copy the linklink copied!1. Bringing health into the 21st century
Luke Slawomirski
This chapter provides the key findings and overarching themes of the entire report Health in the 21st Century: Putting data to work for stronger health systems, which explores how digital technologies – and especially electronic data, can be put to work with the goal of effecting positive health system transformation. This question is approached from several perspectives: improving health service delivery models, empowering patients and health system users, readying the health workforce to make the most of digital technologies such as artificial intelligence (AI), using big data in public health policy, the importance of cross-border collaboration, using routine and real-world data to generate evidence on treatments and therapies, and improving overall health system governance and stewardship. The overarching messages from these studies are outlined here. The chapter also provides an estimate of the potential health and economic return of investing in a digital transformation of the health sector in OECD countries.
copy the linklink copied!1.1. Introduction
Digital technology plays a fundamental part in just about every facet of human activity. Its scale, reach and expansion is certainly colossal. For example, OECD countries currently have about one mobile internet subscription per inhabitant. Mobile data usage more than doubled in most OECD countries between 2015 and 2017. By 2021, three connected devices will exist per person around the globe (OECD, 2019[1]).
People now have access to an unprecedented amount of information literally in the palm of their hand. Digital technology – or more accurately, information and communication technology (ICT) – enables us to interact with, manage and share information with others like never before. As a result, most of humankind now inhabits a global ‘infosphere’, which has fundamentally altered the way people act and interact (Floridi, 2014[2]). The social and economic impact of this digital transformation (Box 1.1) is rightly compared to previous industrial revolutions (OECD, 2019[1]).
While technologies such as the internet, the smartphone, blockchain and artificial intelligence (AI) may be the instruments of digital transformation, electronic data are its lifeblood. The world now creates more than 2.5 quintillion (2.5x1018) bytes of data every day, meaning that more data have been generated in the last few years than since the dawn of civilisation (IBM, 2017[3]; DOMO, 2017[4]). Almost every human activity now generates data. Modern household appliances are on the internet of things (IoT). This means that people’s daily digital footprint will soon begin not only when they check their smartphones, but when they open their ‘smart fridge’ in the morning.
The fundamental economic characteristic of data (and intangible digital products such as software) is that they have no mass, and can be used and re-used without depletion and at very low marginal cost.1 Data generated for a certain purpose may be re-deployed in countless ways to answer new questions, build knowledge and generate insights. They are a highly valuable resource and a genuine factor of economic production. Data availability is even used in some countries to attract international investment (Will, 2011[5]; Ministry of Foreign Affairs Denmark, 2016[6]). Data also exhibit many of the qualities of a public good,2 which makes them particularly interesting to governments and suitable for public policy.
Sectors ranging from, finance, insurance and retail to education, transport and defence have certainly taken advantage of data and digital technology to achieve their objectives, and improve their products and services. The transformation has generated immense value through consumer surpluses and social dividends, as well as profits on the supply side.
The implications for health, a sector where information is critical to success, are profound. Health systems3 now produce as much as 30% of the world’s stored data (Huesch and Mosher, 2017[7]). Collectively, these data contain an immense amount of useful information on health, disease and on how effectively, equitably and efficiently health systems perform. Also, people’s daily digital footprint can reveal a lot about their health. Grocery purchases, smartphone app data, web-browsing and social media content all make up an individual’s ‘digital phenotype’. A recent study used people’s web browsing data (the words typed into search engines) to accurately predict the timing and reason for visiting a hospital emergency room (Asch et al., 2019[8]). But the health sector has been remarkably slow to capitalise on these opportunities.
This report explores how health systems can more effectively harness data and digital technology to initiate a positive transformation. This chapter presents its key findings and themes. Section 1.2 examines why health has been so slow to harness the opportunities. The section highlights the key enablers of digital transformation in other sectors that are relevant to health systems, and serves as a precursor to the remaining messages of the chapter and the report. Section 1.3 explores the opportunities presented by data and digital technologies in health. It also summarises how most health systems remain ‘data rich but information poor’. Section 1.4 examines the barriers to a digital transformation and outlines the organisational, structural and institutional changes needed to address them. Section 1.5 then makes key recommendations for policy makers to move this agenda forward. The section also estimates the health and economic returns on investing in a digital transformation in health.
Digital technology refers to electronic tools, systems, devices and resources that generate, store, process and/or transmit data. These range from devices such as smartphones and computers to intangible products such as software, web-based information and communication platforms such as electronic medical records, Artificial Intelligence (AI) and machine-learning algorithms. The internet, for example, itself is a ‘general purpose’ digital technology, which has had a profound social and economic impact.
In this report, digital technology is used interchangeably with information technology (IT) as well as information communication technology (ICT). The latter stresses the role of telecommunications in the transmission of data and information and is used frequently in this report.
Data are units of information encoded electronically in binary, machine-readable format used by and produced by digital technologies. Health data usually consists of individual, personal health and other related information. These can include a range of data about an individual: history of all medical diagnoses, diseases and medical interventions, medications prescribed, test results, imaging. These may contain information on mental health, genetics, behavioural patterns and social and economic factors. They also include health care administrative data: admissions and discharge data routine operational data, insurance and financial transactional data. Depending on the purpose, health data can identify the individual but can also be anonymised and de-identified.
Digitalisation is the use of digital technologies and data as well as interconnection that results in new activities or in changes or adaptation to existing activities. It is quite distinct to digital transformation, which refers to the economic and societal effects of digitalisation as well as its enabling factors such as adaptation and transformation of organisational structures, processes and behaviour.
This report is principally concerned with leveraging electronic data to generate knowledge and information for improving policy and practice. Examining digitalisation or specific digital technologies is not the main focus. Data underpin of digital technology, but without digital technology data can not be ‘put to work’. The report therefore describes these technologies where relevant. For example, machine-learning algorithms that can interpret medical images, assess the risk of a hospital admission or stratify populations based on health need are examined here. However, these technologies run on data to learn and execute the task(s) they are designed for.
Use of data can be primary or secondary. All data are generated for a specific reason – their primary use. For example, the primary use of insurance claims or administrative hospital data generate information used for management and reimbursement. However, these data can also be deployed (and re-deployed) for secondary clinical, managerial, policy and uses such as examining the safety and efficiency of health care organisations, or the performance of specific therapies and treatments.
Source: European Group on Ethics in Science and New Technologies (EGE), Opinion No 13: Ethical Issues of Health Care in Information Society.
copy the linklink copied!1.2. The health sector is slow to embrace a digital transformation – this requires urgent attention
Many sectors have taken advantage of digital technology. This has led to continual improvement of services and products, and the creation of considerable value on the supply and demand side of the global economy (OECD, 2019[1]). For example:
-
Analysis of customer data is used by the airline, banking and retail sectors to improve responsiveness to needs and expectations (OECD, 2017[9]).
-
In education and insurance, predictive analytics, machine learning and AI provide information on expected behaviour and activity (OECD, 2017[9]).
-
Large datasets are used to stratify populations for more effective and targeted interventions in areas ranging from retail to politics. Real-time data analytics are able to identify fraud by detecting even small deviations from expected activity (Bates et al., 2018[10]).
-
By making existing data publicly available, the Transport Authority of London has generated estimated savings of GBP 130 million per annum for customers, road users as well as public and commercial entities who use these data to inform transportation decision in real-time (OECD, 2019[1]).
Firms, organisations and entire sectors quickly recognised that, unlike other resources, intangible digital goods such as data or software are non-rivalrous and can be shared, used and re-used at very low marginal cost. Data and information are now considered a factor of production – albeit a very unique one – alongside labour, capital and raw materials (Murdoch and Detsky, 2013[11]). For example, routine commercial flights generate a large volume of data on the performance of the aircraft and its component parts, as well as real-time weather information. These data are fed back to the airline. They are also shared with regulators and with manufacturers for analysis aimed at continual improvement along the entire supply chain. Air travel is now one of the safest modes of transport available, and has never been cheaper or more accessible (OECD, 2017[9]).
The health sector provides a stark contrast. Take for instance, the fact that health systems generate mountains of data, but do not routinely re-purpose these for assessing the performance and value of treatments. In some places, it is not possible to detect when patients are re-admitted to hospital if this occurs a different location. More fundamentally, health is one of the few sectors where technological advances result in higher costs and expenditure (OECD, 2017[12]; Marino and Lorenzoni, 2019[13]).
To put it plainly, the sector is a decade or so behind. This represents a considerable amount of foregone health and economic benefits. Despite some signs of progress – discussed below and in the substantive chapters of this report – the consensus is that health systems could and should be doing much more to put data and digital technologies to work.
1.2.1. Digital transformation entails much more than digitising existing processes
A key part a digital transformation relates to how new attitudes and thinking are taken on and adopted. This has been evident in some sectors where disruptive innovators have improved certain aspects of production, which has stimulated adaptation among bigger players. For instance, not too long ago electronic banking was deemed revolutionary. Now the word ‘electronic’ is redundant.
Typically, small-scale disruption is evaluated, adopted and scaled to improve performance across a sector. A related feature, decoupling, is another hallmark of a digital transformation. Smaller operators are taking on specific parts of the value chain and improving these from the consumer perspective. There are some signs of decoupling in health. For example, pre-diabetic care, mental health or radiology services are beginning to be outsourced by established actors such as hospital chains, insurers and health systems to smaller organisations dedicated to more narrow function (Shah, Farkas and Kocher, 2019[14]). GP at Hand, a digital service in the United Kingdom providing health advice, triage and remote GP consultations, was launched in 2017 in partnership with a west London primary care practice. The number of patients enrolled with this service rose from 4 700 to over 50 000 within two years. However, the disruption caused by the digital service is challenging the prevailing order and its institutions (Burki, 2019[15]).
Decoupling may seem ill-suited to health. After all, it conflicts with the rhetoric of service integration (which is often implied to suggest vertical integration). However, disruption need not mean fragmentation. It may actually have the opposite effect if innovation is underpinned by a coherent information infrastructure and policy framework. The urgent need for these is a key finding of this report.
The health sector has unique characteristics. For example, some health data are very privacy-sensitive. They can also be complex. But this does not fully explain the lack of progress. Other types of data, financial or social security, are also considered sensitive. Data mining techniques to analyse complex, unstructured data are available. Complexity is also not inherent. A hallmark of digital transformation is efficient data exchange. This is made possible with adoption of common standards and protocols. The global internet protocol (IP), which enables the seamless exchange of data across the internet, is perhaps the pre-eminent example of this. Yet harmonisation is still largely lacking in health, making health data more complex than it needs to be.
The lack of a common approach is partly responsible for a health data ‘gold rush’. Commercial organisations are profiting from acquiring, harmonising and selling large volumes of personal health data for a variety of commercial purposes (IQVIA, 2019[16]; Forbes, 2018[17]; Fortune, 2016[18]; Computer World, 2019[19]; Healthcare Weekly, 2019[20]). While the commodification of these data is not inherently negative, it does raise a number of questions regarding privacy, consent and efficiency that require a policy response.4 Regulators and policy makers need to prevent the misuse of personal health data, as well as ensuring that the benefits of their use are distributed equitably. After all, most gold rushes did not end well for the majority of those involved.
Despite the uniqueness of health as a sector, the key lesson from other sectors resonates: that digital transformations are not achieved by simply digitising existing practices. In fact, 45% of companies report that ‘digitisation’ fails to deliver the expected returns (McKinsey, 2019[21]). Success depends on deeper institutional change. And while the transformation has certainly entailed disturbance to the established order, has made some actors in the global digital economy wealthy, and has had certain negative social consequences, there is little doubt that it has also generated sizable consumer surpluses and welfare (Brynjolfsson, Eggers and Gannamaneni, 2018[22]). In net terms, the principal beneficiaries have been the public.
1.2.2. Lessons from other sectors are relevant in health
Why has health – a sector where information and knowledge are critical to performance and success – been so slow deploy available technology for better information and knowledge?
