Tuberculosis
Tuberculosis (TB) is the leading cause of death from an infectious disease in Asia-Pacific. In 2018, there were 10 million incident (new and relapsed) TB cases worldwide, 1.2 million deaths among HIV-negative people globally. More than 40% of new cases and almost half of deaths were estimated in India, Indonesia and Pakistan alone. Most of these TB cases and deaths occur disproportionately among men, but the burden of disease among women is also high as it remains among the top three killers for them in the world. Most cases of TB are curable if diagnosed early and the right treatment is provided – such as first-line antibiotics for 6 months -, therefore curtailing onward transmission of infection (WHO, 2019[26]).
TB was declared a global health emergency by WHO in 1993 and the WHO-coordinated Stop TB Partnership set targets of halving TB prevalence and deaths by 2015, compared with a baseline of 1990. The WHO’s End TB Strategy (post-2015) which followed the Stop TB Strategy aims at ending the global TB epidemic by 2035, in line with the Sustainable Development Goals. In the Delhi Call for Action to End TB in the WHO South-East Asia Region by 2030, the health ministers pledged to implement national tuberculosis programmes through an “empowered national initiative” (Sharma, 2017[27]).
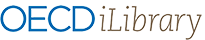
In Asia-Pacific, TB mortality rates were high in Korea DPR and Papua New Guinea with over 50 deaths of people without HIV per 100 000 populations (Figure 3.25, left panel).
Five countries in the world which collectively accounted to 56% of the estimated TB cases globally in 2018 were in the Asia-Pacific region: India (2.69 million), China (0.86 million), Indonesia (0.84 million), the Philippines (0.59 million) and Pakistan (0.56 million). The case notification rate is particularly high in Korea DPR, Papua New Guinea and the Philippines, at more than 300 cases per 100 000 population. An incidence rate higher than 500 cases per 100 000 population was estimated for the Philippines and Korea DPR, while for Australia, New Zealand and Japan less than 15 incident cases per 100 000 population were estimated (Figure 3.25, right panel).
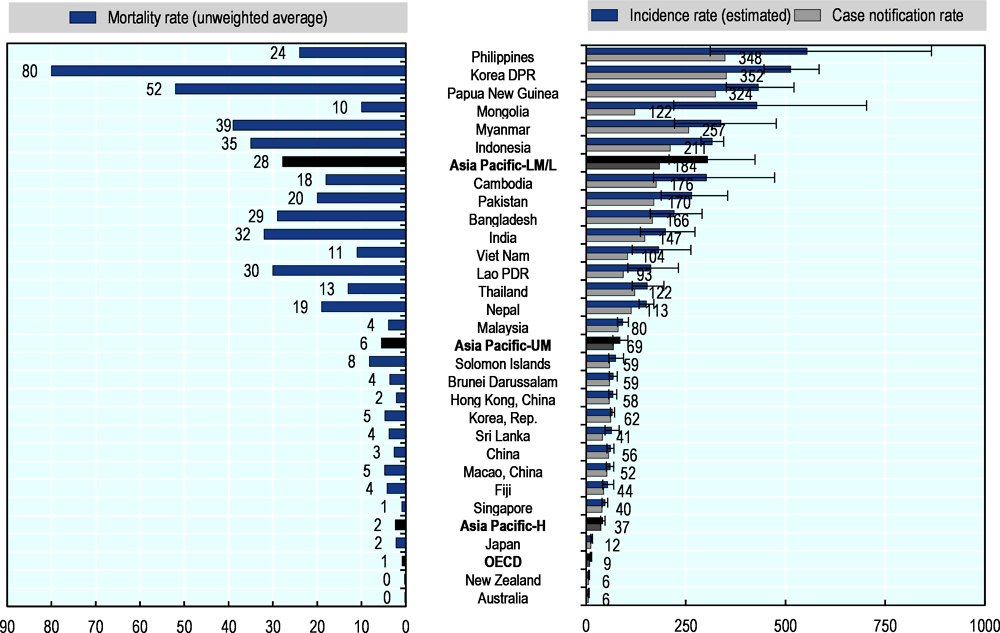
High-quality TB services have expanded and many cases are treated, reaching the treatment success rate for new TB cases of more than 80% in most Asia-Pacific countries in 2017 (Figure 3.26). Nevertheless, Hong Kong, China, Japan and Papua New Guinea report a low treatment success rate at 70%.
