Unmet needs for health care due to cost
Access to health care may be prevented for a number of reasons. These can be due to the functioning of the health care system (such as the cost of health care, distance to the closest health care facility, or waiting lists) or to personal reasons (including fear of not being understood by the doctor or not having the time to seek care). People who forgo health care when they need it may jeopardise their health status.
Unmet needs due to cost is a particularly pressing problem, especially among lower-income groups. Consequently, an increasing number of countries collect data to measure the extent to which health care is foregone due to cost (Fujisawa and Klazinga, 2017). This includes whether people skipped consultations or prescribed medicines due to cost.
On average across OECD countries, just over one in ten people reported having skipped a consultation due to cost in 2016, based on 17 OECD countries (Figure 5.4). Relatively high numbers of people reporting to forego consultations is somewhat surprising, as in most OECD countries consultations are free of charge or with a small co-payment (Paris et al., 2016). The share of the population foregoing consultations due to cost is high in Poland (33%), and also in the United States (22.3%) and Switzerland (20.9%). Less than 5% of the population in Germany, Spain, Sweden, the United Kingdom, Israel and Italy reported skipping consultations due to cost.
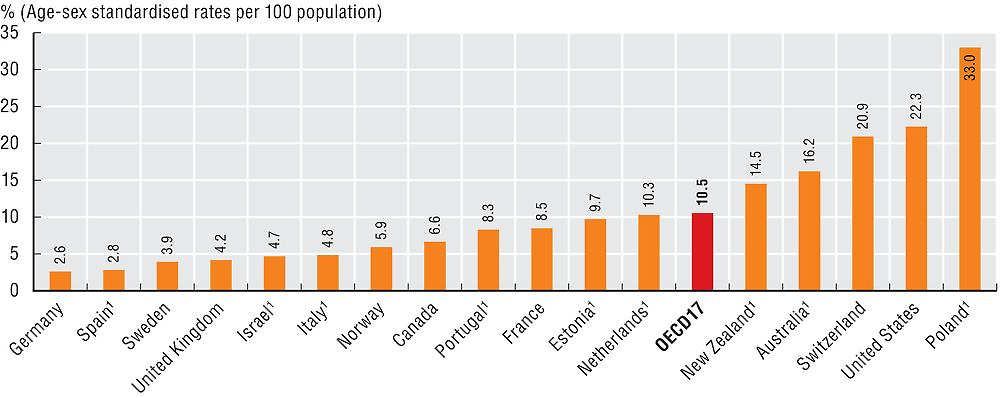
1. National sources.
Source: Commonwealth Fund International Health Policy Survey 2016 and other national sources.
In most countries, the share of the population who skipped a consultation due to cost has not changed much in recent years, but there are some exceptions. A large increase was observed in Switzerland, with people who have foregone consultations concentrated among those younger than 50 years of age and those with low income (OFSP, 2016). In Germany and Estonia, the share of the population who skipped consultation due to cost has decreased.
In terms of prescribed medicines, on average 7.1% of people reported having skipped prescribed medicines due to cost, based on 15 OECD countries (Figure 5.5). Most OECD countries have co-payments for prescribed medicines, though often with exemptions for specific population groups (Paris et al., 2016). Population shares reporting foregone prescribed medicines were highest in the United States (18%) and Switzerland (11.6%); and lowest in Germany (3.2%) and the United Kingdom (2.3%). In most countries, the share of the population who skipped prescribed medicine due to cost has slightly decreased in recent years. Large improvements were reported in Israel, Estonia and Australia. In Israel, this may be due in part to policies to improve accessibility and affordability of medicines for chronic patients and the elderly.
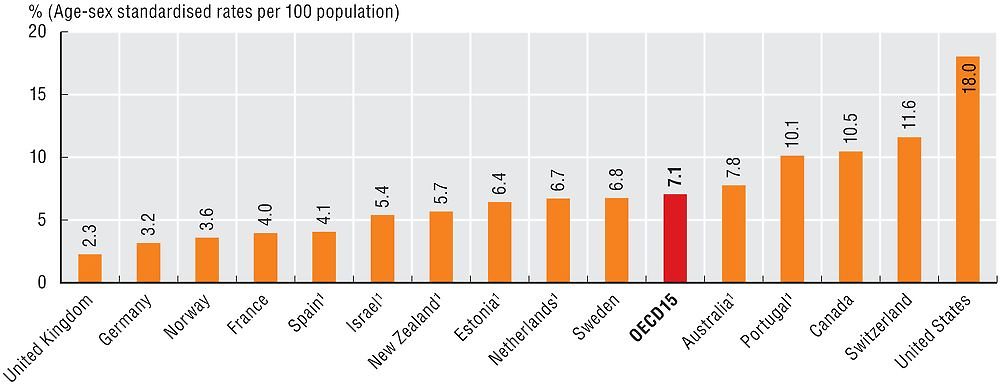
1. National sources.
Source: Commonwealth Fund International Health Policy Survey 2016 and other national sources.
