6. The digital transformation of primary health care in Brazil
Brazil has made strides towards a digital transformation of PHC, building on more than a decade of policies to digitalise health care and make better use of health data, and with key investments in networks, data, interoperability and skills. The COVID-19 pandemic has only provided further impetus. Yet, progress towards effective use of digital PHC has been slow, and fundamentally unequal, with significant inequalities in the use of digital technologies and tools among health workers and citizens. Other major barriers include human and technical capacities in municipalities, with potential diseconomies of scale resulting from setting responsibilities for digital health at municipal level. Tackling these challenges requires: 1) digitalising all PHC units and teams; 2) promoting inclusive connectivity for all Brazilian citizens, especially the most vulnerable; and 3) establishing a governance structure with clear well-funded mandates at the right levels of government.
A digital transformation of health care in Brazil is well underway, propelled by a broader strategy for a digital transformation of the public sector. For some time now, the Government of Brazil has been increasing its use of digital tools and data to make its public institutions more efficient, more transparent and more responsive to citizen and business demands (OECD, 2018[1]). Clear governance and a focus on connectivity, interoperability, open government data and citizen-driven service delivery have resulted in Brazil recently scoring above the OECD average on the 2019 Digital Government Index (OECD, 2020[2]).
Brazil has made significant inroads with respect to building a foundation for digital PHC, from strategies at various levels of government to essential investments in networks, data, interoperability and skills. However, progress towards effective use of digital technologies in PHC has been slow, and fundamentally unequal. Contributing factors include both demand and supply side factors, but also disarticulated governance and insufficient and poorly targeted funding.
This chapter provides an overview of recent initiatives and developments in the digitalisation of PHC in Brazil. Over the last decades, Brazil has been making impressive progress towards a digital transformation of its public sector and its health care services, but progress towards effective use of digital technologies in PHC has been slow, and fundamentally unequal, as discussed in section 6.2. Moreover, as shown in section 6.3, millions of Brazilians are digitally excluded, and there is a risk that a digital transformation of PHC will only compound existing social divides. The chapter concludes with a discussion in section 6.4 of how Brazil’s decentralised government, along with the country’s heterogeneous regional demographics, socio-economic indicators and governance structures, create challenges to digitalising PHC.
The creation of the Brazilian Internet Steering Committee (CGI.br) in 1995 to provide strategic guidelines related to the use and development of the Internet in Brazil can only be considered foundational (OECD, 2018[1]). The Committee established the basis for an ecosystem between citizens, the private sector and the public sector. Linked to the Brazilian Internet Steering Committee, and sitting under the Brazilian Network Information Centre (NIC.br), the Regional Centre for Studies on the Development of the Information Society (Cetic.br) was created in 2005 to monitor the adoption of information and communication (ICT) technologies in Brazil. It has conducted its ICT Households Survey annually since 2005, and has, since 2013, also undertaken the ICT in Health Survey focusing on the infrastructure, availability and use of ICT-based applications in health care facilities in Brazil. These surveys are invaluable and they provide many of the statistics and indicators used in this chapter. Unfortunately, the most recent results predate COVID-19 and thus may not fully reflect the current situation.
6.2.1. The government has made strides with a clear ambition for digital health services
Since 1995, and especially in recent years, Brazil has made impressive progress towards a digital transformation of its public sector. In 2019, more than 500 public services, spanning 29 different entities, were made available through digital channels, leading to reported annual savings of USD 66.9 million1 (BRL 345 million) (gov.br, 2020[3]). Under its current Digital Government Strategy 2020-22, the government is aiming to offer all of its more than 3 000 public services via digital channels by the end of 2022 (Diário Oficial da União, 2020[4]). Among the existing digital transformation plans of 73 public entities is the Brazilian National Digital Health Strategy 2020-28 (Estratégia de Saúde para o Brasil para 2028 or ESD28).
The ESD28 (2020[5]) builds on more than a decade of policies to digitalise health care and make better use of health data, going as far back as the National Policy for Health Information and Informatics of 2004 (Política Nacional de Informação e Informática em Saúde or PNIIS). There has been an acceleration of efforts in more recent years, with the publication of the 2015 PNIIS, which is currently being reviewed, the publication in 2017 of the e-Health Strategy for Brasil 2020 (Estratégia e-Saúde para o Brasil 2020), and the publication in 2020 of Brazil’s National Digital Health Strategy Action, Monitoring and Evaluation Plan (Plano de Ação, Monitoramento e Avaliação da Estratégia de Saúde Digital para o Brasil 2019-23). The ESD28 is also aligned with Brazil’s National Health Plan 2020-23 (Ministério da Saúde, 2020[6]).
Actions within the ESD28 are built around three axes (Ministério da Saúde, 2020[5]). The first axis seeks to build on existing programmes and initiatives to digitalise health care in Brazil, including the National Health Data Network (Rede Nacional de Dados em Saúde or RNDS), as well as the Connect SUS (Conecte SUS) and the Informatiza APS programmes (these are described in greater detail below). The second axis looks to develop the necessary conditions (e.g. organisational, legal, regulatory and governance structures) to spur effective collaboration in digital health. The third and final axis will establish a conceptual, normative, educational and technological forum (the so-called Espaço de Colaboração) to operationalise collaboration. Training and capacity building for health care workers is a key priority in the implementation of the ESD28.
The ESD28 plan of action has seven priorities (Ministério da Saúde, 2020[5]): 1) governance and leadership, 2) digitalisation of the three levels (primary, secondary and tertiary) of health care provision, 3) supporting health care quality improvements, 4) the patient as the protagonist, 5) human resource training, 6) an environment of interconnectivity, and 7) an innovation ecosystem. The ESD28 also identifies the main actors and stakeholders, establishing five types of participation (leadership, partnership, sponsorship, contribution, engagement) that are expected of each actor for each action point (see Box 6.1).
Action point 2.1.2 of the ESD28 seeks to expand the digitalisation of PHC in Brazil. It is led by the Ministry of Health and the Health Secretaries of Municipalities and States, in partnership with the CONASSEMS and CONASS, with sponsorship from the Federal Government, the National Health Council and the CIT, plus contributions from Associations of Health Professionals, and engagement from Anvisa and ANS. The foundation of this action point is the Primary Health Unit Computerisation Programme (Programa de Apoio à Informatização e Qualificação dos Dados da Atenção Primária à Saúde) or Informatiza APS, which seeks to digitalise all PHC units and teams in Brazil. New financing schemes (part of Programa Previne Brasil) and implementation and training initiatives have been piloted in the state of Alagoas (more detail is provided in the text below). The timeline for full implementation of the action point is December 2022.
Source: Ministério da Saúde (2020[5]), Estratégia de Saúde Digital para o Brasil 2020-28, http://bvsms.saude.gov.br/bvs/publicacoes/estrategia_saude_digital_Brasil.pdf.
There is a comprehensive push for a digital PHC in Brazil
The importance of connecting and digitalizing PHC practices is clear and the potential value added would be very significant (see Box 6.2). Digital health can help PHC be the first point of contact with patients, co-ordinate referrals and follow-up to secondary and tertiary care, and monitor and keep track of community and population-level health risks and conditions (Castle-Clarke and Imison, 2016[7]). The COVID-19 pandemic has made clear there are enormous benefits to digitalising and connecting health care facilities and services.
Digital PHC is the use of digital technologies to support PHC (it is a subfield of digital health focusing specifically on PHC). Digital technologies (or information and communication technologies) are electronic tools, systems, devices and resources that generate, store, process and/or transmit data. Digital technologies include devices such as smartphones and computers, as well as intangible products such as software, platforms and algorithms, and can support PHC in a variety of ways.
At the centre of digital PHC is the electronic health record or EHR. The EHR is a longitudinal digital record of an individual patient that contains or virtually links together multiple electronic medical records from different institutions and health care settings. As it contains a history of contact with health care providers from any organisation at any level of care, the EHR plays an essential role in helping PHC providers co-ordinate care for individual patients.
An EHR that is complete, accurate, up-to-date, comprehensive, and that can be shared, enables a plethora of digital applications in PHC. An EHR that contains clinical (e.g. medications prescribed), sociodemographic (e.g. employment) and administrative (e.g. insurance) information allows supports many applications, including among many others:
Targeted alerts and reminders to patients (e.g. for screenings or vaccinations).
Electronic referrals, ePrescribing and certifications (e.g. for sick leave).
Clinical decision making (e.g. medications to avoid given patient allergies).
Telemedicine applications (e.g. video consultations and remote monitoring).
Mobile health or mHealth applications (e.g. smoking cessation and mental health apps).
Population-level statistics on the prevalence and incidence of diseases and risks.
Research studies taking into account real-world data (e.g. pharmacovigilance).
It is possible to implement some of these applications without a complete EHR system (e.g. telemedicine), however without the EHR, digital technologies will fall short of their potential and will not fully assist PHC.
Source: World Health Organization (2018[8]), Digital technologies: shaping the future of primary health care, https://apps.who.int/iris/bitstream/handle/10665/326573/WHO-HIS-SDS-2018.55-eng.pdf?sequence=1&isAllowed=y; OECD (2019[9]), Health in the 21st Century: Putting Data to Work for Stronger Health Systems, https://dx.doi.org/10.1787/e3b23f8e-en.
The potential benefits of a digital transformation of PHC are also clear in the context of Brazil’s National Health Plan 2020-23 (Ministério da Saúde, 2020[6]). Among its objectives are to promote the expansion and effectiveness of PHC services in an integrated and planned fashion, to guarantee access to quality PHC services for all, and to reduce population health risks through prevention, epidemiological surveillance and health promotion.
