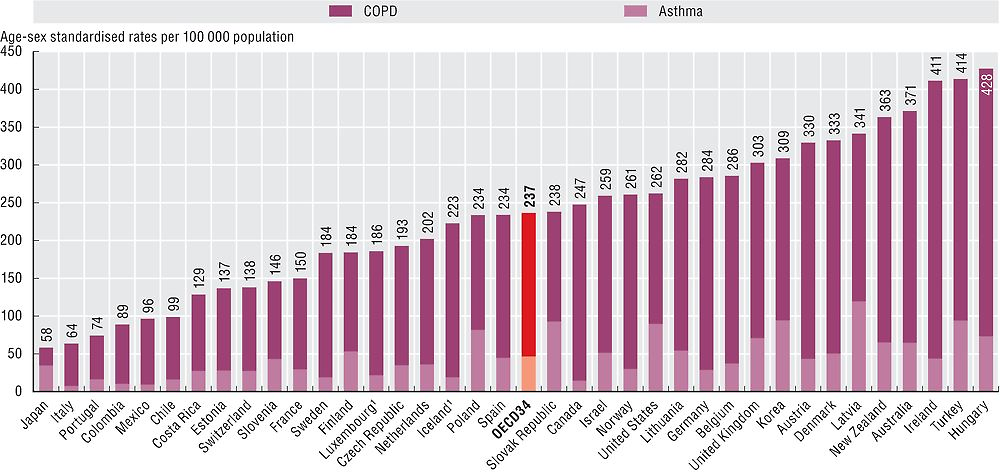
1. Three-year average.
Source: OECD Health Statistics 2017.
Hospital admission rates for CHF vary 12-fold, as shown in Figure 6.9 Colombia, Costa Rica and Mexico, have the lowest rates, while Hungary, Poland and Lithuania report rates about 2 times the OECD average.
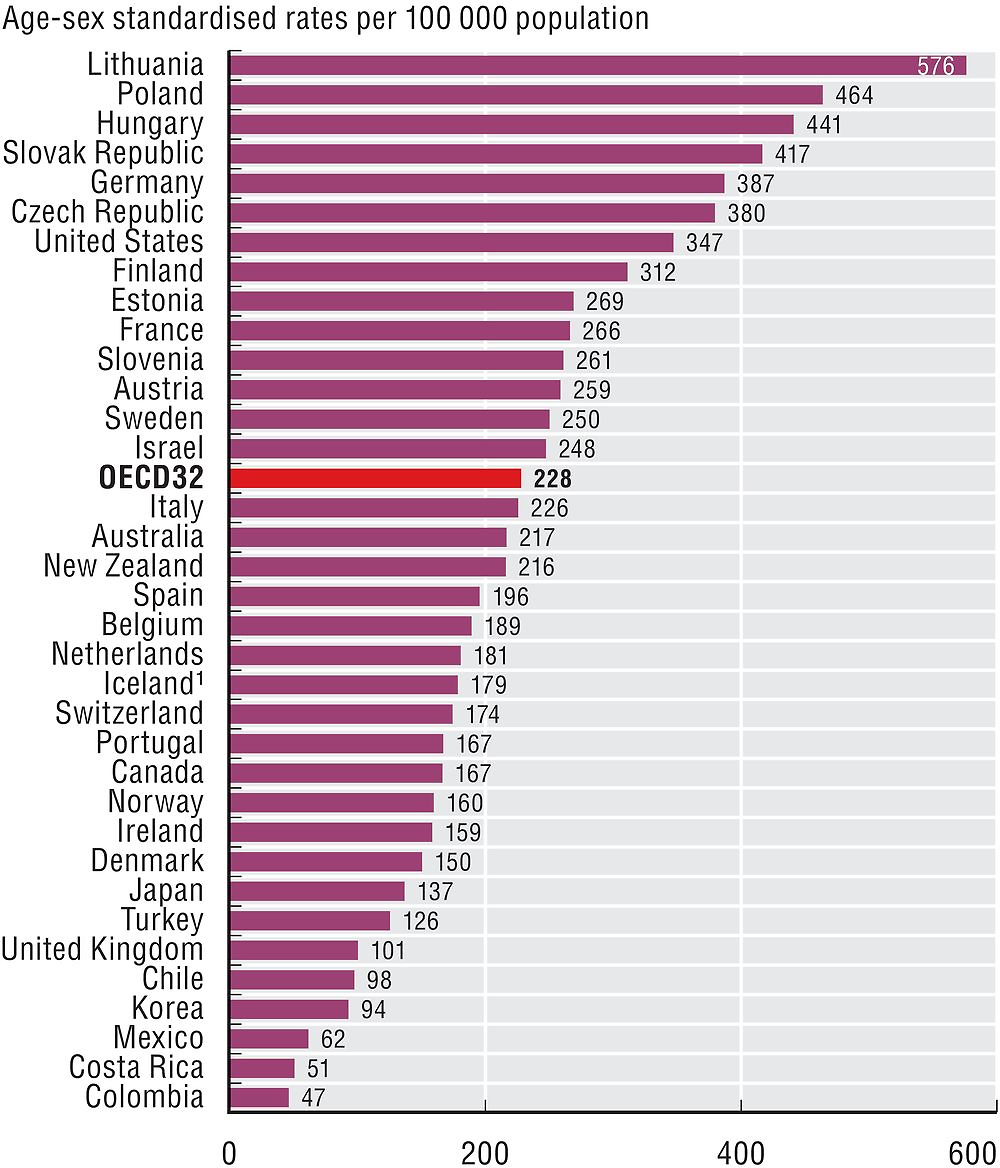
1. Three-year average.
Source: OECD Health Statistics 2017.