Inputs are not the reason. The data exist, ready to be exploited. The technologies to extract, manage, transmit and analyse them are also available and are continuously improving. Investment in AI is accelerating worldwide as is the number of registered AI patents (OECD, 2019[1]). The number and proportion of scientific papers using data mining and big data5 analytics is rising (Galetsi, Katsaliaki and Kumar, 2019[23]). The expertise to put data to work exists – albeit residing mostly in other sectors.
The reasons relate to the very things other sectors have been able to address: the organisational and institutional capacity to harness these inputs. The key enablers – flexibility, re-structuring and working across silos – are anathema to the fundamental way in which health systems are organised. Their institutions, forged in the pre-digital era when it was not possible to combine, share and analyse large amounts of data, are known for being static and resistant to change. In many ways, the arrival of digital technology has simply highlighted these long-standing barriers to achieving health policy objectives.
A digital transformation must begin with an explicit recognition that data are a valuable resource, but have no intrinsic value unless put to work within an enabling institutional environment. This recognition, which in many cases finds expression in strategic orientation (an important element of policy making), must be pan-sectoral in order to begin bridging the silos that impede digital transformation. Digital strategies abound in health, but whole-of-government approaches on which enabling policy frameworks can be built are rare.
Flexibility is another defining feature of any transformation. This means allowing existing actors and new entrants to disrupt thinking and practice. It also means allowing smaller parts of larger organisations to trial new approaches, which are then evaluated and, if viable, scaled up for broader adoption and until the new practice becomes the new normal across entire sectors – as was the case with e-banking.
Health, of course, is not an area where the fail early, fail often mantra holds the same appeal as in Silicon Valley. Nevertheless, a number of examples exist of how innovation is not just possible but can advance health policy objectives. The challenge is to permit some flexibility and controlled disruption, while managing risks. This is eminently possible even in complex, risk laden endeavours. Aviation, for example, has already been mentioned. The British Army has overhauled its operational model, enabling its forces to become more modular and agile (McKinsey, 2019[24]). But in order to work, innovation must be underpinned by common protocols, standards and an integrated information infrastructure. This hinges on appropriate governance designed specifically to maximise the opportunities and minimise the new, unique risks of the digital era.
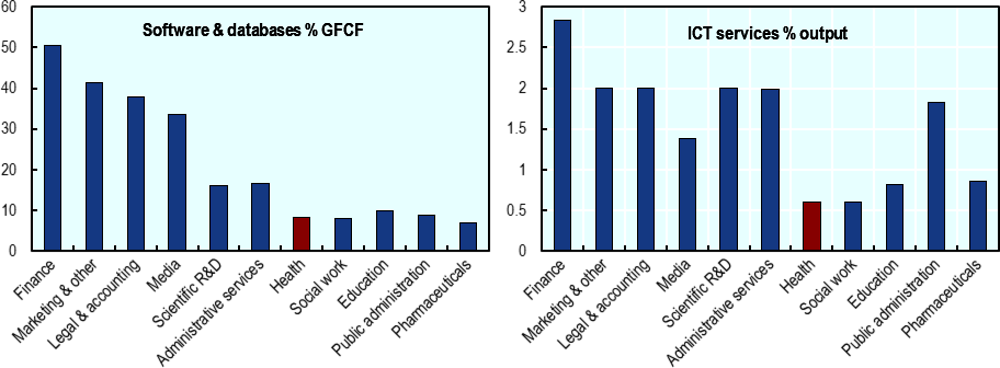
Capacity to use digital technology, manage data and extract knowledge from them must exist. This requires investment in not just hardware but the expertise to make the most from it. It must target the supply side and the demand side. Providers and patients need to be engaged. Surprisingly, OECD countries typically invest only under 5% of health budgets on managing information. In other sectors investment is four times higher (OECD/WHO/World Bank Group, 2018[25]). Closer inspection reveals that the health spends similar amounts to comparable sectors on tangible products such as ICT hardware, computers and network infrastructure (Calvino et al., 2018[26]). However, spending on intangible products such as software and databases, and the purchases of ICT services is comparatively modest (Figure 1.1).
Lifting productivity and creating value through process innovation
Data-driven technologies are general-purpose, meaning that they can be deployed in almost any aspect of any human endeavour. Their inherent characteristics (low marginal costs, non-rivalrous nature, network effects) provide the means to fundamentally change production functions, thus improving productivity in unforeseen ways (Brynjolfsson, Rock and Syverson, 2019[27]). For instance, not many could have predicted how the internet would transform the global economy. While digital technology has spawned a handful of completely new human activities, its value has overwhelmingly manifested in making routine, existing activities and processes more efficient, more convenient, more productive and cheaper.
Seen in this fashion, a digital transformation has the potential to address Baumol’s cost disease – the inflationary effects on expenditure experienced in labour-intensive sectors such as health (Baumol, 1967[28]). This need not necessarily be achieved through automation of labour alone. Rather, digital technology, deployed intelligently, can improve just about every facet of production in a health system on both the supply and demand side: service providers become more efficient in producing and delivering services, while consumers become more savvy and competent at using them. As was the case in previous industrial revolutions, this often involves complementing human labour with that of machines.
In health, the potential economic benefits of data- and digitally-driven process innovation are abundantly clear. This is a sector that consumes a tenth of national incomes (a figure that is also rising), where approximately 20% of expenditure does not generate health benefit, and where technological progress tends to increase prices and spending (OECD, 2017[29]; OECD, 2017[12]). Investing in a digital transformation is therefore a very attractive proposition (see Section 1.5.4). Rather than creating new things to do, data and digital technology can make existing health system processes and activities more productive and efficient.
The term ‘existing processes and activities’ may appear to exclude new treatments and therapies – a pivotal aspect of the health sector both in terms of value as well as expenditure growth. However, it includes the process of finding innovative new treatments, as well as their regulation, pricing and integration into service provision. All of these activities can be greatly improved by using existing data and digital technology.6 The combined improvement of these and other processes may be instrumental in tackling Baumol’s inflationary effects in the health sector.
But risks and potential pitfalls must be actively managed
It is not suggested the exact processes and behaviours of other sectors should simply be replicated in health. Some, such as excessive hype and overinflated expectations, are best avoided. For example, replacing conventional cars with safe, automated vehicles has been more difficult than expected despite promises by the technology and automotive sectors (The Economist, 2019[30]). The complexity of human-designed systems is often underestimated. The obstacles, however, have been technological as well as ethical and legal. A parallel with the health sector are predictions that health professionals will be replaced by algorithms fed on Big Data. It is best to temper such forecasts with solid analysis.7
Perhaps more concerning is evidence – explored in this chapter and in this report – that the benefits of digital technology accrue unevenly across socio-economic and demographic strata. While a digital transformation delivers a net consumer dividend, it can favour the already more well off while others are left behind (OECD, 2019[1]). Given that equity is a key health policy objective, policy makers must actively manage and avoid the perpetuation of disadvantage and inequality.
In the end, a digital transformation in health is not be an end in itself. It is a means to achieving a set of agreed public policy objectives more effectively and efficiently. Data and digital technology can provide the tools but will not achieve much on their own. Caution, prudence and oversight are always advised. Policy makers should take care to avoid the pitfalls and minimise unintended consequences of specific aspects of digital technology. But the fundamental socio-technical enablers that underpinned transformation in other sectors can and should be deployed to guide a similar transformation in health.
copy the linklink copied!1.3. Despite rising digitalisation, health systems remain ‘data rich but information poor’
Using data and digital technologies intelligently harbours a number of opportunities to improve health and health policy outcomes in a number of areas. For example:
-
empowering people to take greater control of their health and communicate with their health care team;
-
enabling health care providers to have access to consistent and timely information about their patients to promote appropriate and coordinated care;
-
Identifying at-risk and complex population groups more accurately, and targeting delivery of appropriate treatments and integrated, people-centred care;
-
using existing data ranging from electronic medical records to insurance claims to assess and compare the performance of biomedical technology and treatments;
-
extracting information on health system performance to identify waste, inappropriate practice and inefficiency, and improve policy making, system governance and stewardship, including better funding and remuneration;
-
harnessing Big Data from within and outside of the health system to improve public health policies and interventions, and prevent the occurrence of disease more effectively as well as enabling effective responses to public health emergencies.
This section briefly describes these opportunities as well as how OECD countries are faring in turning these opportunities into outcomes. It also outlines the critical role of health workforce in a digital transformation. Countries are beginning to recognise and act, but more coherent and proactive policy responses are needed.
1.3.1. The right information to the right people at the right time
The failure to extract and use information contained in health data, which exist already, is a significant missed opportunity to improve services and care. For example, 10% of patients are unnecessarily harmed during care. The health burden of this in OECD countries is on par with diseases such as multiple sclerosis and some cancers. The direct financial impact is as high as 15% of hospital expenditure, and the broader economic drag estimated to be in the trillions of dollars (Slawomirski, Auraaen and Klazinga, 2017[31]). The most common root cause is a failure of communication – information and knowledge not reaching the right person at the right time. Shared electronic information platforms have been shown to improve safety by addressing the communication problem (Banger and Graber, 2015[32]).
Better information exchange makes care not only safer but also more effective and efficient. Care can be better coordinated by different providers and integrated with other services, with better results and less duplication and waste (OECD, 2017[29]). This is especially important for the growing number of people who have multiple chronic conditions, currently estimated to represent at least 20% to 30% of the adult population in OECD countries. For these individuals, accessing care can be frustrating, inefficient and costly in a system fragmented across sectors and disease groupings.
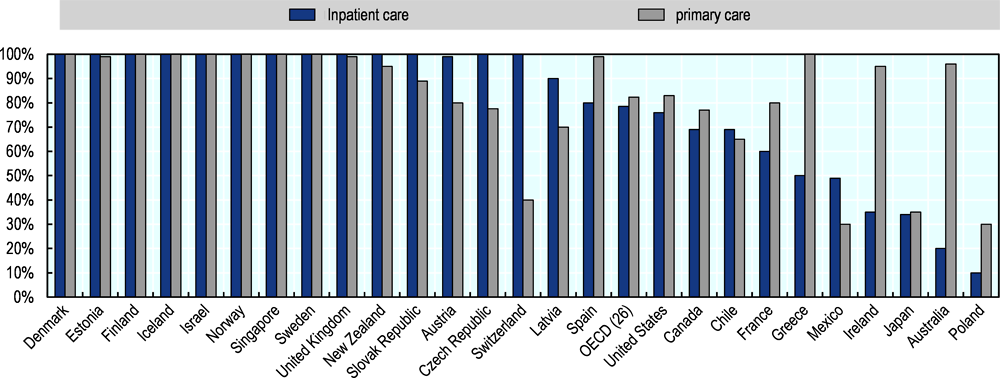
Enabling access to the electronic health or medical record (EHR or EMR)8 by all actors involved in a patient’s care is a key structural component of a high-quality health system (Auraaen, Slawomirski and Klazinga, 2018[33]). While most OECD countries are well on the way to digitalising their health services through the introduction of electronic records in physician practices, hospitals and other settings (Figure 1.2), only 64% of countries report that these form part of an integrated network where secure but unencumbered exchange of information is possible (Oderkirk, 2017[34]).
This can mean either a ‘one patient one record’ approach or one made up of disparate platforms that are set up to exchange data and information. A patchwork of electronic records that cannot efficiently link or exchange information with one another is not effective in improving safety or other aspects of care quality such as co-ordination, efficiency and a positive patient experience. From a systems viewpoint it is not much better that the pre-digital equivalent of paper records stored in individual health care organisations.
Enabling people to access their health records and interact with their own medical information is a driver of high quality people-centred care. Digital technology provides the ideal platform to enable this access easily and efficiently. It is encouraging that approximately 70% of responding countries to the 2016 OECD survey reported that people can access their record. However, only 43% reported that individuals could interact with their own record (e.g. enter information, send requests, communicate with providers). A study by Barbabella et al. (2017[35]) found that the majority of hospitals in Europe (90%) do not permit patients to access their own health data. Elsewhere, access restrictions can sometimes result from legislation. For example, United States federal and state laws allow patients to request amendment to their health record but not to directly interact with their record.