Brazil has a long history of developing, implementing and using health information systems (Ministério da Saúde, 2017[10]). In 2017, the government launched a public tender, the Primary Health Unit Computerisation Programme, to support the country’s PHC units in using electronic health record (EHR) systems by enhancing connectivity, acquiring ICT equipment, and providing technical support and training of health professionals (OECD, 2020[11]). Following concerns from the Federal Court of Accounts regarding the viability of a national rollout, the programme was replaced by Connect SUS. Connect SUS seeks to bring together all the health information of any one citizen under a large data network that can be used to continuously improve health care and decision making. The Connect SUS programme depends on two essential elements: the RNDS and the updated Primary Health Unit Computerisation Programme (Programa de Apoio à Informatização e Qualificação dos Dados da Atenção Primária à Saúde or Informatiza APS).
Through the Connect SUS programme, and as part of the Previne Brasil programme, the Informatiza APS programme provides federal funding (between USD 330 or BRL 1 700 and USD 388 or BRL 2000 per month) to family health teams that are able to collect and send data from electronic health record (EHR) systems (Harzheim et al., 2020[12]). The programme includes the provision of training in ICT and data analysis to public employees in municipal health departments (CGI.br, 2020[13]). The training is jointly organised by the Ministry of Health and the University of Rio Grande do Sul. It consists of 60 hours of training delivered through Telehealth Centres. In order to qualify for support from Informatiza APS, family health teams need to have already made investments in digital technologies, have a working EHR system and be able to share data through the PHC Health Information System (the Sistema de Informação em Saúde para a Atenção Básica or SISAB). Those teams that are eligible may use the funds from Informatiza APS to acquire software or hardware, pay for Internet connectivity in UBS, and hire ICT services, among others.
A key eligibility requirement of the Informatiza APS programme is that family health units need to already be using digital technologies. However, Connect SUS ran a pilot project in the state of Alagoas between October 2019 and June 2020 that did include an additional financial incentive for PHC units that have not yet been able to digitalise (Ministério da Saúde, 2020[14]). The Alagoas pilot provided a lump sum of between USD 1 649 (BRL 8 500) and USD 1 940 (BRL 10 000) to each municipality in Alagoas for every PHC unit that was not yet digitalised (more than USD 1.07 million or BRL 5.5 million were disbursed to 97 municipalities). In light of the COVID-19 pandemic, the Ministry of Health instituted a time-limited incentive of USD 5 268 (BRL 27 157) to be paid to municipalities and states for each health team that has not yet been digitalised (see Box 6.3). The Ministry of Health is also collaborating with the Ministry of Science, Technology, Innovation and Communications, with support from the National Education and Research Network (Rede Nacional de Ensino e Pesquisa or RNP), to provide Internet connectivity to 16 000 PHC facilities (CGI.br, 2020[13]).
A key element of Connect SUS focusing specifically in PHC is the e-SUS APS strategy (or Estratégia e-SUS APS, often also referred to as e-SUS AB for Atenção Básica) which seeks to modernise PHC through the use of health information systems, in order to better manage individual health and care, optimise data collection and improve health information (Ministério da Saúde, 2020[6]). The strategy is based on two underlying data collection systems: the simplified data collection system (Coleta de Dados Simplificada) and the EHR system (Prontuário Eletrônico do Cidadão or PEC). Around 56% of family health units that have been digitalised use the PEC, while others use third-party EHR systems (Ministério da Saúde, 2020[14]).
The Informatics Department of SUS – typically referred to as DATASUS – has also made various other applications available to citizens, frontline care workers and health care managers (CGI.br, 2020[13]). These include: MedSUS, an application that lists all medications approved for use in SUS; e-Gestor AB, a platform that combines multiple PHC information systems to facilitate the planning and delivery of health services; and the Conecte SUS Cidadão app, which builds on a previous version called Meu digiSUS¸ which allows citizens to access their personal and clinical data collected from multiple national registries as well as access useful information, such as where are the closest health care facilities and pharmacies. There are also versions of Conecte SUS for frontline health workers (Conecte SUS Profissional) as well as managers.
Another interesting system is DigiSUS Gestor – Módulo Planejamento (DGMP), a tool made available to states, the Federal District and municipalities in May of 2019. The DGMP allows local managers to register population health targets, annual plans, produce and send reports to the National Health Council, as well as produce annual reports. The Ministry of Health also makes available an Application Programming Interface, or API, that allows different software platforms used by health care facilities to integrate their EHR systems with the RNDS, as well as make use of blockchain solutions.
Municipalities are also increasingly providing digital services to citizens (CGI.br, 2020[13]). For example, the São Paulo prefecture has developed an app called Agenda Fácil which allows patients to book, confirm and cancel consultations and examinations in the municipality’s PHC units. According to the latest ICT Electronic Government Survey (2020[15]), 25% of Brazilian prefectures allow patients to book appointments online and in some cases to be consulted via the Internet.
Start-ups in telemedicine are also becoming increasingly relevant. Brasil Telemedicina, founded in 2010, offers online medical services. It produces around 60 000 reports per month and has clients in more than 700 Brazilian cities (Brasil Telemedicina, 2020[16]). Another startup, Telelaudo, provides tele radiology services 24 hours a day, seven days a week, and employs 120 radiologists. It has provided more than 4.7 million reports to more than 450 hospitals (Telelaudo, 2021[17]).
The federal government authorised on 15 April 2020 the use of telemedicine during the COVID-19 pandemic (through law number 13.989/2020). This enabled continuity of care for patients who may have feared physically visiting health care facilities, but it also protected health care professionals most at risk of serious COVID-19 (such as those with chronic conditions, those who are pregnant and those aged 60 years old and older) (see Chapters 3 and 4). To help PHC units access digital technologies, the Ministry of Health also instituted an exceptional incentive to be paid to municipalities and states for each health team that has not yet been digitalised, budgeting over USD 83.8 million (BRL 432 million) for 2020. The Brazilian Telemedicine University Network (RUTE) also created a special interest group on COVID-19.
Artificial intelligence, specifically machine learning algorithms, has also been employed to monitor the spread of SARS-CoV-2 infections and to actively search for individuals who may have been exposed to the virus. Algorithms have been used to predict how the virus will spread further, to assess the clinical outlook of individual patients as well as support decisions concerning the most appropriate treatments, and to manage hospital beds and other resources.
Chatbots and virtual assistants have been used by public authorities to provide accurate information on COVID-19 to populations, and also to collect data that can be used to monitor the spread of the virus. The Ministry of Health created a WhatsApp channel to answer questions from citizens as well as health care professionals, and to fight disinformation. Various states – such as Ceará, Rio Grande de Sul, and Amazonas – have also used digital tools to communicate with their populations and to aid decision making during the pandemic.
This rapid adoption of digital tools is potentially introducing some risks. For example, the emergency approval of telehealth during COVID-19 (law 13.989/2020) does not include any language relating to medical liability, data and information protection and security, medical licensing across states, nor location of medical act for tax purposes. While in some cases, it is clear that other existing laws apply (e.g. with respect to data protection and medical liability), the lack of specific text on these issues may introduce significant uncertainty and lead to lower adoption than would be desirable.
Source: CGI.br (2020[13]), ICT in Health 2019; CGI.br (2020[15]), ICT Electronic Government 2019; Diário Oficial da União (2020[4]) PORTARIA Nº 3.193, DE 27 DE NOVEMBRO DE 2020; Caetano et al. (2020[18]), Challenges and opportunities for telehealth during the COVID-19 pandemic:, https://doi.org/10.1590/0102-311X00088920.
6.2.2. Progress towards digital health has been uneven, especially in PHC
Out of the 40 880 PHC units (from a total of 43 200) that responded to the ICT in Health Survey (2020[13]), it is estimated that 3 600 did not have computers and 7 200 were not connected to the Internet. Internet connection speeds in PHC facilities increased from 2018 to 2019, but still only 17% of PHC units had speeds over 10 Mbps (CGI.br, 2020[13]). Across all health care facilities, only 20% of public facilities had speeds over 10 Mbps compared to 60% of private facilities. The United States Federal Communications Commission (FCC) recommends a minimum speed of 10 Mbps for a small practice with two to four physicians (ONC, 2019[19]). Speeds under 4 Mbps are not recommended if practices want to make simultaneous use of EHR systems and high-quality video consultations, not to mention remote patient monitoring. Because many public PHC facilities are small, these facilities do not actually contract broadband connections themselves, but rather these are procured by municipal and state health secretaries. This could be why almost half (46%) of managers in public health facilities do not know the speed of their broadband connections (CGI.br, 2020[13]).
While health care managers increasingly perceive their ICT equipment and Internet connections to be up-to-date and appropriate, there are marked differences between perceptions of managers in public and private health facilities (CGI.br, 2020[13]). A majority (68%) of managers of private facilities consider their ICT equipment to be new and up-to-date, compared to only 36% of managers in public facilities, and 40% of managers in PHC units. Similarly, 67% of managers in private facilities considered their Internet connection to be appropriate given their needs, compared to only 31% of managers in public health care facilities, and 32% in PHC units. These same patterns are observed among frontline care workers, like physicians and nurses. Across both public and private facilities, managers in non-capital cities were less likely than managers in capitals to consider their ICT equipment and Internet connections were up-to-date and appropriate.
Only 14% of public health care facilities (from large institutions with over 50 beds to smaller PHC practices) had an ICT department, compared to 38% of private facilities (CGI.br, 2020[13]). Among PHC units, 10% had in-house ICT teams. The share of public facilities (16%) that had an information security policy was significantly lower than the share of private facilities with such a policy (44%). Among PHC units, 15% had an information security policy in place. Around 14% of public facilities had adopted data loss protection and prevention tools, compared to 29% of private facilities. The use of information security tools in PHC units was especially underdeveloped, with only 40% of facilities having a firewall, only 27% with encrypted databases, and 16% having data loss prevention tools. Close to a third of PHC units did not have password-protected access to electronic systems.