Figure 6.10 reveals that in Austria, Israel and Ireland a reduction in admission rates for CHF has been achieved in recent years, whereas in Belgium rates have remained relatively stable and in Spain rates have increased. While observed improvements may represent advances in the quality of primary care for these countries, recent reviews undertaken by OECD indicate that investment in primary care may not be happening fast enough (OECD, 2017b), potentially resulting in wasteful spending on health care (OECD, 2017a)
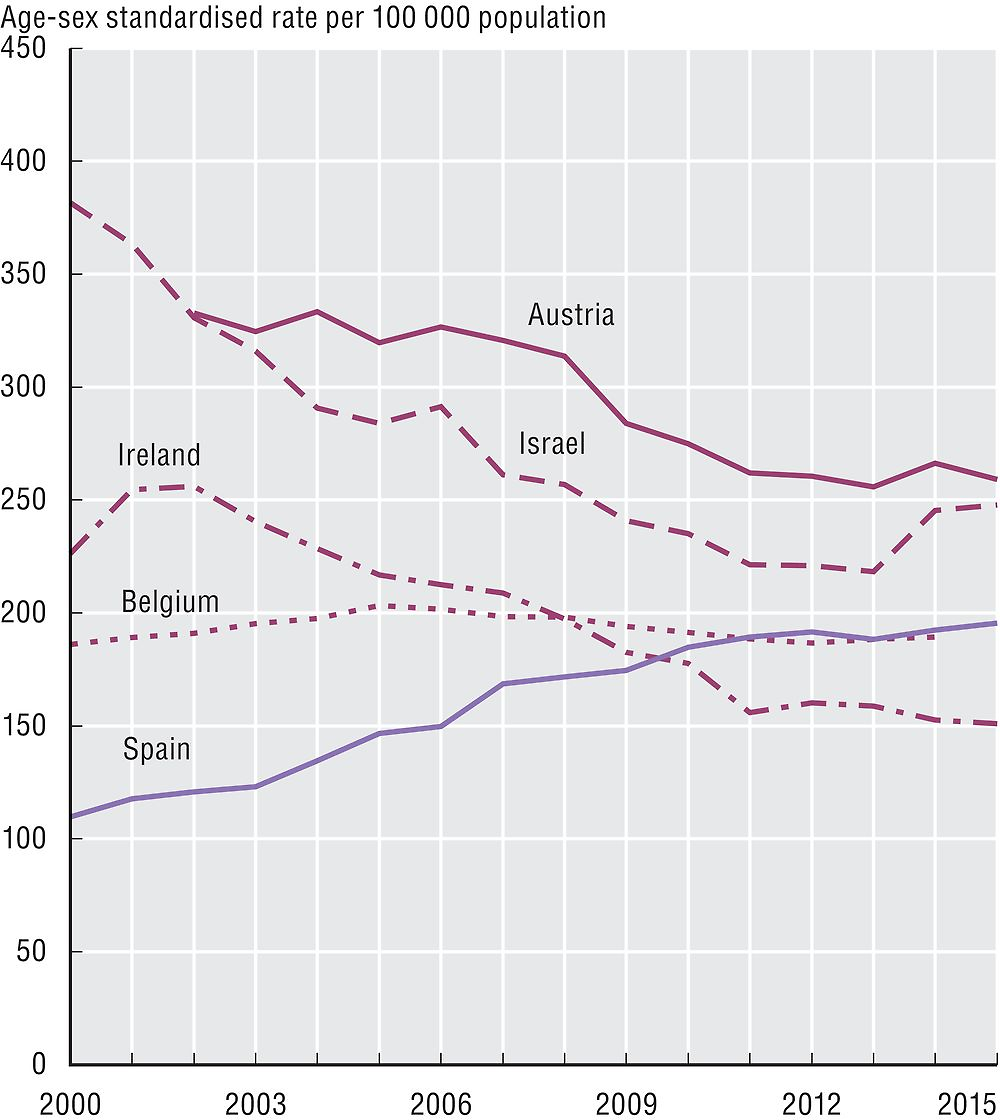
Source: OECD Health Statistics 2017.
The indicators are defined as the number of hospital admissions with a primary diagnosis of asthma, COPD or CHF among people aged 15 years and over per 100 000 population. Rates are age-sex standardised to the 2010 OECD population aged 15 and over. Admissions resulting from a transfer from another hospital and where the patient dies during the admission are excluded from the calculation as these admissions are considered unlikely to be avoidable.
Disease prevalence and availability of hospital care may explain some, not all, variations in cross-country rates. Differences in coding practices among countries may also affect the comparability of data. For example, the exclusion of “transfers” cannot be fully complied with by some countries. Differences in data coverage of the national hospital sector across countries may also influence indicator rates.
References
Global Asthma Network (2014), The Global Asthma Report 2014, Auckland, New Zealand, access at http://www.globalasthmareport.org/resources/Global_Asthma_Report_2014.pdf.
OECD (2017a), Tackling Wasteful Spending on Health, OECD Publishing, Paris, https://doi.org/10.1787/9789264266414-en.
OECD (2017b), Caring for Quality in Health, Lessons Learnt from 15 Reviews of Health Care Quality Publishing, Paris, http://www.oecd.org/els/health-systems/Caring-for-Quality-in-Health-Final-report.pdf.
Ponikowski, P. et al (2014), “Heart Failure: Preventing Disease and Death Worldwide”, ESC Heart Failure, No. 1, pp. 4–25, https://doi.org/10.1002/ehf2.12005.
WHO (2016), “Chronic Obstructive Pulmonary Disease (COPD)”, November 2016 http://www.who.int/mediacentre/factsheets/fs315/en/.