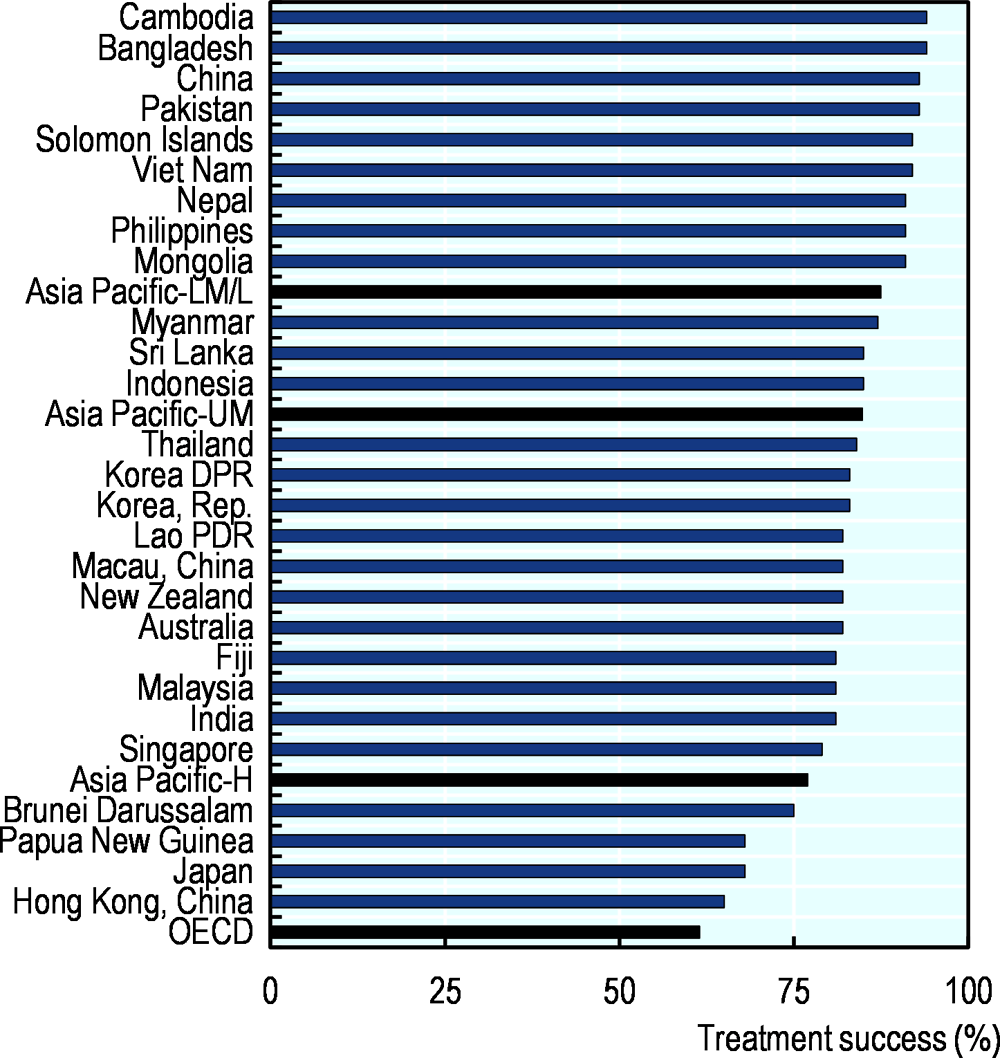
The Asia-Pacific region is rising to the challenges presented by TB. In a large part of the countries, incidence rates have declined from 2013 to 2018 (Figure 3.27). However, countries like Malaysia, the Philippines, Fiji, Singapore, New Zealand, Australia and Brunei Darussalam are showing upward trends, with the latter four belonging to the high-income economies group and experiencing low base incidence rates. In the period in this study, TB incidence was stable in Bangladesh, Mongolia and Papua New Guinea.
The region still faces important challenges in TB control, including providing services to those in greatest need, especially the poor and vulnerable. HIV-TB co-infection, the emergence of drug-resistant strains, a sizeable proportion of TB-affected population facing catastrophic costs due to TB, funding gaps and the need for greater technical expertise all remain threats to progress (WHO, 2016[28]; WHO, 2019[26]). Concerning drug-resistant TB (MDR/RR-TB), the burden is high in China with 7.1% of new cases are estimated to have MDR/RR-TB. This proportion is also high at 5.1% in Myanmar and Viet Nam, at above 4%. Treatment of MDR/RR-TB can take up to two years and is far more costly than drug susceptible strains.
Tuberculosis (TB) is a contagious disease, caused by the Mycobacterium tuberculosis bacteria. Tuberculosis usually attacks the lungs but can also affect other parts of the body. It is spread through the air, when people who have the disease cough, sneeze, talk or spit. Most infections in humans are latent and without symptoms, with about one in ten latent infections eventually progressing to active disease. If left untreated, active TB kills between 20% and 70% of its victims within ten years depending on severity.
The TB incidence rate is the number of new and relapse cases (newly occurring) of the disease estimated to occur in a year, per 100 000 population. TB mortality does not include TB/HIV as per ICD-10. Case notification rate is the total of new and relapse cases and cases with unknown previous TB treatment history notified to the national programmes per 100 000 population.