In 2019, an estimated 82% of all health care facilities and 78% of PHC units had EHR systems (CGI.br, 2020[13]). Around 18 000 health care facilities (or 18% of all facilities) did not have an EHR system, 12 000 of which were public facilities. According to the National Register of Health Establishments (CNES), 62% of FHTs were digitalised (using the same definition as that used in Informatiza APS), leaving almost 20 000 teams not digitalised (Ministério da Saúde, 2020[14]).
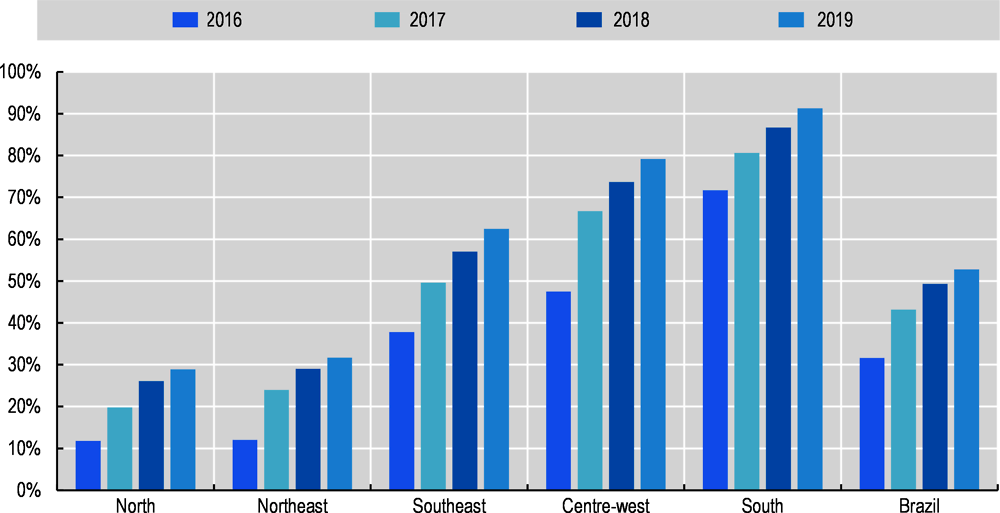
Adoption of EHR systems was highest in the South and Southeast regions (at 90% and 83% of facilities in those regions, respectively) compared to the Northeast and North regions (77% and 74% respectively). Facilities in non-capital cities lagged behind those in capital cities in the use of EHR systems (79% of non-capital facilities compared to 92% of facilities in state capitals). Close to one in every three public facilities, and 25% of all PHC units, still maintained clinical records and patient data only in paper form, compared to one in ten private facilities. In particular, while a majority of physicians in public facilities do use electronic prescribing, 71% of physicians signed their prescriptions by hand, rather than electronically. Between 2016 and 2019, the number of PHC units using EHR systems increased from 13 375 to 21 557, a 61% increase in three years (Ministério da Saúde, 2020[6]). Yet, the evolution has been very unequal across regions of Brazil (see Figure 6.1).
Many of Brazil’s indigenous populations are based in the North and Northeast regions where digitalisation is least advanced. Indigenous children under one year old have lower rates of utilisation of medical appointments to monitor their growth and development (Ministério da Saúde, 2020[6]). There are also significant inequalities in the rates of vaccination against yellow fever in Brazilian states where vaccination has been recommended, ranging, in 2018, from 21.8% in Sergipe to 100% in the Federal District and Roraima (the national average for all states where vaccination is recommended is 64.1%).
Digital tools can help tackle these inequalities but the underlying infrastructure needs to be in place. Unfortunately, the rate of digitalisation of PHC units in Brazilian states seems to be inversely proportional to inequalities in health status and need. The share of hospital admissions due to conditions that are treatable in PHC is higher in regions with lower use of EHR systems in PHC units: the North and Northeast regions. Digital PHC could help reduce unnecessary admissions through, for example, better prevention, screening and monitoring of conditions that are treatable in PHC (see Box 6.2), but this cannot happen if the needed enablers – from infrastructure to software to skills – are not in place.
While the majority of health care facilities did have an EHR system in place, the information and data contained within these systems was not always complete, limiting the potential benefits. Decision support capabilities, specifically, were low, with only around a fifth of health facilities (including both large inpatient facilities with more than 50 beds as well as smaller PHC units) having EHR systems that allow, for example, drug allergy and drug dosage alerts (CGI.br, 2020[13]). Only around a third of facilities were capable of sending and receiving discharge reports or clinical information (ibid).
Since 2018, the ICT in Health Survey collects data on how many health care facilities have electronic systems in place to send or receive data directly from electronic systems in other health care facilities (be it PHC practices or hospitals). In both 2018 and 2019, the share of health care facilities that had systems in place to exchange information was 19%, suggesting that interoperability and data exchange remain limited in Brazil (CGI.br, 2020[13]). This is a serious barrier to effective PHC, greatly limiting care continuity and co-ordination.
Around one in five public health care facilities and PHC units offer digital services directly to patients (CGI.br, 2020[13]). These include scheduling appointments (23% of PHC units), exams (20% of units) as well as accessing results online (22% of units). Around one in ten allow patients to access their health record online and 7% of PHC units enable communications with health professionals.
Telehealth has been in use in Brazil for quite some time now, especially in remote areas like the Amazon (Santos et al., 2016[20]). In the rest of the country, however, its use has been very uneven. Around one-fifth of health care facilities provide remote learning (or e-learning) services (CGI.br, 2020[13]): continued education for health care professionals delivered via videoconferencing. The share of PHC units using remote learning is higher, reaching 39%. This is the most frequent use of telehealth, with other applications, such as real-time teleconsultations and remote monitoring, having lower adoption rates. Having said that, PHC units make more use of telehealth that the average health care facility in Brazil, with 35% providing teleconsultations and 25% telediagnosis. For example, remote monitoring has been implemented in less than one in ten facilities.
Unlike with the use of EHR and the Internet, it is public health care facilities that are most active in telehealth networks, with virtually no participation among private providers (CGI.br, 2020[13]). Among public facilities, 32% report being part of state telehealth networks, 19% report being part of the Brazil Telehealth Network Programme (Programa Nacional Telessaúde Brasil Redes), and 11% report participating in the Telemedicine University Network (RUTE). Among PHC units, the shares were 40%, 23% and 14% for state networks, the Brazil Telehealth Network Programme and RUTE respectively. Despite these encouraging figures, 47% of all public health care facilities are not part of any telehealth network.
The Brazil Telehealth Network Programme seeks to expand and improve health care provision, especially through PHC. The programme provides health care professionals that are part of the network both synchronous (real-time) and asynchronous teleconsultations, telediagnostics, second opinions and telelearning (Ministério da Saúde, 2020[6]). In 2015, the SMART (Sistema de Monitoramento e Avaliação de Resultados do Programa Telessaúde) system was created to monitor the use of telehealth services in Brazil. From 2016 to July 2019, just under 3.5 million telehealth services (from teleconsultations to telelearning sessions) had been registered by SMART. Of these, 50% had taken place in the Southeast region and 36% in the South region. Only 1% of activities took place in the North region. Out of 26 Brazilian states, only 18 have telehealth centres participating in the network.
Few health care professionals participated in ICT training courses in 2019, according to the latest ICT in Health Survey (2020[13]). Around 36% of nurses and 30% of physicians reported having completed capacity-building courses in health informatics, 8% of nurses and 6% of physicians participated in specialisation courses, and only 1% of nurses and 2% of physicians signed up for master’s or doctorate degrees in health informatics.
Notably, around 60% of nurses and 43% of physicians did not perceive any added or reduced workload as a consequence of using computers and the Internet (CGI.br, 2020[13]). Nurses were less likely than physicians to say that computer and Internet use had decreased their workload (17% of nurses compared to 33% of physicians). More broadly, health care professionals has overwhelmingly positive views of the use of electronic systems in their facilities. Around 90% of physicians and nurses considered the implementation of electronic systems improved efficiency in team work. Over 80% agreed that the use of electronic systems resulted in higher quality of care as well as greater efficiency in services.
6.2.3. Effective digital PHC requires a focus on the fundamental enablers
A real digital transformation of PHC in Brazil will not happen without some foundational basics. These basic enablers – individually necessary though not sufficient – include Internet connectivity, appropriate hardware (e.g. computers, tablets, servers, etc.), standards and interoperability for data collection and sharing, software (like EHR systems), ICT security, and, crucially, appropriate training of clinical and managerial staff, including through change management. All these elements require investments and resources at different levels of government, from the federal government all the way down to the municipalities and family health teams.
Reliable energy supply and fast connectivity are indispensable
Appropriate electricity supply and Internet connectivity are vital. As discussed, a significant number of PHC units do not have an Internet connection and a majority have speeds that are likely insufficient to make simultaneous use of EHR systems, high-quality video consultations and remote patient monitoring. Among the main barriers to digitalisation reported by 12 municipalities in the context of the recent pilot project in Alagoas were unreliable electricity supply and a lack of sufficiently fast broadband (Ministério da Saúde, 2020[14]). In some cases, there were no broadband suppliers (ibid). A 2018 study of 91 electricity suppliers serving 81 million households, found the quality of supply varies across regions, with citizens in remote localities, like the Amazonas, having significantly less stable electricity than someone living in São Paulo (Idec, 2018[21]).
Brazil’s geography (nearly eight times the size of France and Spain combined) and sparsely distributed population are certainly challenging for inclusive connectivity (OECD, 2020[22]). The Brazilian Digital Transformation Strategy (E-Digital), along with the Connected Brazil programme, have been instrumental in expanding broadband connectivity (OECD, 2020[11]). Yet, connectivity targets have focused exclusively on schools and have not made explicit mention of concrete connection speeds or reliability. Brazil could explore how rural co-operatives might help bring stable electricity supply and affordable broadband, as done in North Dakota, and build on private sector efforts to connect rural populations in Peru (see Box 6.4).