People’s rights to access their health records may also be underused. In the United Kingdom, fewer than 8% of patients who were able to access their medical records actually did so (NHS Digital, 2019[36]). In programmes to improve care for multi-morbid patients, tools for sharing of information mainly focus on interactions between professionals and provider organisations, not on making information available to patients (Melchiorre et al., 2018[37]). Access is likely even lower among populations with complex needs. In the Netherlands, for example, just 4% of the chronically ill population reported using a personal health record.
Examples of progress can be found. Estonia has a unified EHR, which enables residents to view all of their medical data in one place – including diagnoses, test results, medications. Residents can also interact with their data. For example, they can update their details, supplement existing information, and carry out administrative processes such as obtaining a medical certificate for a driver’s license without needing a specific appointment. Lithuania (which did not respond to the survey on which Figure 1.2 is based) has implemented a centralised ‘one resident – one record’ EHR system that covers 95% of the population. It carries all relevant medical information in integrated electronic workflows covering appointments, referrals and e-prescribing. It also enables provider interaction and patients have secure access to their record through a patient portal.9
1.3.2. Data can help identify health need and target care more accurately
Analysis of existing health data can enable health service planners and policy makers to identify and target individuals who have complex health needs. These people may not always be in contact with the most appropriate health care providers, making data a valuable resource for creating information on where they reside, their level of need, the type of services they will require and the level of resourcing required.
In Spain, a locally developed risk-stratification tool is used in 14 of the country’s 17 autonomous regions. EMR data from primary care providers and hospitals across the regions are linked to create a common data pool. The model uses this pool to identify complex patients based on a classification termed morbidity adjusted groupings (Grupos de Morbilidad Ajustados – GMAs). The system supports targeting of care and helps allocate resources according to health need. One limitation is that the GMAs do not capture variables that are not coded in clinical data such as social and economic circumstances, which could be included with linkage of additional data sets.
Many of the Spanish regions have built on this tool to develop integrated care models for complex patients identified. These often use shared electronic care plans to plan and monitor the care patients receive from various providers, relying on a shared EHR to exchange information with a single provider taking on a coordination role. Such models harness shared information systems while alleviating overburdened providers, for instance by reducing unnecessary hospitalisations and the administrative workload of primary care doctors.10
The United States Office of the National Coordinator for Health IT (ONC) released Draft 2 of the Trusted Exchange Framework and Common Agreement (TEFCA) in April 2019. This outlines a common set of principles, terms, and conditions to support nationwide exchange of electronic health data across disparate networks. The TEFCA is designed to scale health data exchange nationwide and help ensure that Health Insurance Networks, health care providers, health plans, individuals, and other stakeholders have secure access to their electronic health information when and where it is needed to promote care co-ordination and orientate care around patients’ needs.
While some promising examples such as these can be found, there remains a lot more that can be done in this important area of using existing data for the important purpose of identifying and addressing health need.
1.3.3. Most OECD countries are slow to harness data for safer and better treatments
The potential of using data to generate information and knowledge extends beyond improving patient care. Another important area is the assessment and regulation of medical technologies.
Real-world data (RWD) refers to data created during routine health system activity, as opposed to data generated during clinical trials. RWD can be used to generate evidence on how drugs and other medical products perform in routine clinical use. This can complement evidence derived from clinical trials to better inform decisions and actions of clinicians, patients and policy makers.
It also represents value for money. Clinical trials are complex, lengthy and expensive, yet typically include a relatively small number of carefully selected subjects, who may not represent the patients that the product will eventually be used on. Modern analytical techniques drawing on large sets of RWD can include millions of subjects. The statistical power is comparably large, and advanced methods to limit confounding variables continue to evolve. Real-world trials can now reproduce trial results much faster and at a fraction of the cost (Fralick et al., 2018[38])].
This can deliver faster, safer and better treatments – particularly for emerging health challenges such as dementia and chronic conditions, where pooling relevant data from a range of sources is the only way of devising timely detection and effective therapies.
It can also inform better policy. For example, as evidence of a product’s performance accumulates, payers can determine if prices reflect therapeutic benefit – and adjust them accordingly. This can not only improve efficiency and value derived from medical technologies, but also sets incentive signals for future product development.
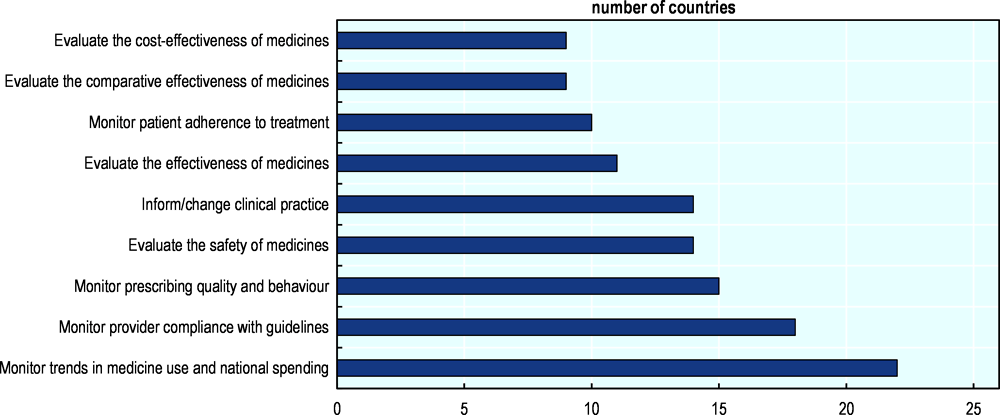
However, most health systems are not harnessing data to their full potential in this way. The majority of twenty-six OECD and European Union countries surveyed in 2018 on the use of routinely collected data reported that the principal purpose was to monitor medicine consumption and expenditure (22 countries). Eighteen used these data to monitor provider compliance and 15 to monitor quality of prescribing. Meanwhile, 14 countries reported using routine data to evaluate the safety of medicines (Figure 1.3).
The positive finding is that at least routine data are beginning to be used. However, in most cases the data excluded drugs dispensed in hospitals, which represents a considerable proportion of medicine consumption. This suggests problems with data linkage and information infrastructure. Moreover, only nine countries reported that evidence generated from routine data was considered by health technology assessment agencies (HTA) in their decision-making (OECD, 2019[39]).
Overall, the majority (19) of responding countries answered ‘no’ to the question of whether routine data were used to their full potential. The main barriers cited were prohibitive privacy legislation and poor data quality (governance issues) and lack of capacity in terms of infrastructure as well as analytical expertise (OECD, 2019[39]).
Perhaps the best example of systematic use of routine data at a national level is the United States Food and Drug Administration’s (FDA) ‘Sentinel’ Initiative. The Sentinel programme monitors the safety of medical products in routine use by accessing personal health data – scattered across a large number of health care organisations, payers, dispensers and other agencies – of over 200 million people. To ensure security and privacy, data never leave their location. Instead, single electronic queries are sent across the entire network. This feature is enabled by common data standards and protocols. Identifying safety problems the old way used to take years. Sentinel does this in weeks or months, reducing harm while saving money and time. Since its establishment in 2014, the initiative has enabled important regulatory decisions. It is also eliminating the need for many expensive post-marketing studies, which can cost millions of dollars to run.11
1.3.4. Big data are not used to their full potential in public health
Public health is arguably the area where data – especially ‘big data’ flowing from non-traditional sources outside of the health system such as social media, web searches and environmental data – can be put to work to advance health and prevent disease. These data can complement traditional information sources to answer many questions and steer public health policy in three key ways:
-
1. Allowing a more precise identification of at-risk population groups (‘precision public health’);
-
2. Enabling better surveillance of both communicable and non-communicable diseases;
-
3. Facilitating better targeted strategies and interventions to improve health promotion and disease prevention.12
These new methods can be used to tackle a range of public health priorities, such as monitoring and responding to food-borne outbreaks, identifying behavioural risk patterns across populations, or monitoring signs of mental ill-health such as suicidal ideation.
Much promising activity is already happening at the municipal level. “Smart Cities” demonstrate how integrating transportation, mobility, food safety and environmental data can contribute to more effective and efficient health promotion and disease prevention. For example, the city of Chicago used publicly available data from a variety of sources (ZIP codes, business licenses, building code violations, and a phone hotline for complaints) to predict restaurants most likely to be in violation of health codes. More recently, researchers used anonymised Google search terms and geolocation data of individual users to identify food-borne disease outbreaks across the city. Problems were identified considerably faster and more accurately than with traditional surveillance methods.
At the national level, Korea is in the process of integrating the national health insurance database (NHID) with clinical records, health care activities as well as data from outside of the health system including climate, pollution and geolocation data. To date, analytical uses of the NHID have included, for example, identifying causality and predicting risk by linking health-screening data with medical history and socioeconomic status, and a surveillance system to target chronic diseases, based on information of individuals’ use of health services. The amalgamation will further equip decision makers, public health experts and citizens with more detailed information to pursue a range of efforts to improve public health and prevent disease.
Some countries have also started exploring the possibility of using genetic data to inform public health prevention. In Estonia, two large-scale clinical trials are working to better target preventive health care services at patients at higher risk of cardiovascular disease or breast cancer, based on genomic algorithms using data from the Estonian Genomic Center. In the United States, a USD 215 million Precision Medicine Initiative was launched in 2016. This will include, among other projects, the All of Us research programme, a 1-million participant study whose mission is “to accelerate health research and medical breakthroughs, enabling individualized prevention, treatment, and care” by studying “individual differences in lifestyle, environment, and biology”.
Big data present a number of opportunities but also have some inherent limitations as well as challenges relating to inter alia ensuring their quality and managing their security and privacy implications. For example, the temptation to over-rely on big data without robust methods for interpreting it can lead to apophenia: “seeing patterns where none actually exist, simply because enormous quantities of data can offer connections that radiate in all directions” (Boyd and Crawford, 2012[40]). Approaches using big data should therefore complement – not replace – traditional public health surveillance methods. Nevertheless, big data have the potential to facilitate the more effective translation of knowledge into effective public health policy, by enabling a better understanding of the interaction between behaviour, genetics, and the physical and social environment.
Transparency represents a key element that can facilitate the success of public health initiatives based on big data. Sharing data and algorithms with other stakeholders (e.g. collaborations between academia, public health departments, industry, and citizens) enables a more effective use of data and facilitates the early detection of any problems, as well as allows other public health authorities to implement similar successful interventions. But transparency needs to be underpinned by good data governance, which ensures that security and privacy are maintained and maximises the utility and use of available data to generate valuable knowledge.
1.3.5. Harnessing data to improve efficiency and value across the health system is rare
Using available data can drive considerable improvements in how complex health systems are managed. The knowledge extracted from data can help decision makers identify and act on problems such as waste and inefficiency, and to make the decisions, and judgements needed for a health system to function. This includes setting priorities, and allocating resources across populations and competing programs.
In some health systems the proportion of unnecessary treatments, procedures and therapies exceeds 40% (O’Neill and Scheinker, 2018[41]). Identifying wasteful spending through better use of available data is a prime opportunity for improving efficiency and outcomes (OECD, 2017[29]).
For example, the Washington State Health Care Authority (WA HCA) has linked claims, billing and EHR data of 2.4 million insured individuals to examine inappropriate and wasteful practices. The algorithm classifies services as necessary, likely to be wasteful, or wasteful. The benefit of linkage across the three data sources is that it allows more nuanced analysis, incorporating the individual context of each case, as opposed to simply tallying the number of procedures on a ‘low value’ list.
Of the 1.52 million services analysed 44% were classified as wasteful (i.e. not adding any health benefit for the recipient). Spending on these services amounted to USD 282 million, or 36% of WA HCA expenditure (WHA, 2018[42]). A similar study in Saint Louis, using data of 1.6 million individuals, identified 46% of services as unnecessary (National Alliance Of Healthcare Purchaser Coalitions, 2018[43]).
Clearly some people receive unnecessary treatments while others, in greater need, miss out. In addition, unnecessary duplication and wasteful administrative processes abound in all health systems. The challenge is using this information and knowledge to develop effective policy responses to reduce these inefficiencies and redeploy resources where they are most needed.