Unmet needs for health care due to cost are consistently higher among people in low income groups compared with those in high income groups, across OECD countries (Figure 5.6). An exception is in the United Kingdom, where unmet care needs due to cost are similar for low income adults and the rest of the population. Unmet needs are particularly large among the low income in the United States, where 43% of low income adults reported having unmet care needs due to cost in 2016. There were also large gaps in unmet care needs between high and low income people in France and Canada.
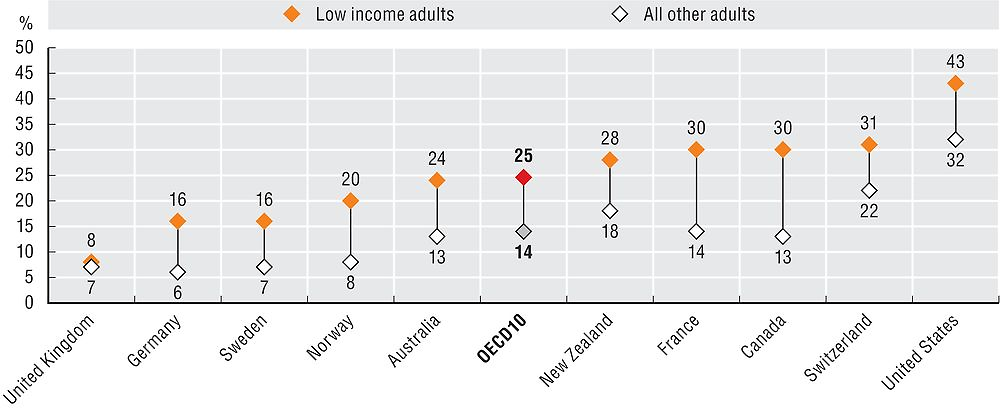
Note: Either did not consult with/visit a doctor because of the cost, skipped a medical test, treatment, or follow-up that was recommended by a doctor because of the cost, did not fill/collect a prescription for medicine, or skipped doses of medicine because of the cost. “Low income” is defined as household income less than 50% of the country median. Sample sizes are small (n < 100) in the Netherlands and the United Kingdom.
Source: Commonwealth Fund International Health Policy Survey 2016.
Self-reported unmet care needs should be assessed together with other indicators of potential barriers to access, such as the extent of health insurance coverage and the amount of out-of-pocket payments. Strategies to improve access to care for disadvantaged or underserved populations need to tackle both financial and non-financial barriers, as well as promoting an adequate supply and distribution of the health workforce.
The OECD collects data on unmet care needs due to cost reported by populations from national and international sources and a number of countries reporting these measures are increasing over time. These use questions that are similar to those asked in the Commonwealth Fund International Health Policy Survey. Rates for Figures 5.4 and 5.5 refer to both primary and secondary care and they are age-sex standardised to the 2010 OECD population structure, to remove the effect of different population structures across countries. Due to the change of data source for this indicator, data cannot be compared directly with those presented in the previous editions of Health at a Glance.
The 2016 Commonwealth Fund’s International Health Policy Survey asks whether people did not visit a doctor when they had a medical problem, skipped a medical test, treatment, or follow-up that was recommended by a doctor, or did not fill prescription for medicines or skipped doses because of cost in the past year and as it also collects socio-economic background including income level, it allows analysis on unmet care needs by income group. This survey was carried out in 11 countries.
References
Fujisawa, R. and N. Klazinga (2017), “Measuring Patient Experiences (PREMs): Progress Made by the OECD and its Member Countries 2006-2015”, OECD Health Working Papers, Paris.
OFSP (2016), “Prise en charge médicale: la population suisse est satisfaite”, Communiqué de presse, Berne, https://www.bag.admin.ch/bag/fr/home/aktuell/medienmitteilungen.msg-id-64545.html.
Paris, V. et al. (2016), “Health Care Coverage in OECD Countries in 2012”, OECD Health Working Papers, No. 88, OECD Publishing, Paris, https://doi.org/10.1787/5jlz3kbf7pzv-en.