The Dakota Carrier Network: a consortium of small, independent rural companies and co-operatives
Local mutual and co-operative organisations, which were crucial in bringing electrical and telephone services to rural areas of the United States in the 1900s, are now attempting to do the same with Internet connectivity. With more than 200 rural co-operatives are building advanced broadband networks across the country, evidence suggests these networks may be cheaper and faster than private-sector networks (OECD, 2021[23]). In North Dakota, a rural and sparsely populated state, in 2019, rural residents had better connection speeds than average fibre speeds in both rural and urban areas nationwide. This achievement has been credited to the Dakota Carrier Network, an umbrella organisation made up of small, independent rural companies and co-operatives. With financial support via the federal Broadband Technology Opportunities Programme, besides connecting citizens, the organisation is also deploying a dedicated 10 Gbps network to cover health care providers to enable telemedicine and data exchange.
Internet para Todos: A private sector collaboration to bring Internet connectivity to rural Peru
A collaboration between IDB Invest (the private-sector arm of the IDB Group), Telefónica, Facebook and the Development Bank of Latin America (CAF), Internet para Todos (Internet for All) is a wholesale operator with a new business model that aims to provide Internet connectivity in rural areas of Peru at a profit (IADB, 2020[24]). The financial institutions provide funding with a long-term vision, while Telefónica makes its infrastructure available to rural operators. By the end of 2021, the company expects to have connected 6 million people in more than 30 000 rural areas. Expansion into other parts of Latin America is being considered, starting in Colombia.
Source: OECD (2021[23]), Delivering Quality Education and Health Care to All, https://dx.doi.org/10.1787/83025c02-en; IADB (2020[24]), https://www.iadb.org/en/improvinglives/internet-para-todos-helping-latin-america-log.
Remote and rural municipalities face significant barriers to dependable and fast connectivity, as well as a stable energy supply. These locations often have more limited resources yet face higher costs from broadband suppliers than better resourced large municipalities in urban areas. Partnerships between the Ministry of Health, the Ministry of Science, Technology and Innovation and the Ministry of Defence to connect PHC units, especially in remote locations, are crucial. It is important to evaluate the impact of these initiatives. For example, the already mentioned programme under the RNP that aims to connect 16 000 primary health units is limited to 12 months and does not seem to set concrete targets in terms of connection speeds or reliability. Without adequate Internet connectivity, the poorest and most remote regions of Brazil will be further left behind, with a digital transformation at national level compounding rather than reducing existing regional inequalities.
Purely financial incentives can be helpful but capacity building is still a major barrier
The Connect SUS pilot project in Alagoas provided municipalities with up to USD 1 940 (BRL 10 000) per unconnected PHC unit (Ministério da Saúde, 2020[14]). Despite this, in the period under evaluation, digitalisation in Alagoas lagged behind the average in the Northeast region as well as the overall Brazilian average (ibid). There is no question that financial support is needed to help PHC units and municipalities acquire essential ICT products and services. Yet, the results in Alagoas show financial support alone is not enough. One of the barriers to digitalisation reported by the 12 municipalities in Alagoas was the lack of an implementation team (Ministério da Saúde, 2020[14]).
It is not only digital skills among health care workers that matter, but also the skills, time and ownership needed to drive digitalisation of PHC units. The Alagoas pilot planned to conduct capacity-building workshops in three regions in the State, but due to COVID-19 ended up conducting workshops in only one region. That region (the 1ª Região de Saúde de Alagoas) was responsible for half of the total increase in digitalisation during the pilot. The workshop trained professionals from 19 municipalities on the installation and use of the e-SUS AB EHR system (PEC) and other e-SUS software, as well as training those professionals attending how they themselves could train their colleagues. Another key activity in the workshop was to establish the timeline and responsibilities for implementation of the EHR system. While there are other reasons for the success of the 1ª Região de Saúde de Alagoas, such as high degree of urbanisation, it is likely that the capacity-building workshop had a positive impact.
It is not just health care workers but also crucially managers that lead digitalisation of care services. In England, since 2017, the NHS Digital Academy has been training clinical and information technology leaders to support the digital transformation of the NHS. The Academy is delivered through a partnership between Imperial College London, the University of Edinburgh and the Harvard Medical School (Socha-Dietrich, 2021[25]). Its flagship Digital Health Leadership programme combines content in leadership and change management, health informatics and data analytics, health systems and user centred design, as well as citizen informatics, among other subjects. In Brazil, the implementation of the Programa Educacional em Saúde Digital is a step in the good direction. The programme was instituted in 2020 by the Secretaria de Gestão do Trabalho e da Educação na Saúde and in partnership with the Federal University of Goiás. In 2021, the programme includes specialisation in digital health for both health care workers and health managers at States and Municipal levels.
As mentioned, the EHR system is at the core of digital PHC. It is impossible to send out vaccination alerts, to suggest therapies based on clinical records, and to predict clinical outcomes when patient records are not digitalised. As seen, the large majority of health care facilities, especially smaller PHC practices, do not have decision support and information exchange capabilities within their EHR systems. However, Brazil has shown it is capable of making rapid progress. In just three years (2016-19), the share of public health care facilities with EHR systems capable of (CGI.br, 2020[13]): listing every lab result a patient has had increased from 17% to 41%; listing every patient that is using a specific pharmaceutical went from 18% to 40%; electronic drug prescribing increased from 29% to 51%. These are key functionalities in support of PHC, especially when it is estimated that the purpose of one in five medical appointments is not clinical but to ask for prescriptions and certificates (Mendes, 2011[26]; Marshall, Shah and Stokes-Lampard, 2018[27]). Tying financing of digital PHC to the use of specific functionalities can be a powerful way to increase adoption (more on this in section 6.4.2).
Ensure reliable energy supply and fast connectivity in all PHC units
Set ambitious and clear targets for both reliability and speed of connections as part of existing and future collaborations between the Ministry of Health and other ministries and the RNP to increase Internet connectivity in PHC units. Improve co-operation among governmental entities and across the different levels of government (federal, state and municipal) for implementation of broadband connectivity initiatives.
Expand digitalisation of PHC units through financial support and capacity building
Expand financial payments included in the Connect SUS pilot project of Alagoas to the entire Brazilian territory. Condition receipt of financial support to participation of municipal and state officials in capacity-building workshops, and develop training specifically for senior executives. Set ambitious and clear quantitative targets for adoption and use of EHR systems (such as e-SUS AB), including effective use of electronic drug prescribing and exchange of clinical and administrative data across units. Emphasise importance of cybersecurity as an inevitable consequence of PHC units’ operational dependence on digital systems.
Note: see also recommendations in the OECD Telecommunications and Broadcasting Review of Brazil 2020 (OECD, 2020[22]) and the OECD Reviews of Digital Transformation: Going Digital in Brazil (OECD, 2020[11]), as well as the Recommendation of the Council on Broadband Connectivity (OECD, 2021[28]).
Even if Brazil were to break down all barriers to connectivity and digitalisation of PHC units, there would still persist significant inequalities in the use of digital technologies and tools among its citizens. While the country has made enormous progress in recent years, millions of Brazilians are still digitally excluded, and what is worse there is a clear association between digital and social inequalities in the country. Evidently, digital PHC cannot be effective if populations – especially those that most need it – do not have access to digital services.
6.3.1. Brazilian citizens have never been as connected but clear digital divides persist
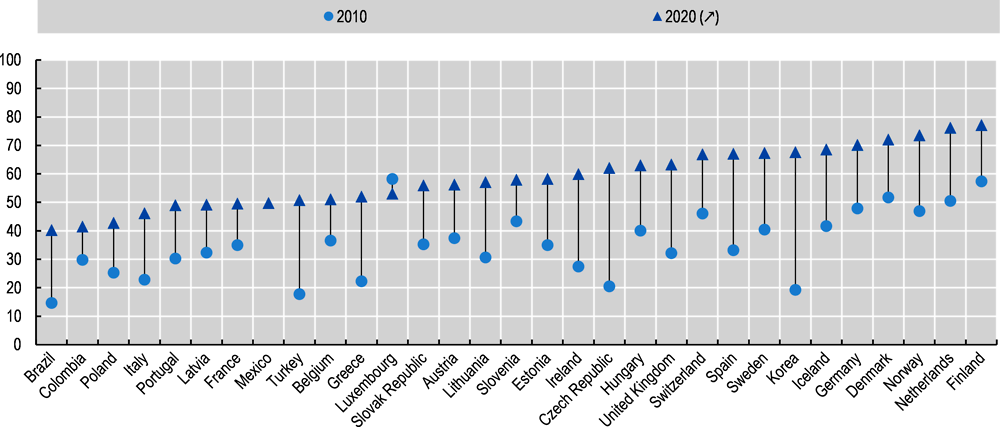
According to the most recent ICT Households Survey, in 2019, 50.7 million Brazilian households (or 134 million individuals) had Internet access (corresponding to 71% of all households), an increase of 5.2 million connected households in relation to 2018 (CGI.br, 2020[29]). Brazilians are more connected but also more digitally engaged. More than two in three Internet users aged 16 or over used electronic government services in 2019 (ibid). Between 2010 and 2019, the share of individuals using the Internet to look for health information more than doubled from around 15% in 2010 to 40% in 2019 (see Figure 6.2). Despite these clear improvements, the country ranks below OECD countries in indicators of digital uptake and use, and digital divides tend to reflect “analogue” divides (OECD, 2020[11]; BNDES, 2017[30]).