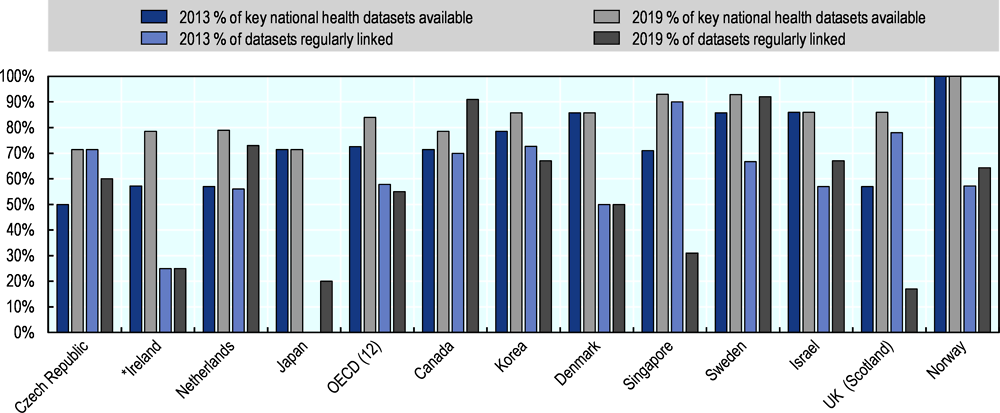
Data linkage, by shedding light on what is really going in a complex health system, is a critical step to assess performance, identify problems such as unwarranted variation, and enable smarter resource allocation. However, a survey of OECD countries conducted in 2013 and repeated in 2019 found considerable variation in both the availability and readiness of key data sets, and their regular linkage for secondary purposes such as system management (Figure 1.4). While the 2019 information is preliminary and the participation of a greater number of countries in the 2019 data collection is necessary for understanding change over time, the results suggest that key health datasets may be less likely to be regularly linked than they were in 2013.
One possible reason for the reported reduction in linkage is that the European General Data Protection Regulation (GDPR) came into force in 2018. The GDPR affords personal health the highest level of protection, and has brought security into sharper focus within the European Union and beyond, with many countries still adapting their systems to respond to the new regulation. Protecting data and putting them to work are not mutually exclusive – both can be achieved with strong data governance frameworks.
Nevertheless, linking disparate datasets to create new knowledge for policy and other purposes is eminently possible. In New Zealand, personal health and other public sector data are linked to create ‘virtual registries’ for diseases such as diabetes (Jo and Drury, 2015[46]). These registries track the health care activity and outcomes of the relevant patient population enabling better assessment, decision-making and resource allocation. Traditionally, such registries are constructed in parallel to existing data sources. This can cost millions of dollars to establish and maintain. Harvesting the data from existing data sets is much cheaper and more efficient. Similar linkage in New Zealand also enabled detailed cost-of-illness study of multi-morbidity, generating hitherto unknown knowledge on the expenditure profiles of patients with various combinations of chronic diseases (Blakely et al., 2019[47]).
Detecting fraud, a significant burden on many health systems (OECD, 2017[29]), can be enhanced with modern data analytics. The United States Department of Health and Human Services-Office of Inspector General (HHS-OIG) mines available data and applies predictive analytics and modelling to enhance oversight of the Medicare and Medicaid programs for fraud. Multi-disciplinary teams use near real time data to examine claims for known fraud patterns, identify suspected fraud trends, and to calculate ratios of allowed services as compared with national averages, as well as other assessments.13
1.3.6. Information systems can enable better health funding models
A major contributor to the problems faced by health systems is the way services are paid for. The rise of chronic diseases and longer life spans means that service delivery should be approached in a more longitudinal and coordinated way that crosses boundaries between sectors (including social care) and settings. Remunerating individual service parcels is becoming less and less conducive to ensuring effectiveness and efficiency in the majority of health care activities.
Payment systems that encourage integration and that cover entire care pathways, better outcomes and efficiency have been discussed for some time. Alternative models to meet the challenges of rising patient complexity and achieve policy objectives include: additional payments made before during or after service delivery for specified outputs or outcomes; bundling – a combined, single payment for entire care cycles across settings and including primary and tertiary care, imaging and pathology, rehabilitation and follow-up care; and population-based payment, in which groups of health providers receive payments on the basis of the population covered, in order to provide most appropriate health care services for that population (OECD, 2016[48]).
While these non-traditional payment models vary in their design, incentives and structure, they have one thing in common: their success relies heavily on an information system with the capacity to integrate data on inputs, outputs, processes and outcomes. This was difficult in the analogue era – part of the reason that fragmented payments such as fee-for-service became the dominant model. However, electronic linkage of clinical, administrative, financial and other data makes these new approaches possible. Payments can be bundled across a set of providers and activities, with data systems ensuring that each component is remunerated appropriately. The clinical and budgetary consequences of a medical error at any point in the pathway become the responsibility of the entire team of providers, as opposed to the ones downstream to where the problem occurred. This encourages better coordination and communication (the lack of which is the most common cause of adverse events). Good information systems can ensure that payment for achieving agreed performance metrics is based on reliable data from several sources that can be more accurately adjusted for patient complexity and other confounders. Technologies such as blockchain, which can enable deployment of ‘smart contracts’, can further enhance the reliability of these payment models.
Similarly, population-based remuneration can also be adjusted to reflect health need, making it possible to transform care. The possibilities for these innovative approaches to payment expand when health data can be linked with social care data. Enabling payment models that encompass a broader range of health determinants could yield better health outcomes than the current fragmented approach. Integrating data in this way increases the accountability of each provider who contributes to a patient’s care pathway.
While the possibilities are many, examples are few, especially at the national level. Partners HealthCare in the United States has implemented a bundled payment framework that encompasses acute and post-acute care providers. The framework comprises four parts: risk stratification of patients, care team convening and planning, monitoring and communication, and patient engagement. The cornerstone of this model is an integrated EMR that enables communication between providers and patients, and that supplies the data for risk stratification and eventually payment. But implementation was heavily reliant on organisational leadership and policy (Safavi, Bates and Chaguturu, 2019[49]).
Some countries are laying the foundations for new payment and resourcing mechanisms. Finland, for example, is establishing a one-stop shop for all secondary use of health and social care data, enabling a wider set of information to be integrated for use by the health system. The integration of data from all providers of health and social services, as well as socio-economic data, is intended to inform the needs-based allocation of resources across the country’s regions.14
However, data infrastructure and digital technology merely provides the possibility for changing the way providers are paid. Institutional and policy changes are needed to adapt remuneration towards a model more suited to modern demands (See Section 1.4.5).
1.3.7. Preparing the health workforce to make the most from a digital transformation is a challenge
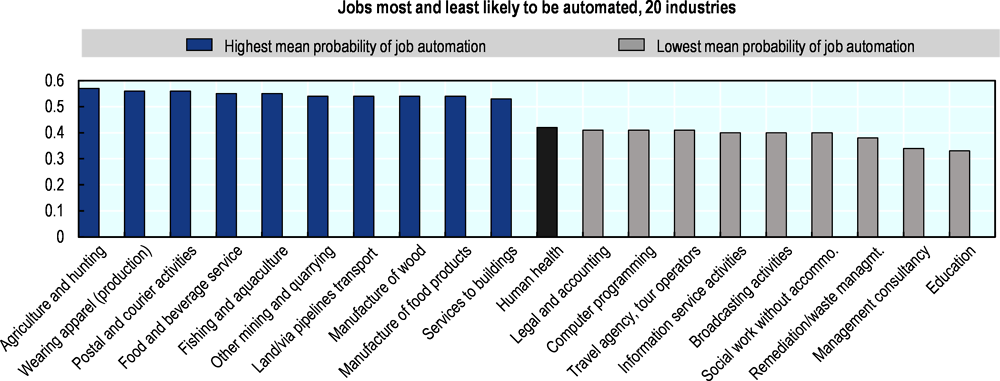
The health workforce is pivotal in a successful digital transformation. OECD analysis suggest that automation will create significant workforce disruption in modern economies. But the perception that health workers will be replaced by machines is not supported by the evidence, with their roles and tasks among the least likely to be affected (Figure 1.5). Nevertheless, majority of health workers are likely to see changes in their task composition towards tasks that are difficult to automate, such as those related to creative and social intelligence, teamwork and other ‘soft’ skills.
As discussed, digital technology offers opportunities to improve care delivery. Data-driven tools can support health workers in performing tasks that are repetitive, time-consuming, and heavy on data processing, such as selecting irregular results from large volumes of preventive or routine chronic care tests, synthesising information relevant for a given patient’s condition from numerous sources (patient records, archives, guidelines, specialist recommendations), or analysing patterns in patient outcomes for regular improvements in practice.
Machines are also beginning to match human performance and accuracy in, for example, analysing radiological images and retinal scans. Workers aided by these tools could become more productive. This includes having greater opportunities for face time with patients or colleagues, and to employ human skills to address their professional obligations more effectively and with requisite empathy.
Leveraging data to improve clinical as well as other activities of health care systems also means that new occupations – and roles within existing occupations – are likely to emerge. For example, oncologists, radiologists and anaesthesiologists could work with coders and data scientists to design, evaluate and refine the algorithms that enhance their practice.
However, things are not as simple as feeding reams of data into a machine – as the aforementioned problems with of autonomous vehicles suggest (Section 1.2.1). In the health space, difficulties with initiatives such as IBM ‘Watson’ suggest that the automation of complex and nuanced clinical decision-making is more complex than initially thought. Watson was trained to give treatment advice for cancer patients, but frequently made unsafe recommendations. A key problem was that Watson was trained on hypothetical, not real-world data, highlighting the importance of strong data governance to enable putting real-world data to work for productive purposes.
Nevertheless, the fact remains that health workforces are ill-prepared for a digital transformation, which makes change harder and slower. For example:
-
Requirements to undertake continuous professional development have not kept up with technological and labour markets changes affecting the economy as a whole. Up to 70% of health professionals report not being accustomed to using digital solutions due to gaps in knowledge and skills in data analytics (Hegney et al., 2007[51]; Foster and Bryce, 2009[52]; Skills for Health, 2012[53]; European Commission, 2013[54]; European Health Parliament, 2016[55]; Quaglio et al., 2016[56]; Melchiorre et al., 2018[37]). A health professional who does not understand how an algorithm behind a clinical decision support tool was developed, or the data used for its conclusion, will see it as a “black box” and may be reluctant to use it (Galetsi, Katsaliaki and Kumar, 2019[23]).
-
A fragmented, disease-centred approach to health care delivery means that many digital solutions are not fully deployed because of limited teamwork among health workers belonging to different professional categories, specialties, or provider organisations (Rudin et al., 2016[57]).
-
Tasks in health care are defined based on the type of employment. For example, only doctors can perform certain tasks. This limits the opportunity to leverage digitalisation to improve efficiency and address shortages by facilitating shifting of tasks from doctors to nurses and community health workers.
-
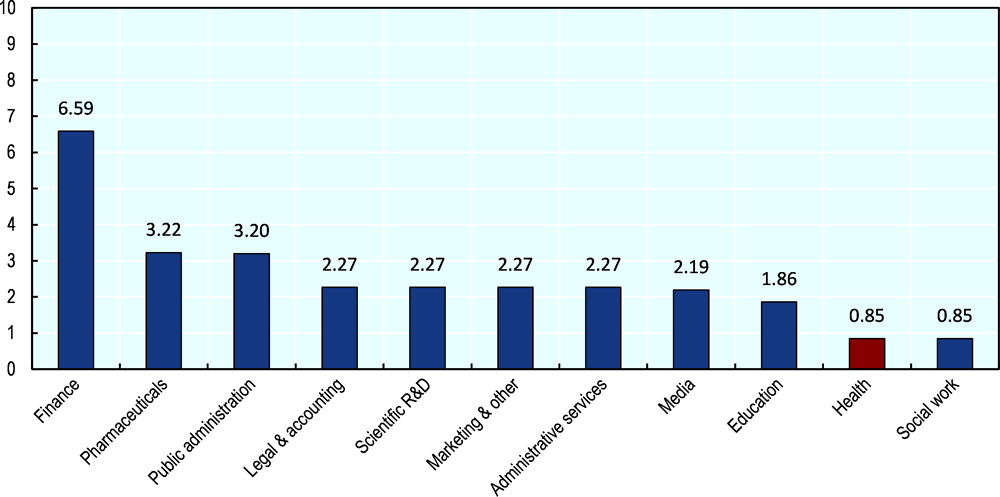
In-house expertise to put data to work is also missing. Making the most of digital opportunities and ensuring that the changes result in favourable outcomes requires ICT specialists and data scientists. Sector-specific specialisation for these occupations is becoming increasingly common and valued. Yet, recent OECD analysis suggests that the health sector has relatively few specialists (less than 1% of employees) in these fields compared to education, public administration and finance (Figure 1.6).