Digital divides mirror social inequalities limiting effective digital PHC provision
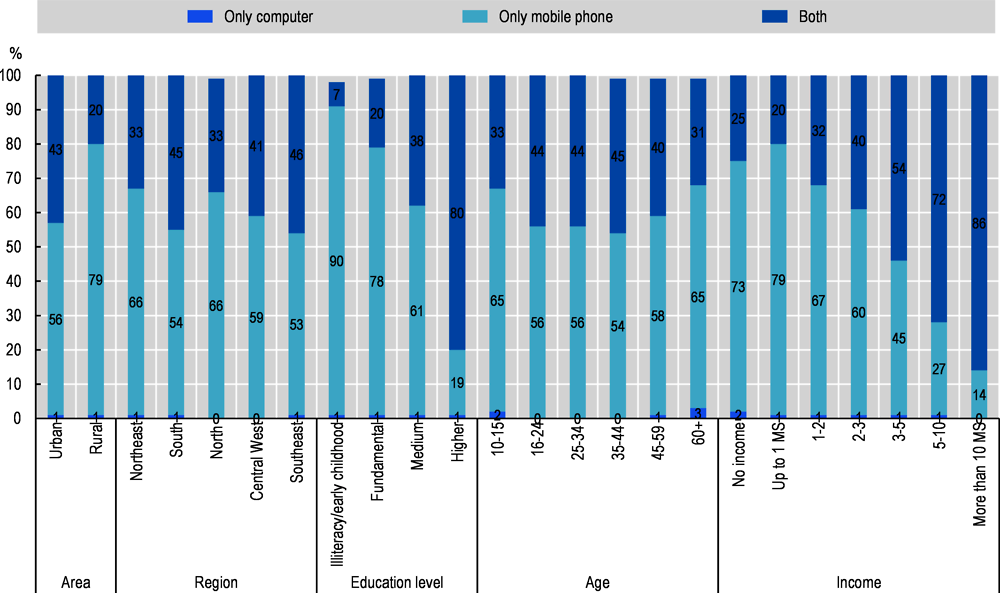
There is a clear association between digital and social inequalities in Brazil (see Figure 6.3). Despite important increases in connectivity, nearly 47 million Brazilians did not use the Internet in 2019 (CGI.br, 2020[29]). Among non-users, the large majority had lower education (85%) and lower socio-economic status or SES (95% belonged to classes C and DE2). Furthermore, regional disparities in use persist. The difference between the proportion of connected households in the Southeast (75%) and the Northeast (65%) regions is of 10 percentage points (ibid). According to the most recent ICT Households Survey (2020[29]), close to 20 million Brazilian households did not have Internet access in 2019, of which 6.4 million households were from the Northeast region. Households with the lowest SES made up the majority of households without Internet access (13 million households in classes DE did not have access in 2019). In 2019, nearly 35 million were disconnected in urban areas (23%) and 12 million in rural areas (47%).
As mentioned, in 2019, 40% of Internet users in Brazil searched for information on health or health care services online (CGI.br, 2020[29]). The share of individuals seeking health information on the Internet was lower among those aged 60 years and older, as well as in groups with lower SES (classes DE). Only 23% of Internet users searched for or used public health services (CGI.br, 2020[29]).
While Brazil has made significant progress in implementing digital government services, certain groups of individuals are not taking full advantage. According to the 2019 ICT Household Survey (2020[29]), those less likely to use e-government services include people aged 60 years and older (46% use e-government services compared to 75% of 25 to 34-year-olds), those with lower education levels (46% of those with elementary education compared to 87% of those with tertiary education), and those from groups with lower SES (48% in classes DE compared to 88% in class A).
6.3.2. Equitable digital PHC starts with ensuring digital uptake and use
It is clear that a digital transformation of PHC can have multiple benefits for populations and individuals, but there is also a risk that digital divides may add to social divides, compounding existing inequalities and deepening social exclusion. With digital divides so clearly aligned with social inequalities in Brazil, there is a serious risk that a digital transformation of PHC will compound existing social divides. An effective digital PHC that reaches all Brazilians is only possible if every citizen is not only connected but can have a say in the design of digital PHC services.
Digital inclusiveness as a foundation for digital PHC for all
Brazil’s policies for digital inclusion have focused on bringing the Internet to remote areas and isolated communities (OECD, 2020[11]). This is the case with the Electronic Government – Citizen Assistance Service (Governo Eletrônico – Serviço de Atendimento ao Cidadão or GESAC) programme, created in 2002 to provide free broadband Internet connections to telecentres, schools, health care units as well as indigenous villages and socially vulnerable communities (OECD, 2018[1]). Other programmes3 include the Digital Inclusion Programme, the Connected Citizen Project, the One Computer Per Student Project and the Telecentros.BR Programme (OECD, 2018[1]). The Internet for All (Internet para Todos) programme is a more recent expansion of the GESAC, focusing on subsidising broadband connections for the more than 30 000 localities and districts in Brazil without a connection.
The creation of telecentres throughout Brazil in the 2000s was one of the first initiatives at the federal level to promote digital inclusion (CGI.br, 2020[31]). Telecentres are public spaces that provide computers with an Internet connection free for anyone to access, as well as workshops, courses and training. According to the most recent ICT Public Access Centres 2019 Survey, which gathers information on telecentres, 45% of telecentres were not operational in the three months prior to the data collection, the most cited reason being a lack of computers and Internet connection, followed closely by lack of maintenance and financial resources (CGI.br, 2020[31]). The number of telecentres in use decreased from the previous Survey in 2013, one possible reason being that the original telecentre programme stipulated that after an initial five-year period of support by the federal government, the equipment would be donated to the municipalities (OECD, 2020[11]).
In 2015, the Federal Audit Office (Tribunal de Contas da União) reviewed public policies related to digital inclusion, finding difficulties in the co-ordination of the different levels of government, limited previous studies to inform and frame new policies and actions, and no systematic monitoring and evaluation of programmes (Tribunal de Contas da União, 2015[32]). In 2018, the Federal Audit Office again drew attention to the lack of co-ordination across the federal, state and municipal governments, and pointed out that many municipalities do not have any telecentres (Tribunal de Contas da União, 2018[33]).
Many policies and programmes to promote digital literacy and ICT use focus on younger people and on schools, which are undeniably important and will lead to improvements in digital inclusion in the coming decades (OECD, 2020[11]). Yet, it is older people who most need and access PHC (Mendes et al., 2019[34]), and more must be done today to include older Brazilians in the digital transformation. Besides strengthening the role of telecentres as providers of training, especially in rural and remote areas, it is important to develop a multi-channel approach to the inclusion of vulnerable groups who are most likely to need and access PHC. Such an approach cannot ignore the crucial role that mobile phones play as a means to access the Internet for older individuals as well as those from rural areas, those on lower incomes, and those with lower levels of education (see Figure 6.4).
Access to mobile broadband is behind the rapid increase in Internet access among the Brazilian population (OECD, 2020[11]). Reliance on mobile connectivity exclusively may prevent some users from accessing more sophisticated services that require higher speeds (e.g. real-time teleconsultations), either because those speeds are not available or data plans are prohibitively expensive. The fact that exclusive use of mobile phones for Internet access is associated with more vulnerable groups could mean that those citizens who most stand to benefit from digital PHC may also be less likely to be able to access it. This is why it is important to adopt a dual strategy of developing new channels to reach these vulnerable groups on mobile platforms, coupled with improvements in high-speed broadband connectivity and digital skills, for example through an expansion of telecentres.
The use of short message service (SMS) and mobile applications to deliver government services is already a reality in many countries, especially in Korea, a country that topped the OECD 2019 Digital Government Index, and where citizens can access government services on their mobile phones. In the United States, the government has set up a mobile first strategy to ensure government services are mobile friendly (United Nations, 2020[35]). In Finland, the government has created a centralised multi-channel one-stop-shop portal that is linked with other specialised portals, thus promoting equity in citizen access to digital government services (ibid).
Adopting a user-driven approach to digital PHC
A user-driven approach describes government actions that allow citizens and businesses to indicate and communicate their own needs and, thereby, drive the design of government policies and public services (OECD, 2020[36]). This requires a shift from a government-centred focus to a user-centred approach that places the needs of users at the core of digital transformation processes and services. A common pitfall of many digital health initiatives is that they fail to adequately engage with health professionals and citizens, leading to products and services that are not relevant to users and add no value (WHO and ITU, 2012[37]).
User needs should be the basis of a digital transformation of PHC. From service design and development through to implementation and monitoring, the user should be present during the entire lifecycle (OECD, 2020[36]). Throughout the process there should be opportunities for feedback and even co-creation. What is key, especially in the Brazilian context, is that a user-driven approach that is accessible and inclusive is also an approach that produces more accessible and inclusive services. Coupled with a strategy to increase digital literacy among citizens, a user-driven approach can engage those citizens that are both most vulnerable and most digitally excluded. Indeed, the now widely used participatory budgeting approach is a Brazilian creation, first implemented in the city of Porto Alegre (OECD, 2019[38]). Participatory budgeting allows citizens a say in how (usually local) budgets are formed and how public moneys are spent. In Porto Alegre, widely seen as a success story, thousands of people have voiced their preferences over the years, affecting how millions of dollars were spent, and importantly – because minorities and vulnerable groups were sometimes overrepresented – shifting public money to where it as most needed (Local Government Association, 2016[39]).
Focus on eliminating digital divides as a foundation for effective digital PHC
Strengthen the role of telecentres as providers of training, especially in rural and remote areas, and ensure appropriate funding and technical assistance at all levels of government. In parallel, develop a multi-channel approach that focuses on mobile access to reach vulnerable groups who are most likely to need and access PHC.
Users must be at the centre, if not drivers, of a true digital transformation of PHC
Develop content, services and applications that meet the needs of both health professionals but especially citizens, particularly those with low digital uptake, e.g. low-educated, low-income and elderly people. Continue to expand patient access to their personal health information.
Note: see also recommendations in the OECD Reviews of Digital Transformation: Going Digital in Brazil (OECD, 2020[11]) and the OECD Digital Government Review of Brazil: Towards the Digital Transformation of the Public Sector (OECD, 2018[1]), as well as the Recommendation of the Council on Broadband Connectivity (OECD, 2021[28]).
Brazil’s government is divided into 26 states and the federal district, and well over 5 000 municipalities. Municipalities are granted the status of federal entities, at the same level as the states. While there is great heterogeneity in the geographical area and population, as well as social and economic indicators, among the subnational jurisdictions, all Brazilian municipalities enjoy the same legal status (OECD/UCLG, 2019[40]). In 2015, 17 municipalities had more than 1 million inhabitants (22% of population). About 44% of municipalities had less than 10 000 inhabitants. Brazil also has 438 health regions, which are made up of municipalities, and are also very heterogeneous in their demographics, socio-economic indicators and governance structures (Ministério da Saúde, 2020[6]). Collaboration and co-ordination across these multiple structures is very challenging, yet it is crucial for a successful digital transformation of PHC.
6.4.1. Brazil’s decentralised government poses challenges to digital PHC
Decentralisation can have economic and administrative benefits, from services that are better aligned with local needs, to more innovative local experimentation, to economic growth driven by competition and accountability in public services (OECD, 2019[38]). However, there are challenges too. Some of the most relevant drawbacks in the context of a digital transformation of PHC in Brazil include overlapping responsibilities, diseconomies of scale, and lack of human and technical capacities.
A digital transformation of PHC cannot take place without adequate governance arrangements, from leadership and co-ordination to institutional models and resources (OECD, 2020[2]). The OECD Digital Government Index sets out four transversal facets that can be used to frame progress towards digital public services, including in PHC (see Box 6.7): a strategic approach with a clear vision, objectives, goals and actions; the specific policy levers and tools to connect strategies to policy actions; implementation capacity that transforms goals and strategies into effective and concrete programmes; and finally monitoring activities to take stock of progress and feedback into strategies.
The OECD Digital Government Index (DGI) is a cornerstone of the OECD work on digital government and public sector data. Built on the OECD Recommendation on Digital Government Strategies, the Index responds to the need for a measurement instrument to track the adoption of digital government policies across OECD member and partner countries. The Digital Government Index draws upon the OECD Digital Government Policy Framework, which characterises a mature digital government as:
being digital by design when governing and leveraging digital technologies to rethink and re-engineer public processes, simplify procedures, and create new channels of communication and engagement with stakeholders;
being data-driven when valuing data as a strategic asset and establishing the governance, access, sharing and re-use mechanisms for improved decision-making and service delivery;
acting as platform when deploying platforms, standards and services to help teams focus on user needs in public service design and delivery;
being open by default when making government data and policy making processes available to the public, within the limits of legislation and in balance with national and public interest;
being user-driven when according a central role to people’s needs and convenience in the shaping of processes, services and policies; and by adopting inclusive enabling mechanisms;
being proactive when anticipating people’s needs and respond to them rapidly, avoiding the need for cumbersome data and service delivery processes.
Source: OECD (2020[2]), Digital Government Index: 2019 results, https://doi.org/10.1787/4de9f5bb-en.
Brazil’s strategic approach is exemplary, embodied in the excellent and comprehensive ESD28. However, like other OECD countries, Brazil has been better at adopting strategies than at promoting and monitoring their implementation. The ESD28 sets out an ambitious vision for digital health in Brazil, but it will be difficult to realise. This is because there are significant risks, as identified in the WHO/ITU National eHealth Strategy Toolkit (2012[37]), namely: insufficient and geographically imbalanced resource capacity, scarce funding, too broad of an implementation focus, and unavailability of required infrastructure (this last one has already been discussed in previous sections). To these barriers, one can add a lack of clarity in the assignment of responsibilities across levels of government.
In Brazil, the division of responsibilities is unclear in a number of areas, including in health care (OECD, 2019[38]). This is frequently the case in policy areas that are “shared” across levels of government, as is the case with health care in Brazil. This can result in duplication, cost shifting and scale inefficiencies. The government’s 2017 eHealth Strategy noted that initiatives to create a national eHealth architecture had lacked alignment and continuity, leading to frustration, scepticism that such a programme could work and demotivation in tackling the inevitable barriers (Ministério da Saúde, 2017[10]). It was also mentioned that strategies and investments had been traditionally defined and executed in isolation by the federal, state and municipal governments. Despite the existence of high-quality initiatives in digitalising health care, these remained “islands of excellence” due to a lack of integration across levels of government (Ministério da Saúde, 2017[10]).
Small municipalities, especially, face significant barriers to digitalisation of PHC units and teams. Because responsibilities are “shared”, the three levels of government are often dependent on each other to implement the actions set out in the ESD28. This can lead to delays in adoption due to holdups in different levels of government (Andrade et al., 2019[41]). Municipalities are responsible for many key steps in digitalising PHC, from purchasing ICT equipment and software to hiring ICT specialists. Smaller municipalities may have limited capacity to manage these processes. One example is the requirement that the contracting of essential services be renewed every five years, which has been flagged as an impediment to the expansion and upkeep of ICT infrastructure (Ministério da Saúde, 2017[10]). It is not uncommon for smaller municipalities, and even larger ones, to not have any long-term ICT planning (Veloso et al., 2011[42]).
Financial commitments have also perhaps not been as ambitious as the agendas set out in previous strategies and in the ESD28. This has led to a situation in which some municipalities are responsible for digitalising PHC services but lack the necessary resources to do so. In other words, these are unfunded mandates (OECD, 2019[38]). Since 2014, the Ministry of Health has provided a monthly payment of USD 117 (BRL 603.38) for PHC units who seek to improve their connectivity (Ministério da Saúde, n.d.[43]). The target was to connect 12 000 units, however only 8 000 had been connected and only 4 800 were sending data back to the Ministry of Health.
More recently, the Informatiza APS programme provides monthly support of USD 330 (BRL 1 700) to USD 388 (BRL 2000) to family health teams that are able to collect and send data to central repositories. A key eligibility requirement of the programme is that family health units need to already be using digital technologies. The pilot project in the state of Alagoas has expanded support to include an additional financial incentive for PHC units that have not yet been able to digitalise (a lump sum of between USD 1 649 (BRL 8 500) and USD 1 940 (BRL 10 000) to each municipality in Alagoas for every PHC unit that was not yet digitalised). As this is still a pilot, this form of pre-digitalisation support is not yet available for all municipalities. In light of the COVID-19 pandemic, the Ministry of Health did institute a time-limited incentive of USD 5 268 (BRL 27 157) to be paid to municipalities and states for each health team that has not yet been digitalised, but it is still too early to know what impact this has had on the numbers of PHC units without computers and Internet access.
6.4.2. Moving from digital strategies to implementation and monitoring
Determining which level of government should take over which responsibility related to digitalisation is not without challenge, but it is also of the utmost importance. Clear assignment of responsibilities is crucial for accountability, monitoring and effectiveness of investment (OECD, 2019[38]). Particularly with shared responsibilities, as is the case with health care in Brazil, clarity is all the more important, so that all parties mutually understand what their individual responsibilities are. It is important to avoid multiple co-ordination mechanisms with no clear role in decision-making processes (OECD, 2019[38]). Finally, it is vital to build the necessary capacity to deliver on mandates. This means aligning funding with functional responsibilities to avoid unfunded mandates, but also encouraging sharing of best practices and specialised knowledge across jurisdictions, making expertise available to all levels independent of size (OECD, 2019[38]).
Setting clear well-funded mandates for digitalisation at the right levels of government
A major barrier to digital PHC in Brazil is human and technical capacity in municipalities. Having more than 5 500 municipalities procure ICT products and services for over 42 000 PHC units every five years is not good practice. Around one in five Brazilian municipalities have less than 5 000 inhabitants, and yet they are responsible for hiring ICT specialists and purchasing ICT products and services, from hardware to software, to connectivity and cybersecurity. Often, municipalities either have no providers to choose from, or face prohibitively high costs. As the pilot project in Alagoas has demonstrated, municipal managers lack the capacity to digitalise, even when financing is provided by federal and state governments (Ministério da Saúde, 2020[14]). Setting responsibilities for digitalisation of PHC at municipal level for all of Brazil is likely leading to diseconomies of scale, and creating challenges for small municipalities that do not have the human and technical capacities.
In OECD countries with small subnational government units, such as the Nordic countries, France, the Slovak Republic and Spain, subnational partnerships, joint authorities and outsourcing are frequently used to create scale economies (OECD, 2019[38]). In the context of digital health, specifically, regional health authorities that bring together smaller jurisdictions and provide shared services to all members are a way to achieve both economies of scale and valuable expertise. For example, in New Zealand, primary health organisations or PHOs, especially larger PHOs like ProCare (which serves 800 000 patients in greater Auckland), offer its member practices a centralised human resource, practice management and procurement service (Varsamis, 2019[44]).
Established in 2005, the English NHS Shared Business Services (SBS) provide a mix of finance and accounting, procurement, digital innovation services, employment services, innovation and technology services, and change management to hundreds of NHS organisations (NHS Shared Business Services, 2020[45]). Through a partnership with the Royal Papworth Hospital NHS Foundation Trust, NHS SBS has developed a digital patient booking system that can be rolled out to all NHS organisations (ibid). Also in the United Kingdom, the NHS GP IT Futures programme will create a new environment for the supply of clinical ICT systems to general practice, including a new online NHS Digital Buying Catalogue to find PHC technology systems and services (NHS Digital, 2020[46]). In Portugal, the Shared Services of the Ministry of Health (SPMS) is the Ministry’s central purchasing and ICT authority, providing shared services in the areas of purchasing and logistics, financial services, human resources and ICT. Recently, SPMS added new electronic dynamic purchasing systems for NHS organisations to procure consultancy services in blockchain, artificial intelligence, telemedicine and mHealth from providers that have been certified (SPMS, 2020[47]).