Some health systems are addressing these issues, particularly in terms of improving digital literacy among their health workers. Australia, Canada, Norway, Switzerland, New Zealand, and the United Kingdom completed a review or established a regular process to assess how technological and other developments (including ICT, AI, genomics, or demographics) are likely to change the skill requirements and the roles and functions of health workers over the next two decades. These reviews include the consequences for the education of future, and the training of current health workers.
Based on such a review, the Norwegian government, for example, is currently restructuring national curriculum regulations in health to make these more future-oriented. In Switzerland, eHealth Swiss has published guidelines for educators on how to integrate digital-health topics into the education and professional training of health workers. Canada Health Infoway – an independent, not-for-profit organisation, fully funded by the federal government – supports the Digital Health FACTS programme, which engages inter-professional faculty and students of medicine, nursing, and pharmacy to promote and scale up development of digital skills that match the demands posed by the emerging digital technologies.
Many countries have developed new programmes and accreditation standards in Clinical Informatics, with some – the United Kingdom and the United States, for example – creating hybrid degrees that closely tie clinical leadership with informatics and digital transformation. These hybrid programmes allow clinical leaders to obtain new competencies in ICT-based quality improvement and change management to provide the needed leadership and ensure buy-in from health workers in general. In the United States, the HITECH Act funded two distinct health IT workforce training programs, which have trained 21 437 students and working professionals.15
However, more is required to ensure that the skills health workers (and the health workforce) needed for effective and safe use of emerging digital tools, technologies and data analytics are taught routinely. The same goes for human capital in administration, management and policy making, where digital, data and statistical literacy are equally crucial to drive positive transformation. With the current accelerated pace of technological development, it will become more necessary for health workers to regularly update their skills. As such, it is important to reconsider the skills delivery pathway, and encourage a shift towards a lifelong learning model. But concrete strategies for achieving this are still to be formulated in most countries.
copy the linklink copied!1.4. Tackling the barriers to a digital transformation needs an overhaul of policies and institutions
Failing to implement and harness a digital transformation is a missed opportunity for better care, more effective treatments and improved health system performance. The lack of progress pints to significant barriers. But these are not technological. The data and technology are, in the main, sufficient. The barriers are structural, organisational and institutional. They have been in place since long before digital technology made it possible to generate, transmit and analyse large amounts of data easily. They include fragmentation and silo thinking – a renowned, persistent and frustrating characteristic of health systems.
These barriers are habituated and firmly baked into how health systems function. They are difficult to change without a fundamental overhaul. Addressing them requires changes and adaptation on a number of fronts. The most critical are outlined in this section. They include changing professional attitudes and skills, updating ethical frameworks, engaging health system users, opening data availability and facilitating their integration, and an environment that creates incentives and behaviour for a transformation to take hold.
1.4.1. Transforming skills and attitudes across the sector
Using data (and to a lesser extent digital technology) is still too often seen through a lens of risk as opposed to opportunity. This is an outdated, 20th century view, but is reflected in existing policies that make it very difficult to put data to work. Too often use of data is seen principally as a risk to privacy, cybersecurity threats and the costs of security breaches (including liability).
While data security and privacy are crucial, forward-thinking countries and health systems equally recognise and communicate the opportunities of using data. In contrast to previous decades, the 21st century approach is to maximise the benefits while minimising the risks. Both are possible but only with strong, fit-for-purpose governance and policy frameworks.
Paternalistic attitudes that tend to prevail in health sector are also not conducive to promoting the use of data and information for purposes ranging from empowering people to take greater control of their health or effective sharing of data across specialties and settings of care. Beyond care delivery, this presents a barrier to secondary uses of data for research, public health and performance monitoring.
The way in which digital tools are developed serves to illustrate why this is a problem. For example, few health apps are designed with involvement of the end user – the individual with a particular health need or the health professional. Often, there is little input from clinical experts. More typically, digital tools and gadgets are developed by IT experts. Another example are EHRs, which are often developed and designed with a purpose other than making clinical care more effective and efficient. The technology ends up ‘getting in the way’ of not only delivering good services but also of generating high quality data that can then be used for other important purposes.
A fundamental part of addressing this revolves around equipping the entire health workforce with the skills and attitudes to make the most of data-driven technologies. For example by reforming both initial training and continued professional education and supporting health workers in acquiring new digital and teamwork skills. It concerns how health workers are socialised and taught to interact with colleagues in their as well as other professions and their patients. It also requires ensuring that individuals and patients feel empowered to work in partnership with their care providers (see Section 1.4.3).
As discussed, most countries are still at the preparatory stage of restructuring of health workers’ curricula to respond to the demand for updating of skills. Similarly, courses and teaching methods such as inter-professional education that aim at reinforcing skills related to teamwork and inter-professional collaboration are not yet routinely included in the core curricula. Only some countries – Canada, for example – have built in these skills explicitly into their core competency frameworks informing health professional education. The need for strengthening the skills of health workers to work with (as opposed to around) patients, such as skills in effective person-centred communication and shared decision-making, is also usually marginalised in education and training (OECD, 2018[58]).
Other opportunities include facilitating the integration of new professions and roles in health systems and relaxing rules around the division of work between health professionals, in light of the reorganisation of tasks that digitalisation can offer at all levels of the health system. More than half of the OECD countries have made progress in this direction by expanding the roles of nurses and allowing task shifting from physicians (and nurse practitioners) to nurses (and nurse assistants) (Maier, Aiken and Busse, 2017[59]) and by creating new medical specialists such as Clinical Information Officers.
1.4.2. New ethical frameworks are needed
At the new digital frontier, a growing number of health care activities will be performed by humans together with machines. How do health workers answer questions about collaborating with AI? Even relatively simple machine-learning models already used – such as those automatically stratifying patients into at-risk and intervention groups – give rise to questions regarding health workers’ and machines’ respective roles, accountability, and about how to ensure that digital systems do not crowd out the personal touch between patients and providers.
Other questions concern how to inform a patient when a risk-prediction model did not recommend treatment, what mechanism exists to override the model’s recommendation if necessary or, again, what happens if the model’s recommendation leads to a suboptimal outcome.
No progress will be made unless professional and ethical frameworks are updated. The 2019 OECD Recommendation on Artificial Intelligence can guide countries in this regard. The recommendation comprises two sections. The first outlines the principles for responsible stewardship of AI (inclusivity, sustainability, human-centric values, transparency, security, safety and accountability). The second lays out the policy requirements for trustworthy AI (investment, a digital ecosystem, an enabling policy environment, building human capital and preparing for labour market transformation, and international co-operation) (OECD, 2019[60]). Further delay will make health professionals hesitant to use data-enabled tools and other technologies that enhance cooperation among providers across settings.
The novelty and complexity of big data analytics raises a new set of ethics-related challenges for researchers, regulators and policy makers (Ienca et al., 2018[61]). Growing possibility to use non-traditional data sources such as social media are also challenging the existing ethical frameworks, especially when these data are used for purposes that benefit public health, such as disease surveillance and outbreak management. Work is needed by researchers, ethicists and policy makers to develop acceptable decision making frameworks. For example, Vayena et al. (2015[62]) established three categories for the ethical use of personal data in public health: 1. Context sensitivity (e.g. commercial versus public health use); 2. The nexus of ethics and methods (e.g. robustness of algorithms and data provenance); and 3. Legitimacy requirements (e.g. pest practice, regulatory bodies, public communication).
Data ownership is another related area requiring ongoing discussion (Koskinen and Kimppa, 2016[63]). Here, two challenges are emerging. First, the commodification of health data, with commercial entities acquiring and on-selling personal data for commercial purposes. While these data are typically, but not always, de-identified this still raises questions about consent, ownership and about who should profit from the knowledge extracted from them. Evidence suggests that the public are reticent about their data being used for commercial purposes. Yet a considerable part of health system activity could be deemed commercial and certainly has a commercial component. Excluding companies with the expertise and resources from using health data to, for example, develop improved diagnostic tools or precision therapies that maximise clinical effectiveness and minimise risk, may inhibit potential advances to human health and welfare.
Second is the opinion that individuals are the sole ‘owners’ of their data. In a world where these data could theoretically be re-deployed in an infinite number of ways, this becomes an important issue and a technical as well as policy challenge. Ownership can be debated based on who paid for the activities that generate the data (Koskinen, Kainu and Kimppa, 2016[64]). If paid for by a third party (typically the taxpayer or insurance plan enrolees) data may be considered a public good with the payers as well as the data subjects potentially entitled to a say in how the data are used (Rodwin, 2009[65]). These and other questions become even more challenging when genomic data are considered.
Even where personal health data are voluntarily sold by the data subject, this emerging market needs to be examined through the lens of ethics and policy. People should have the opportunity to sell their data. But the likelihood that these people would overwhelmingly be from the poorer and more vulnerable social strata, and the consequent risk of exploitation needs to be considered. For similar reasons, the World Health Organisation advises against paid organ donation (World Health Assembly, 2004[66]). In addition, the potential bias in the data could affect the findings of research and other outputs they are used for.
Clues on where societies stand on these issues can be found in regulatory frameworks such as the GDPR, which recognises the societal benefits that can be derived from health data (and puts these data in a special category). But this is a fast-moving field and these questions require deeper, ongoing discussion and the development of dedicated, clearly articulated ethical frameworks and charters.
1.4.3. Engaging patients while ensuring that no one is left behind
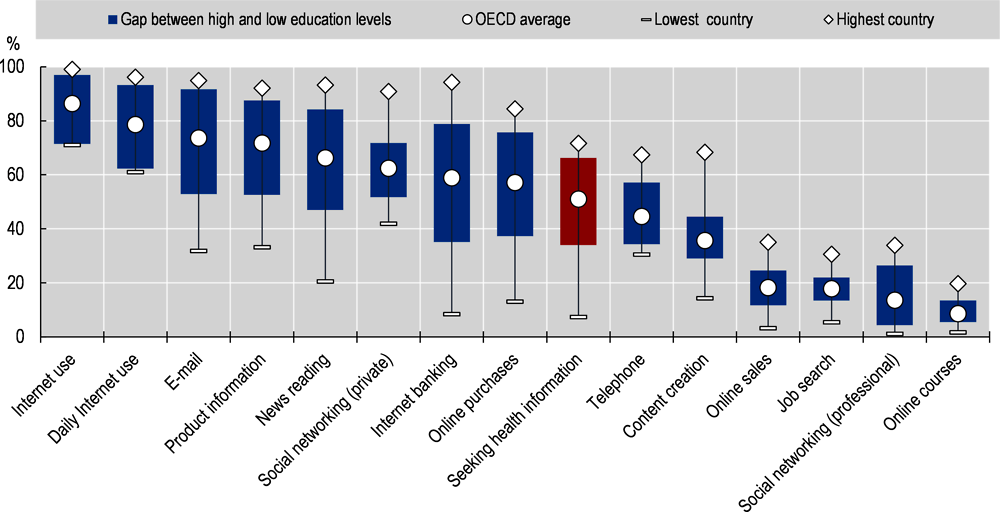
People appear to be quite willing to engage with data and information. In 2017, 3.7 billion health related smartphone apps were downloaded globally, up from 1.7 billion in 2013. The proportion of adults seeking health information on line more than doubled between 2008 and 2017 (Figure 1.7).