Brazil could look to these examples from New Zealand, England and Portugal for a new model of shared services for digital PHC. Given the geography, population and population density of Brazil, shared services and responsibilities could be aggregated at the level of the federal government, state governments or even health macro-regions and regions, depending on the specific service being considered. For example, dynamic purchasing systems can be set up by the federal government, building on the experiences of the Co-ordenação-Geral de Tecnologia da Informação e Comunicações (CGTIC), which already plans, co-ordinates, supervises and guides ICT investments for the federal government. For smaller states (like Roraima, Amapá and Acre), health macro-regions and bigger health regions could then set up agencies for shared services, providing specialised human resources, purchasing and management services for digital PHC to municipalities.
There are three important policy levers to carry out this regionalisation of competencies for digital PHC:
First, it is crucial that standards and interoperability remain a central federal responsibility. This does not mean that these should be developed by only the federal government, but it does mean that states and municipalities should participate in this process rather than lead it. This would ensure that whatever systems are procured by states and municipalities, the ability to share data and patient mobility remain possible throughout Brazil.
Second, these new mandates need to be adequately funded and responsibilities be clearly set. This would guarantee that the new shared services agencies are both able to execute their responsibilities and accountable for the results.
Third, local leadership, community participation and local ownership remain essential (OECD, 2019[38]). A new model of shared services needs to have the buy-in and ownership of the municipalities and PHC units it is supposed to serve.
Larger and smarter investments are needed to deliver on ambitious digital health strategies
Digitalisation requires investments in infrastructure and connectivity (e.g. high speed broadband), in hardware (e.g. computers), software (e.g. EHR systems), specialised human resources (ICT specialists), user training (e.g. digital literacy of professionals and patients), and importantly, though often neglected, change management and implementation. Brazil has invested significantly in connectivity (e.g. GESAC) and software (e.g. e-SUS AB), as well as providing support for hardware and training (e.g. Informatiza APS). However, as seen in previous sections, substantial numbers of PHC units and teams, as well as citizens, remain disconnected, and thus unable to benefit from a digital transformation of PHC. The vision set out in ESD28 and previous digital health strategies requires both larger and smarter investments, tying financial support to effective and equitable use.
The International Telecommunication Union has recently estimated that connecting every Brazilian to the Internet would cost USD 11.1 billion (ITU, 2020[48]). Brazil’s Connect SUS programme is likely to involve total investments of USD 0.77-1.16 billion (BRL 4-6 billion) over five years (OECD, 2020[11]). In 2019, according to the World Bank Group, Brazil had a population of 211 million and a gross domestic product (GDP) of USD 1.84 trillion. By comparison, in Sweden, a country that in 2019 had just over 10.2 million inhabitants and a GDP of USD 530 billion, the country’s 21 regions invest around USD 1.2 billion annually in health care ICT (U.S. Department of Commerce, 2020[49]). Only 1% of Swedish drug prescriptions are issued in paper format (ibid).
As previously discussed, Brazil instituted an exceptional incentive for municipalities and states digitalise PHC units, budgeting over USD 83.8 million (BRL 432 million) for 2020 (Diário Oficial da União, 2020[50]). In the United States, the FCC’s Emergency Broadband Benefit is a USD 3.2 billion progamme to support households struggling to pay for internet service during the pandemic, providing monthly discounts towards broadband service, as well as one-time discounts to purchase equipment like laptops or tablets, with higher discounts on Tribal lands (FCC, 2021[51]). The FCC’s COVID-19 Telehealth Program provides USD 200 million in immediate support to nonprofit and public eligible health care providers responding to the COVID-19 pandemic by fully funding their telecommunications services, information services, and devices necessary to provide critical connected care services (FCC, 2021[52]).
While it is challenging to compare investments across different geographies, populations and economies, it is helpful to place financial commitments across countries in the contexts of their digital health strategies. The Brazilian ESD28 sets out an ambitious agenda, including milestones for the achievement of certain capabilities (e.g. ePrescribing by December 2022). Looking to the order of magnitude of investments in countries that have already achieved these milestones is a practical way to assess whether current investments are sufficient. As an example, in the United Kingdom, a USD 33.3 million (GBP 26 million) national fund has been set up to have all NHS doctors, nurses and other clinical staff on e-rostering systems by 2021 (GOV.UK, 2021[53]). E-rostering, which allows clinicians to select shifts digitally, providing them with more flexibility and more efficient work schedules, is just one capability.
Investments should also be comprehensive in their scope. It is often the case that one of the most important steps in implementing new technologies – change management and support for implementation – is not appropriately funded (Varsamis, 2019[44]). As the pilot project in Alagoas illustrates, it is possible to have buy-in from municipalities, provide funding, and still have limited adoption. While support in the form of capacity building is undoubtedly important, it might need to be combined with financial support for lost productivity and service disruption during periods of change and adaptation (Bakhai et al., 2019[54]).
It is not just the magnitude of investments that matters. Conditions for accessing these funds by the beneficiaries can promote, or hinder, the adoption and everyday use of digital technologies. Tying financial support to the use of specific functionalities or programmes can be a way to target investments and increase their effectiveness. The Informatiza APS programme already does this by conditioning eligibility for financial support to the reporting of data to the SISAB, but it can potentially go further. The Australian Practice Incentives Program (PIP) eHealth Incentive encourages practices to adopt key digital services, from patient records to secure messaging capabilities (to communicate with both patients and other practices), to ePrescribing, among others (Australian Government, 2016[55]).
Finally, while a digital transformation of PHC has enormous potential (see Box 6.2), there is little high-quality evidence regarding recent digital-first PHC models, such as the one being implemented in the United Kingdom (Rodgers et al., 2019[56]). It is important that funds be made available for continuous monitoring and evaluation of digitalisation in PHC in Brazil.
Set clear well-funded mandates for digitalisation at the right levels of government
Consider aggregating shared services and responsibilities related to digitalisation of PHC at less decentralised levels. Build on experiences of the CGTIC to explore setting up dynamic purchasing systems at federal level, with appropriately funded agencies at state or regional level providing specialised human resources, purchasing and management services for digital PHC to municipalities.
Make larger and smarter investments to promote baseline digital PHC services for all
Review magnitude of investments needed to deliver on vision of ESD28, including funding for change management, capacity building, and monitoring and evaluation. Tie financial support to specific milestones in the adoption and use of digital PHC functionalities, starting with ePrescribing, referral management, appointment scheduling and patient access to EHR.
Note: see also recommendations in Making decentralisation work: A handbook for policy makers (OECD, 2019[38]) and in the OECD Digital Government Review of Brazil: Towards the Digital Transformation of the Public Sector (OECD, 2018[1]).
Over the last decades, Brazil has been making impressive progress towards a digital transformation of its public sector, and is aiming to offer all of its more than 3 000 public services via digital channels by the end of 2022 as part of its Digital Government Strategy 2020-22. The country has made significant inroads also in building a foundation for digital PHC, with successive ambitious and comprehensive digital health strategies, coupled with vital investments in hardware, interoperability and skills. However, progress towards effective use of digital technologies in PHC has been slow, and fundamentally unequal. Thousands of PHC units have no computers or Internet access. Only 17% of PHC units have speeds over 10 Mbps. Around 18 000 health care facilities (or 18% of all facilities) do not have an EHR system. The COVID-19 pandemic has likely accelerated the adoption of digital technologies but its true impact remains unclear for now.
At the same time, and despite significant progress in recent years, millions of Brazilians are still digitally excluded. More than two in three Internet users aged 16 or over used electronic government services in 2019, and the share of individuals using the Internet to look for health information more than doubled between 2010 and 2019. However, nearly 47 million Brazilians did not use the Internet in 2019. Digital divides are also clearly associated with social inequalities, with older Brazilians, those from rural areas, those with lower incomes and lower education levels all less likely to use the Internet, and more likely to use mobile phones only. There is thus a serious risk that a digital transformation of PHC will only compound existing social divides.
Against this backdrop, Brazil’s decentralised government creates challenges to digitalising PHC. The country’s 26 states, one federal district, well over 5 000 municipalities (around 44% of which had less than 10 000 inhabitants), and 438 health regions are very heterogeneous in their demographics, socio-economic indicators and governance structures. The municipality of Serra da Saudade, with around 800 inhabitants, has the same responsibilities to manage the digitalisation of PHC as the municipality of São Paulo, with its over 12 million inhabitants. There are significant risks for the country’s ambitious strategy for digital health, including insufficient and geographically imbalanced resource capacity, scarce funding, too broad of an implementation focus, and unavailability of required infrastructure.
Brazil has established a solid basis on which to build an effective, equitable and efficient digital PHC. But, to do so, it must tackle three sets of interconnected challenges: digitalisation of all PHC units and teams; digital inclusion for all Brazilian citizens, especially those that are most vulnerable; and a governance structure that is fit to deliver a digital transformation of PHC, by setting clear well-funded mandates at the right levels of government.
References
[41] Andrade, M. et al. (2019), “Challenges and lessons from a primary care intervention in a Brazilian municipality”, Revista de Saúde Pública, Vol. 53, https://doi.org/10.11606/S1518-8787.2019053000457.
[55] Australian Government (2016), Practice Incentives Program eHealth Incentive Guidelines, https://www.servicesaustralia.gov.au/sites/default/files/ehealth-incentive-pip-guidelines.docx (accessed on 10 March 2021).
[54] Bakhai, M. et al. (2019), Using Online Consultations In Primary Care Toolkit – First edition, https://www.england.nhs.uk/wp-content/uploads/2020/01/online-consultations-implementation-toolkit-v1.1-updated.pdf (accessed on 10 March 2021).
[30] BNDES (2017), Produto 8: Relatório do Plano de Ação.
[16] Brasil Telemedicina (2020), Sobre nós, https://brasiltelemedicina.com.br/sobre-nos/ (accessed on 5 March 2021).
[18] Caetano, R. et al. (2020), “Challenges and opportunities for telehealth during the COVID-19 pandemic: Ideas on spaces and initiatives in the Brazilian context”, Cadernos de Saude Publica, Vol. 36/5, https://doi.org/10.1590/0102-311X00088920.