Digital transformation holds some promise to ‘democratise’ health and health care, and certainly to helping people better manager their own health. But for this to happen in practice, without widening health disparities, more needs to be done. For example:
-
Helping patients access and use effectively their own medical records. Section 1.3.1 outlined the growing digitalisation of health records and the rising proportion of countries that enable people to access their data electronically. However, few appear to permit individuals to interact with their own data and evidence suggests that a small proportion of people actually do so (especially those with high levels of health need – see below). In some cases legal restrictions are in place preventing interaction with data. These may need to be re-examined with a view to what is best for health outcomes and care quality.
-
Improving health and digital literacy is key. In 18 OECD countries recently surveyed, at least 30% of the population has poor health literacy levels and in 12 of those countries the proportion is over 50% (Moreira, 2018[68]). Ways to address this gap include raising digital and health literacy, but also better design of web portals or smartphone apps as well as better information about their availability.
Canada Health Infoway recently launched a country-wide campaign, Access 2022, to promote the use of electronic health records by patients and health professionals. In Norway, the government has allocated NOK 27.5 million since 2014 to increase participation in the digital health portal and developed training programs for digital skills at the municipal level.
-
Focussing on uptake among the patients who stand to benefit the most. Evidence suggests that the very complex or vulnerable people that could benefit the most from better care models do not engage with digital technology like their more healthy counterparts. The structural inequalities of digitalisation, which mirror more long-standing social stratification (Figure 1.8), are very telling in this context. In the Netherlands, for example, just 4% of the chronically ill population reported using a personal health record. Addressing this requires a specific focus on vulnerable population segments. For example, educational courses and tutorials targeted at patients with low digital literacy have been implemented in Estonia and are being trialled in the United States.
1.4.4. Opening data availability and facilitating their integration
The institutions and habits formed in the pre-digital era have entrenched fragmentation and a silo approach to doing things. Meanwhile, the utility of data for producing actionable knowledge rises exponentially if they can be combined and pooled – a requirement that is blocked by fragmentation.
Making data available to all stakeholders who can turn them into valuable knowledge is also important. In non-health sectors, opening public sector data has been shown to catalyse innovation by the private sector (OECD, 2019[1]). The openness of government data in general varies across OECD countries (Figure 1.9). Opening access to non-rivalrous health data will help transition them towards being seen as a public good. The benefits to societies and humanity of making them available on the broadest possible scale can therefore be maximised (Grossmann et al., 2010[69]; OECD, 2019[1]).
Addressing the issue of openness, and facilitating comprehensive data linkage require policy to create the right environment and implement the right levers to make progress. For example:
-
Improving the preparedness for EHR data to be used for secondary purposes such as research. Most countries are capturing clinical data electronically, but based on a 2016 OECD survey, only the countries in the upper right quadrant of Figure 1.10 report readiness to put them to work. Of note is Estonia, which has implemented a state-of-the-art digital infrastructure. Yet, it reports not being very well prepared to use this information for secondary purposes, highlighting the need for data governance and capacity to put data to work. The required operational, policy and governance levers include:
-
A national plan or strategy that includes the secondary uses of these data.
-
Having a legal framework that enables these data to be securely extracted and used for secondary purposes
-
Building the capacity to analyse the data to generate meaningful information and knowledge
-
Ensuring data completeness (population coverage), minimum data specifications, common data terminology standards, and unique patient and provider identifiers.
-
Financial incentives to not only adopt and maintain high quality electronic records, but deploy data and digital technology to improve services and outcomes (see Section 1.4.5).
-
-
Encouraging common approaches to data terminology and exchange standards. The lack of standards creates barriers to – and inefficiencies in – sharing and diffusing data within countries and across them. Other sectors have developed protocols and standards for computer communications, data exchange and cybersecurity – to the benefit of entire economies and societies. There is no reason why this cannot happen in health care. For example, Internet Protocols (TCP/IP) were adopted across the world; exchange standards for data sharing among banks, clients and financial services; and cybersecurity standards for aviation have enabled globalised control of air transportation.
The bespoke approach that has been applied to health data development, on the other hand, causes health care organisations, systems and countries to speak ‘different data languages’ – a major barrier to modernising health systems and achieving similar economic and social benefits as have been realised in other sectors. The inconsistency of health data is also a major reason for the commodification of personal health data, with profits to be made from aggregating, cleaning and harmonising large datasets.
There is some progress on developing common data terminology standards that harmonise data and enable their pooling, with a number of public and private sector initiatives currently under way. The EU has established policy to support the sharing of health data across borders, including work toward fully interoperable electronic records for research, diagnosis, treatment and disease prevention, and policies promoting effective sharing of genomic datasets to advance personalised medicine. The European Health Data and Evidence Network (EHDEN) is a shared public/private investment in developing an approach to standardising a wide range of health data. EHDEN to create a common data model to facilitate health statistics, monitoring and research undertaken by governments, universities and the private sector entities, such as for pharmaceutical research (EHDEN, 2019[70]). Global private sector initiatives such as the DaVinci project and FHIR are also aiming to establish common approaches and standards to enable the sharing of health data across borders.16
These initiatives should be welcomed. But there is a risk that their multitude exacerbates the very challenge they are trying to solve. The work that has taken place to date needs to be consolidated, and countries should agree and reach consensus on standards for the growing range of data relevant to health that can and should be shared across borders. This effort requires global coordination involving a range of stakeholders in both the public and private sectors. An international organisation such as the WHO or the OECD could facilitate this needed collaborative work.
-
Ensuring that data are available broadly, securely and at low cost. In contrast to data that are generated as a pure by-product of health care delivery or other human activities, access to some types of data whose generation entails costs may need to be subject to exclusivity through intellectual property rights. Policy on intellectual property, generally developed for tangible products, may need to evolve to strike the right balance between economic incentives to generate data and the societal benefits of open access to data (OECD, 2019[1]). This relies on solid data governance and policy frameworks (see Section 1.5.2).
1.4.5. The right incentives play a major part, and rely on policies and institutions
Transformation, especially in complex systems, does not occur organically. Transformation only occurs under the right environment, when the right incentives are aligned. The first industrial revolution began in Britain not because of the invention of steam power, which had existed for decades. Rather, it was the high cost of labour and low cost of energy (coal) in Britain at end of the 18th century (Allen, 2011[71]). Steam power was integrated into the industrial system – or rather the industrial system was reconfigured to make the most of steam technology – only when it made economic sense to do so. When it was, it transformed the industrial production methods and entire economies in the process.
Health is a highly regulated sector and the incentives, which may be financial or not, throughout health systems are heavily influenced by policy. Policies and their enabling institutions are therefore pivotal in driving a digital transformation. However, it can be argued that current policy settings create incentives that do not promote the intelligent use of data and digital technology. This dissonance may be a core reason for the slow pace of digital transformation in the health sector. It highlights the importance of re-designing the policy and institutional settings that underpin how a health system functions – and that digital transformation is not possible without institutional reform.
New payment models (see Section 1.3.6) can illustrate this issue. Remuneration plays a key part in dictating individual and institutional behaviour. While data infrastructure and digital technology provide the tools, uptake will be slow without the deeper institutional and policy changes. For example, continuing to pay for individual fragments of care will do little to stimulate the adoption of technologies that can make service delivery more people-centred materials (Murdoch and Detsky, 2013[11]). Alignment of budgetary and expenditure accountability across organisations, regions or care settings is required, and providers and provider organisation would need to move towards a team-based approach of delivering care across settings. Such fundamental changes in practice and behaviour requires tailored incentives.
Payers also need to ensure that integration of new technology does not destabilise existing services as this may compromise clinical safety as well as trust and morale among patients and providers. NHS England, for example, is in the process of updating its contracting and payment rules for primary care to address emerging challenges and embrace opportunities of digital technology because a growing share of primary care activity occurs on digital platforms. The new payment system will account for the ‘mix’ of ICT-based and face-to-face contacts. While this can only be achieved by using various forms of available data, reporting of data on the costs of digital provision in general practice is a critical part of the new model. This will enable to enable close monitoring, and continuous development of payment rules (NHS England, 2018[72]).
Harmonised information systems, appropriate skills and attitudes, ethical frameworks and engaged stakeholders provide the possibility for a positive digital transformation. But progress will be slow without a significant overhaul of existing institutional and policy frameworks that steer health system behaviour.
copy the linklink copied!1.5. A focus on strategy, governance and capacity will require sustained commitment but also deliver a healthy return on investment
A digital transformation is not an end in itself. It is a means to achieving policy objectives such as better health outcomes, equity and financial sustainability. If anything, the emergence of digital technology and its potential uses have highlighted some long-standing problems that impede any reform – digital or other – in achieving these goals. As highlighted in the previous section, digital transformation is therefore best seen as part of a more fundamental transformation of institutions that govern how health systems function.
This section outlines a tractable approach to bring about the transformation that will see data and digital technology put to work intelligently and productively. The objective is to create an enabling policy environment. Policy makers to focus on three related but sequential elements: strategy, governance and capacity. In most cases this requires additional investment or, at a minimum, a re-allocation of existing resources towards capacity-building elements. If executed well, the expected returns are considerable.
1.5.1. An overarching strategy is the foundation
All countries that are on track to harness the opportunities of health data and digital technology have one thing in common: an overarching digital strategy. This begins with the acknowledgement that data and digital technologies are a valuable resource to advancing human health, and a vision of how this resource can be used. Clearly articulating a set of principles that align with broader health system objectives can convey a number of cross-cutting advantages to driving a digital transformation at all levels of a health system. This allows better planning and execution of the necessary changes, as well as adaptation of organisational structures, institutions and workflows.
For example, in Sweden successive digital health strategies have been in place since 2006 (Swedish Ministry of Health and Social Affairs; SALAR, 2016[73]). The latest strategy was jointly developed by the national government and the Swedish Association of Local Authorities and Regions (SALAR) and endorsed in 2016 to guide the digital transformation through to 2025. The goal of the strategy is to “make it easier for people to achieve good and equal health and welfare, and to develop and strengthen their own resources for increased independence and participation in the life of society” (ibid, p.3). The Swedish strategy comprises three streams:
-
1. increasing digital information exchange, both between different public authorities and with citizens, while safeguarding privacy and data security;
-
2. advancing semantic interoperability of data in the health system; and
-
3. ensuring technical interoperability of ICT systems.
As shown previously, Sweden reports near-universal use of electronic medical records in primary care and hospitals, the second highest rate of availability and linkage of key health datasets for secondary use and the use of routine data for monitoring medicine use and expenditure. The proportion of people who access health-related information online in Sweden has increased from less than 30% in 2007 to more than 65% in 2017, which is among the highest shares across OECD countries.
Strategy is the first step to address the key problem of fragmentation
A good strategy can promote coherence across the health system silos. For example, in Israel, the digital strategy sets the foundation for cooperation between private and public entities, with the public sector setting standards for ICT and data and the private sector developing and delivering innovative digital tools. Nearly the entire Israeli population is covered by EMRs developed independently by the four Israeli health maintenance organisations (HMOs) that provide mandatory health care coverage. A digital health strategy helps working towards interoperability of these systems, creating unified EHRs that can be shared across all health and social care providers and be re-used to support research and other purposes.
A single, national strategy is particularly critical in countries with a federated system of government and/or corporatist social health insurance systems. In these situations, understanding and co-operation between states, territories and provinces, and self-governing entities is a make-or-break feature of a digital transformation at a national scale.
In Canada, for example, the federal government established Canada Health Infoway in 2001, an independent and not-for-profit organisation, to advance a pan-Canadian approach to health-related ICT and promote the implementation of a common digital architecture. Both, federal and provincial health ministries are part of the Canada Health Infoway governance framework and define priorities jointly. Federal funding is channelled to local projects through Infoway, which allows the federal government to influence the design of technical solutions and encourage provinces to implement ICT that is interoperable. However, the fragmentation of legacy systems and interoperability between provinces, and among individual health authorities between provinces, continue to be a challenge in Canada.
Cross-sectoral, whole-of government strategies appear to be most effective
The aforementioned Swedish digital health strategy builds on earlier progress of e-government in sectors outside of health care, which has improved significantly the communication between government entities and citizens and the responsiveness of such entities. The strategy covers the full range of social services and recognises that health care is an integral part, but not the only means of achieving societal goals, such as allowing everyone to live independently while participating in social life. The Swedish strategy explicitly prioritises marginalised and underserved groups to promote equitable distribution of gains from digitalisation.
Developing an overarching digital strategy also requires broad stakeholder consultation, most notably with the public. For example, in Australia, the Australian Digital Health Agency conducted a national consultation with clinicians, health care providers, payers and the general public to support the development of the national digital health strategy. The strategy was launched in 2017, and publicly supported by associations of health professionals, private sector trade associations and consumer representatives (Australian Digital Health Agency, 2017[74]).
Within the Israeli strategy, broad consultations are held to identify challenges in the health care system that are amenable to digital solutions. Tenders are then opened to provide funding to IT firms, and in particular local start-ups, to develop innovative solutions. Broad commitment to a strategy paves the way for creating the policy and technical infrastructure that enables putting data to work. Involving all relevant stakeholders is also the first critical step in establishing good governance and trust.
1.5.2. Good data governance can develop the key element of trust
Governance, in the context discussed here, means creating a policy environment that enables digital technology to be deployed, and knowledge to be extracted from data while at the same time ensuring that this is done securely, and in a way that respects individuals’ privacy and their preferences. Governance includes technical, legal and policy levers. In most countries, the key elements of governance in the context of data and digital technology such as privacy legislation were developed and instituted last century. The HIPAA Act, for example, which sets out the data privacy and security provisions for safeguarding medical information in the United States, was enacted in 1996.
The Recommendation of the OECD Council on Health Data Governance, welcomed by Health Ministers of OECD countries in 2017, sets out the fundamental elements countries need to manage and use personal health data for purposes that serve the public interest, while protecting privacy and ensuring data security. (OECD, 2019[75]). The Recommendation’s twelve mechanisms can be grouped into categories relating to technical, policy and communication requirements. Implementing the Recommendation will go some way in addressing the barriers of using data (and digital technology) and putting these to work for positive system transformation.
For example, the Recommendation provides clarity for health system leaders to communicate the benefits of a digital transformation. This enables an informed public discourse that encompasses the opportunities as well as the risks, which include, of course, the benefits foregone of not putting data to work. It also dispels the notion of a trade-off between data protection and their use. The Recommendation also contains technical requirements to ensure efficient data exchange can occur, and necessitates the institution of strict cybersecurity policies and processes. Perhaps most importantly, it is designed to promote harmonisation of policies and legal requirements governing access, management and use of personal health data within and across countries. Such ‘policy interoperability’ is critical in pooling of large datasets for public policy purposes.
A key purpose of governance is to establish trust
Lack of trust among patients, the public, data custodians and other stakeholders in how data are used and protected is a major hindrance to getting more out of data and the technologies that generate, and depend on them.
Personal health data are very sensitive, and privacy is understandably one of the most often cited issues in using them. But by generating useful knowledge, using personal health data can also make a great contribution to human health and welfare. Evidence suggests that patients and citizens are actually positively disposed to their data being used as long as the data are kept secure and are used for purposes that benefit society. Strong cybersecurity is therefore an important component of trust and data governance. Technologies such as blockchain can be deployed, but it is also important to ensure that personnel tasked with ensuring data security and integrity have the requisite skills and expertise.
It also very important to communicate the benefits of using data – as well as the risks of not using them. Transparency about when data are used, for what purpose and by whom is important. Equally, transparency, leadership and decisive action when breaches do occur. This is often lacking, and creates another barrier to better uses of data for public benefit.
Governance across sectors and across borders
Good data governance enables the health system work with the commercial sector to achieve common objectives, both in terms of processing and managing health data as well as developing digital solutions that advance health and wellbeing. It also encourages the development of common taxonomies and data standards to encourage interoperability of digital products and platforms both within and across countries.
Some countries are moving towards better engagement with the technology developers. The Israeli Ministry, for example, employs so-called Challenge Tenders. These specify a policy or technical problem that needs be solved without defining the nature or specifications of the solution. Companies are challenged to come up with the solutions to the proposed problems. This flexible approach is particularly suited to digital technologies.
In the United States, the ONC has created a prizes and challenges program to engage technology developers and incentivize digital innovation in health. The competitions focus on innovations that support: 1) ONC’s aim to clear hurdles related to the achievement of widespread adoption and interoperability; 2) ONC and HHS programs and programmatic goals; and 3) the achievement of a nationwide health IT system that improves quality, safety, and/or efficiency of health care.
The European Union is investing in elements of a pan-European information system to enable biomedical research, health system surveillance and clinical information exchange, as well as improving patients’ access to quality care and their care experience. Work is underway in areas such as data infrastructure for health system performance monitoring and research; infrastructure for clinician collaboration in patient treatment decisions and research; and data and infrastructure for biomedical and genomic research.
For example, the EU-funded CEPHOS Link project applied a common protocol to administrative data from national health care databases in six European countries (Austria, Finland, Italy, Norway, Romania, Slovenia) – all with different health care systems and varying data collection methods – to estimate psychiatric rehospitalisation rates and their predictors (Katschnig and Strassmayr, 2017[76]). The project involved data acquisition, management, quality, interoperability, privacy protection and linkage methods and included local and pooled data analyses, performed with statistical methods and innovative dynamic modelling approaches. A number of European initiatives are under way to facilitate more in-depth research based on pooled data, including research based on the human genome. A significant part of these efforts concerns harmonising data collection and exchange standards across borders.
In addition to technical interoperability, alignment of policy and governance frameworks is also essential. If regulations regarding privacy, transparency and control over data are not aligned between countries, common data languages will do little to advance putting data to work on a global scale. The OECD Council Recommendation provides a mechanism to harmonise national data policy and governance frameworks that goes some way to create a global information ecosystem that can extract knowledge from large pools of health data but do so securely and in accordance with agreed regulatory principles (OECD, 2019[75]).
1.5.3. Building capacity for a digital transformation requires investment
Strategy and governance are very important. But without the institutional, operational and policy capacity to extract knowledge from data and then deploy this knowledge effectively, any potential for positive system transformation will not be realised.
Capacity building covers the barriers and enablers discussed in Section 1.4. It also means ensuring that the underlying infrastructure is in place to enable data to be put to work effectively. This applies to hardware as well as software and other intangible products to generate, store, link and analyse data.
Institutional capacity must not be neglected. The best digital strategies, governance frameworks and skilled workforce will not ensure that knowledge extracted from data is applied to meet policy objectives. Existing policies, processes and workflows need to be reformed in a way that enables data-driven knowledge to be applied most effectively. It means equipping agencies and organisation with access to data and the ability to extract knowledge from them. It also means arming these institutions with the necessary ‘teeth’ to act on the knowledge generated. The roles, responsibilities and powers of regulators, payers, public health authorities and other health system actors must be aligned with what a data-driven approach can do.
This includes re-thinking the prevailing macro-policy settings and institutions that dictate how things are done in health. This concerns not just remuneration, but also how regulation is set and enforced or how performance is evaluated. Policy makers must think about lowering the barriers for smart deployment of digital technologies and intelligent uses of data that can help achieve policy objectives – from better quality care, to using scarce resources more efficiently at all levels of the system.
Targeted and sustained investment is needed
The complexity – and cost – of successfully implementing the actions discussed above requires sustained investment. OECD countries typically invest considerably fewer resources than other sectors on information systems (OECD/WHO/World Bank Group, 2018[25]). This is surprising for an information-intensive industry. More targeted investment is certainly needed to better manage data and information. However, in most cases the investment should be principally targeted at institutional and policy reforms, skills and expertise of the workforce, and demand-side capacity. This is because the majority of costs of implementing a data-driven innovations and digital technologies in the health sector are tied up in the planning, preparing personnel and redesigning process. Capital expenditure can represent only about a quarter of the overall implementation costs. The dominance of costs related to capacity-building and workflow redesign align with the long-standing findings on digital technology and its role in productivity (Brynjolfsson and Hitt, 1998[77]). Moreover, the initial costs of implementing digital platforms dwarf ongoing, marginal costs of maintenance, which can be as low as 3.5% of the initial costs (Fleming et al., 2011[78]).
The most pressing areas for investment are human capital and expertise, adapting processes and workflows, and – critically – solid policy and governance frameworks to ensure benefits are maximised while risks are managed. Investment is required within communities, in the health workforce and in the policy capacity to turn knowledge into meaningful action.
1.5.4. But the returns can be considerable
Digital technology is general-purpose, meaning that it can penetrate all aspects and activities of an organisation or endeavour (Brynjolfsson, Rock and Syverson, 2019[27]). Rather than creating new things to do (a main driver of spending growth in health), data and digital technology are particularly suited to improve virtually every existing process and activity in an organisation, industry or sector (see Section 1.2.2). The resulting efficiencies and productivity gains of small and incremental as well as large innovations are considerable but also difficult to quantify ex ante. For example, thirty years ago it would have been impossible to predict the myriad ways that the internet would transform the global economy.
Capturing the macroeconomic effects of a fundamental system transformation, the costs and benefits within and outside the health system, is a challenging task. Suitable economic models are yet to be developed (Marino and Lorenzoni, 2019[13]). Nevertheless, by making virtually every aspect of what a health system does more efficient and productive, the expected health and economic dividends of a digital transformation in health are considerable – even when factoring in increased investment The dividend can be broken into two parts:
-
1. reducing wasteful and inefficient practices, redundant processes and clinical harm, and
-
2. addressing unmet health need, improving public health and enabling access to safer and better therapies.
Reducing wasteful and inefficient practices
As described previously, approximately a fifth of health care expenditure generate no benefit to people and populations and, sometimes, their effects are even detrimental (OECD, 2017[29]). Across OECD health systems, 20% of waste amounts to over USD 1.3 trillion per year. However, the health sector in some countries is considerably more inefficient and wasteful, with pricing failure, administrative complexity, and fraud among the key drivers of (Shrank, Rogstad and Parekh, 2019[79]).
Leveraging data and digital technologies can help reduce this waste in the ways outlined in Section 1.3 and the remainder of this report. Even a relatively modest reduction of 30% would amount to approximately USD 400 billion per year across OECD countries. This would be principally achieved by improving clinical, operational and administrative efficiency, and removing redundant activities and wasteful practices.
Improving health outcomes
More intelligent use of data and digital technologies can also improve public health and address unmet health need more effectively. Harnessing real-world-data can also enable the continued development of safer and better treatments, and help integrate them into service delivery in a sustainable way. Such improvements can also deliver considerable economic benefits through healthier and more productive populations. Some of these returns, would be spent on breakthrough biomedical technologies. On the other hand, more agile and outcome-driven remuneration of treatments and services across an entire health system could deliver much improved value and efficiency.
The combining economic benefits of putting data and digital technology to work in health to improve efficiency, reduce waste, address unmet need and improve population health care could amount to USD 600 billion each year This is equates roughly to the GDP of Poland, and represents about 8% of current health expenditure across OECD countries. It is a conservative estimate and, compared to existing projections, is not far-fetched.
-
Projected savings generated by leveraging digital technology and data in the health sector have been as high as 17% of health care expenditure (Kayyali and Van Kuiken, 2013[80]).
-
It is estimated that digital technology in National Health Service (NHS) of the United Kingdom has the potential to deliver efficiencies amounting to of GBP 13 billion a year (OECD, 2017[12]).
-
NHS data alone have been valued at GBP 9.6 billion per annum, the value generated principally by the new knowledge and insights that could be unlocked from them (EY, 2019[81]). This is approximately 5% of health expenditure in the United Kingdom (OECD, 2019[82]).
-
Interoperability between electronic data platforms in the United States is said to potentially deliver annual savings approaching USD 100 billion (OECD, 2017[12]).
Based on these figures, additional investment equivalent to 2-4% of health care expenditure to promote more intelligent use of data for information and knowledge (effectively a doubling of current investment levels)17 could equate to a healthy return of approximately 3 to 1. In some cases, simply redirecting existing resources towards the key areas described above – capacity building and data governance – could achieve the expected returns.
copy the linklink copied!1.6. Conclusion
The explosion of data and digital technology has led to significant improvements, value and surpluses in a range of sectors. In the health sector, the potential health and societal benefits of using data and digital technologies are profound. The information and knowledge derived from existing data can be used to deliver not only better care, better public health and faster access to better treatments but also more efficient management and administration of complex health systems. A digital transformation can help deliver better health more efficiently and equitably.