[7] Castle-Clarke, S. and C. Imison (2016), The digital patient: transforming primary care?, Nuffield Trust, https://www.nuffieldtrust.org.uk/files/2017-06/1497259 872_nt-the-digital-patient-web-corrected-p46-.pdf (accessed on 29 April 2019).
[15] CGI.br (2020), ICT Electronic Government 2019, Comitê Gestor da Internet no Brasil, São Paulo.
[29] CGI.br (2020), ICT Households Survey 2019, Comitê Gestor da Internet no Brasil, São Paulo.
[13] CGI.br (2020), ICT in Health 2019, Comitê Gestor da Internet no Brasil, São Paulo.
[31] CGI.br (2020), ICT Public Access Centers Survey 2019, Comitê Gestor da Internet no Brasil, São Paulo.
[4] Diário Oficial da União (2020), DECRETO Nº 10.332, DE 28 DE ABRIL DE 2020.
[50] Diário Oficial da União (2020), PORTARIA Nº 3.193, DE 27 DE NOVEMBRO DE 2020.
[52] FCC (2021), COVID-19 Telehealth Program | Federal Communications Commission, https://www.fcc.gov/COVID-19-telehealth-programme (accessed on 10 March 2021).
[51] FCC (2021), Emergency Broadband Benefit | Federal Communications Commission, https://www.fcc.gov/broadbandbenefit (accessed on 10 March 2021).
[3] gov.br (2020), Estratégia de Governo Digital – 2020 a 2022, https://www.gov.br/governodigital/pt-br/EGD2020/ (accessed on 4 March 2021).
[53] GOV.UK (2021), GBP 7.5 million to digitally schedule shifts and save NHS staff time, https://www.gov.uk/government/news/75-million-to-digitally-schedule-shifts-and-save-nhs-staff-time (accessed on 10 March 2021).
[12] Harzheim, E. et al. (2020), “New funding for a new Brazilian primary health care”, Ciencia e Saude Coletiva, Vol. 25/4, pp. 1361-1374, https://doi.org/10.1590/1413-81232020254.35062019.
[24] IADB (2020), This project will connect 6 million Peruvians to the Internet for the first time, https://www.iadb.org/en/improvinglives/internet-para-todos-helping-latin-america-log (accessed on 8 April 2021).
[21] Idec (2018), Avaliação da qualidade do serviço de fornecimento de energia das Concessionárias e Permissionárias Brasileiras, Instituto Brasileiro de Defesa do Consumidor, São Paulo.
[48] ITU (2020), Connecting humanity: Assessing investment needs of connecting humanity to the Internet by 2030.
[39] Local Government Association (2016), Case study: Porto Alegre, Brazil, https://www.local.gov.uk/case-study-porto-alegre-brazil (accessed on 8 April 2021).
[27] Marshall, M., R. Shah and H. Stokes-Lampard (2018), “Online consulting in general practice: making the move from disruptive innovation to mainstream service”, BMJ, https://doi.org/10.1136/bmj.k1195.
[26] Mendes, E. (2011), As redes de atenção à saúde, nização Pan-Americana da Saúde, Brasília.
[34] Mendes, E. et al. (2019), A construção social da atenção primária à saúde, CONASS, Brasília.
[5] Ministério da Saúde (2020), Estratégia de Saúde Digital para o Brasil 2020-28, http://bvsms.saude.gov.br/bvs/publicacoes/estrategia_saude_digital_Brasil.pdf (accessed on 4 March 2021).
[6] Ministério da Saúde (2020), Plano Nacional de Saúde 2020-23.
[14] Ministério da Saúde (2020), Relatório Final do Projeto Piloto Conecte SUS: análise dos avanços obtidos entre outubro/2019 e junho/2020, Ministério da Saúde, Brasília.
[10] Ministério da Saúde (2017), Estratégia e-Saúde para o Brasil.
[43] Ministério da Saúde (n.d.), Saber online como é investido cada real do SUS na saúde do brasileiro, https://www.gov.br/saude/pt-br/centrais-de-conteudo/e-sus-ab-pdf (accessed on 9 March 2021).
[46] NHS Digital (2020), GP IT Futures systems and services, https://digital.nhs.uk/services/gp-it-futures-systems (accessed on 9 March 2021).
[45] NHS Shared Business Services (2020), ANNUAL REPORT AND FINANCIAL STATEMENTS.
[28] OECD (2021), Recommendation of the Council on Broadband Connectivity, OECD/LEGAL/0322.
[23] OECD (2021), Delivering Quality Education and Health Care to All: Preparing Regions for Demographic Change, OECD Rural Studies, OECD Publishing, Paris, https://dx.doi.org/10.1787/83025c02-en.
[2] OECD (2020), “Digital Government Index: 2019 results”, OECD Public Governance Policy Papers, No. 3, OECD Publishing, Paris, https://doi.org/10.1787/4de9f5bb-en.
[11] OECD (2020), Going Digital in Brazil, OECD Reviews of Digital Transformation, OECD Publishing, Paris, https://dx.doi.org/10.1787/e9bf7f8a-en.
[22] OECD (2020), OECD Telecommunication and Broadcasting Review of Brazil 2020, OECD Publishing, Paris, https://dx.doi.org/10.1787/30ab8568-en.
[36] OECD (2020), “The OECD Digital Government Policy Framework: Six dimensions of a Digital Government”, OECD Public Governance Policy Papers, No. 2, OECD Publishing, Paris.
[9] OECD (2019), Health in the 21st Century: Putting Data to Work for Stronger Health Systems, OECD Health Policy Studies, OECD Publishing, Paris, https://dx.doi.org/10.1787/e3b23f8e-en.
[38] OECD (2019), Making Decentralisation Work: A Handbook for Policy-Makers, OECD Multi-level Governance Studies, OECD Publishing, Paris, https://dx.doi.org/10.1787/g2g9faa7-en.
[1] OECD (2018), Digital Government Review of Brazil: Towards the Digital Transformation of the Public Sector, OECD Digital Government Studies, OECD Publishing, Paris, https://dx.doi.org/10.1787/9789264307636-en.
[40] OECD/UCLG (2019), 2019 Report of the World Observatoryon Subnational Government Finance and Investment – Country Profiles, https://www.sng-wofi.org/publications/SNGWOFI_2 019_report_country_profiles.pdf.
[19] ONC (2019), What is the recommended bandwidth for different types of health care providers? | HealthIT.gov, https://www.healthit.gov/faq/what-recommended-bandwidth-different-types-health care-providers (accessed on 29 January 2021).
[56] Rodgers, M. et al. (2019), “Informing NHS policy in ‘digital-first primary care’: a rapid evidence synthesis”, Health Services and Delivery Research, Vol. 7/41, pp. 1-124, https://doi.org/10.3310/hsdr07410.
[20] Santos, A. et al. (2016), “Telehealth in the Amazon Region in Latin America: an Overview”, Journal of the International Society for Telemedicine and EHealth, Vol. 4/e12, pp. 1-7, https://journals.ukzn.ac.za/index.php/JISfTeH/article/view/149 (accessed on 5 March 2021).
[25] Socha-Dietrich, K. (2021), Empowering the health workforce to make the most of the digital revolution, OECD Publishing, Paris, https://doi.org/10.1787/37ff0eaa-en.
[47] SPMS (2020), Boletim Informativo Compras Públicas na Saúde nº 45, https://www.spms.min-saude.pt/wp-content/uploads/2020/02/Boletim-CPS_N45.pdf (accessed on 9 March 2021).
[17] Telelaudo (2021), Telelaudo. Sua Equipe Sempre Completa., https://www.telelaudo.com.br/ (accessed on 7 April 2021).
[57] The King’s Fund, The Health Foundation and Nuffield Trust (2018), The health care workforce in England: make or break?, http://www.hee.nhs.uk/news-blogs-events/news/hee-launches-plan-future-proof-nhs-care-workforce (accessed on 5 May 2019).
[33] Tribunal de Contas da União (2018), TC 012.352/2018-7.
[32] Tribunal de Contas da União (2015), Política pública de inclusão digital, Tribunal de Contas da União, Brasília.
[49] U.S. Department of Commerce (2020), Sweden eHealth, https://www.trade.gov/market-intelligence/sweden-ehealth (accessed on 9 March 2021).
[35] United Nations (2020), E-Government Survey 2020 – Digital Government in the Decade of Action for Sustainable Development, United Nations, New York.
[44] Varsamis, D. (2019), Incentives and levers for digitising and integrating primary care in New Zealand, Australia and the USA – lessons for the UK NHS, Winston Churchill Memorial Trust, https://www.wcmt.org.uk/sites/default/files/report-documents/Varsamis%20D%202 019%20Final_0.pdf (accessed on 9 March 2021).
[42] Veloso, J. et al. (2011), “Uma Visão Inicial dos Subsistemas da Gestão Pública Municipal”, in Veloso, J. et al. (eds.), Gestão Municipal no Brasil: um retrato das prefeituras, Ipea, Brasília.
[37] WHO and ITU (2012), National eHealth strategy toolkit.
[8] World Health Organization (2018), Digital technologies: shaping the future of primary health care, https://apps.who.int/iris/bitstream/handle/10665/326573/WHO-HIS-SDS-2018.55-eng.pdf?sequence=1&isAllowed=y (accessed on 22 January 2021).
Notes
← 1. Here and throughout this chapter, an exchange rate of BRL 5.155/USD for the year 2020 from https://stats.oecd.org.
← 2. The 2020 Brazilian Criteria for Economic Classification (Critério de Classificação Econômica Brasil) defines six classes (A, B1, B2, C1, C2, DE) of socio-economic stratificaiton based on a system of points that aggregates survey data on wealth, living conditions, education and income. Category A represents a higher socio-economic status.
← 3. See also Table 3.1. in (OECD, 2020[11]).