However, health lags far behind other sectors in this regard. But the barriers to catching up are not technological, but institutional and organisational. The data as well as the technologies and infrastructure to use them are mostly there. Failing to exploit them is costly and wasteful. Indeed, the difficulties of achieving a true digital transformation has served to highlight structural problems – such as fragmentation and silos – that pre-date the digital era and have hindered progress for decades. These cannot be fixed by simply digitising what health systems do, It needs an overhaul of policy settings and institutions. In a sense, digital technology is a Trojan horse for a more badly needed deeper transformation in health. Instituting such a transformation is a political choice. It will not happen without leadership and policy action.
In order to progress, countries must invest in strategy, governance as well as institutional and operational capacity. Increasing current investment, or in some cases simply re-allocating existing resources, targeted at improving governance and capacity can promote a digital transformation and deliver a healthy return approaching 10% of what OECD countries currently spend on health care.
References
[71] Allen, R. (2011), “Why the industrial revolution was British: commerce, induced invention, and the scientific revolution1”, The Economic History Review, Vol. 64/2, pp. 357-384, https://doi.org/10.1111/j.1468-0289.2010.00532.x.
[8] Asch, J. et al. (2019), “Google search histories of patients presenting to an emergency department: an observational study”, BMJ Open, Vol. 9/2, p. e024791, https://doi.org/10.1136/bmjopen-2018-024791.
[33] Auraaen, A., L. Slawomirski and N. Klazinga (2018), “The economics of patient safety in primary and ambulatory care: Flying blind”, OECD Health Working Papers, No. 106, OECD Publishing, Paris, https://dx.doi.org/10.1787/baf425ad-en.
[74] Australian Digital Health Agency (2017), Health Ministers approve Australia’s National Digital Health strategy, https://www.digitalhealth.gov.au/news-and-events/news/health-ministers-approve-australia-s-national-digital-health-strategy.
[32] Banger, A. and M. Graber (2015), Recent Evidence that Health IT Improves Patient Safety Issue Brief Recent Evidence that Health IT Improves Patient Safety - Issue Brief, US Department for Health and Human Services, Washington D.C., https://www.healthit.gov/sites/default/files/brief_1_final_feb11t.pdf (accessed on 19 November 2018).
[35] Barbabella, F. et al. (2017), How can eHealth improve care for people with multimorbidity in Europe?, NIVEL and TU Berlin, Utrecht, Netherlands, http://www.icare4eu.org/pdf/PB_25.pdf.
[10] Bates, D. et al. (2018), “Why Policymakers Should Care About “ Big Data ” in Healthcare”, Health Policy and Technology, Vol. 7/2, https://doi.org/10.1016/j.hlpt.2018.04.006.
[28] Baumol, W. (1967), “Macroeconomics of Unbalanced Growth: The Anatomy of Urban Crisis”, The American Economic Review, Vol. 57/3, pp. 415-426, https://www.jstor.org/stable/1812111.
[61] Biemba, G. (ed.) (2018), “Considerations for ethics review of big data health research: A scoping review”, PLOS ONE, Vol. 13/10, p. e0204937, https://doi.org/10.1371/journal.pone.0204937.
[62] Bourne, P. (ed.) (2015), “Ethical Challenges of Big Data in Public Health”, PLOS Computational Biology, Vol. 11/2, p. e1003904, https://doi.org/10.1371/journal.pcbi.1003904.
[40] Boyd, D. and K. Crawford (2012), “Critical questions for big data: Provocations for a cultural, technological, and scholarly phenomenon”, Information, Communication & Societ`y, Vol. 15/5, pp. 662–679, https://doi.org/10.1080/1369118X.2012.678878.
[22] Brynjolfsson, E., F. Eggers and A. Gannamaneni (2018), Using Massive Online Choice Experiments to Measure Changes in Well-being, National Bureau of Economic Research, Cambridge, MA, https://doi.org/10.3386/w24514.
[77] Brynjolfsson, E. and L. Hitt (1998), “Beyond the productivity paradox”, Communications of the ACM, Vol. 41/8, pp. 49-55, https://doi.org/10.1145/280324.280332.
[27] Brynjolfsson, E., D. Rock and C. Syverson (2019), “The Productivity J-Curve: How Intangibles Complement General Purpose Technologies”, SSRN Electronic Journal, https://doi.org/10.2139/ssrn.3346739.
[15] Burki, T. (2019), “GP at hand: a digital revolution for health care provision?”, The Lancet, Vol. 394/10197, pp. 457-460, https://doi.org/10.1016/s0140-6736(19)31802-1.
[26] Calvino, F. et al. (2018), “A taxonomy of digital intensive sectors”, OECD Science, Technology and Industry Working Papers, No. 2018/14, OECD Publishing, Paris, https://dx.doi.org/10.1787/f404736a-en.
[19] Computer World (2019), Q and A: Christiana Care Health CIO talks up Apple’s Health Record App, https://www.computerworld.com/article/3365242/qa-chistina-care-health-cio-talks-up-apples-health-record-app.html (accessed on 11 July 2019).
[83] Cowen, T. (n.d.), Public Goods, The Library of Economics and Liberty, https://www.econlib.org/library/Enc/PublicGoods.html (accessed on 15 Aug 2019).
[4] DOMO (2017), Data Never Sleeps 5.0, https://www.domo.com/learn/data-never-sleeps-5.
[70] EHDEN (2019), European Health Data and Evidence Network, https://www.ehden.eu/ (accessed on 11 July 2019).
[54] European Commission (2013), Benchmarking Deployment of eHealth among General Practitioners, European Commission - Directorate-General of Communications Networks. Content & Technology.
[55] European Health Parliament (2016), Digital skills for health professionals, https://www.healthparliament.eu/digital-skills-health-professionals/.
[81] EY (2019), Realising the value of heath care data: Realising the value of heath care data: a framework for the future, https://assets.ey.com/content/dam/ey-sites/ey-com/en_gl/topics/life-sciences/life-sciences-pdfs/ey-value-of-health-care-data-v20-final.pdf.
[78] Fleming, N. et al. (2011), Exploring Financial and Non-Financial Costs and Benefits of Health Information Technology: The Impact of an Ambulatory Electronic Health Record on Financial and Workflow in Primary Care Practices and Costs of Implementation.
[2] Floridi, L. (2014), The Fourth Revolution - How the Infosphere is Reshaping Human Reality, Oxford University Press.
[17] Forbes (2018), Flatiron health acquisition a shot in the arm for roches oncology real world evidence needs, https://www.forbes.com/sites/reenitadas/2018/02/26/flatiron-health-acquisition-a-shot-in-the-arm-for-roches-oncology-real-world-evidence-needs/#75219f1e3f60.
[18] Fortune (2016), Why IBM Is Dropping $2.6 Billion on Truven Health, https://fortune.com/2016/02/18/ibm-truven-health-acquisition/.
[52] Foster, J. and J. Bryce (2009), “Australian nursing informatics competency project”, Studies in Health Technology and Informatics, Vol. 146, pp. 556-60, https://doi.org/10.3233/978-1-60750-024-7-556.
[38] Fralick, M. et al. (2018), “Use of Health Care Databases to Support Supplemental Indications of Approved Medications”, JAMA Internal Medicine, Vol. 178/1, p. 55, https://doi.org/10.1001/jamainternmed.2017.3919.
[23] Galetsi, P., K. Katsaliaki and S. Kumar (2019), “Values, challenges and future directions of big data analytics in healthcare: A systematic review”, Social Science & Medicine, Vol. 241, p. 112533, https://doi.org/10.1016/j.socscimed.2019.112533.
[69] Grossmann, C. et al. (eds.) (2010), Clinical Data as the Basic Staple of Health Learning: Creating and Protecting a Public Good: Workshop Summary, The National Academies Press, https://doi.org/10.17226/12212.
[20] Healthcare Weekly (2019), How the “Big 4” Tech Companies Are Leading Healthcare Innovation, https://healthcareweekly.com/how-the-big-4-tech-companies-are-leading-healthcare-innovation/.
[51] Hegney, D. et al. (2007), Nurses and information technology, Australian Nursing Federation, http://www.anf.org.au/it_project/PDF/IT_Project.pdf.
[7] Huesch, M. and T. Mosher (2017), Using It or Losing It? The Case for Data Scientists Inside Health Care, https://catalyst.nejm.org/case-data-scientists-inside-health-care/.
[3] IBM (2017), 10 Key Marketing Trends for 2017 and Ideas for Exceeding Customer Expectations, https://www-01.ibm.com/common/ssi/cgi-bin/ssialias?htmlfid=WRL12345USEN (accessed on 23 August 2018).
[16] IQVIA (2019), IQVIA Core, https://www.iqvia.com/about-us/iqvia-core.
[46] Jo, E. and P. Drury (2015), “Development of a Virtual Diabetes Register using Information Technology in New Zealand.”, Healthcare informatics research, Vol. 21/1, pp. 49-55, https://doi.org/10.4258/hir.2015.21.1.49.
[76] Katschnig, H. and C. Strassmayr (2017), Comparative Effectiveness Research on Psychiatric HOSpitalisation by record LINKage of large administrative data sets in six European countries, https://thl.fi/documents/189940/2732416/CEPHOS-LINK+final+scientific+report+2017-03-31+export.pdf/6f206810-5919-415c-82a1-884795732186.
[80] Kayyali, B. and S. Van Kuiken (2013), The big-data revolution in US health care, https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/the-big-data-revolution-in-us-health-care.
[64] Koskinen, J., V. Kainu and K. Kimppa (2016), “The concept of Datenherrschaft of patient information from a Lockean perspective”, Journal of Information, Communication and Ethics in Society, Vol. 14/1, pp. 70-86, https://doi.org/10.1108/jices-06-2014-0029.
[63] Koskinen, J. and K. Kimppa (2016), “An Unclear Question: Who Owns Patient Information?”, in IFIP Advances in Information and Communication Technology, Technology and Intimacy: Choice or Coercion, Springer International Publishing, Cham, https://doi.org/10.1007/978-3-319-44805-3_1.
[59] Maier, C., L. Aiken and R. Busse (2017), “Nurses in advanced roles in primary care: Policy levers for implementation”, OECD Health Working Papers, No. 98, OECD Publishing, Paris, https://dx.doi.org/10.1787/a8756593-en.
[13] Marino, A. and L. Lorenzoni (2019), “The impact of technological advancements on health spending: A literature review”, OECD Health Working Papers, No. 113, OECD Publishing, Paris, https://dx.doi.org/10.1787/fa3bab05-en.
[21] McKinsey (2019), Digital transformation: Improving the odds of success, https://www.mckinsey.com/business-functions/mckinsey-digital/our-insights/digital-transformation-improving-the-odds-of-success.
[24] McKinsey (2019), How the British Army’s operations went agile, https://www.mckinsey.com/business-functions/organization/our-insights/how-the-british-armys-operations-went-agile.
[37] Melchiorre, M. et al. (2018), “eHealth in integrated care programs for people with multimorbidity in Europe: Insights from the ICARE4EU project”, Health Policy, Vol. 122/1, pp. 53-63, https://doi.org/10.1016/j.healthpol.2017.08.006.
[6] Ministry of Foreign Affairs Denmark (2016), Start with Denmark, https://www.regioner.dk/media/3759/270916-startwithdenmark2016-fullreport.pdf.
[68] Moreira, L. (2018), “Health literacy for people-centred care: Where do OECD countries stand?”, OECD Health Working Papers, No. 107, OECD Publishing, Paris, https://dx.doi.org/10.1787/d8494d3a-en.
[11] Murdoch, T. and A. Detsky (2013), “The Inevitable Application of Big Data to Health Care”, JAMA, Vol. 309/13, p. 1351, https://doi.org/10.1001/jama.2013.393.
[43] National Alliance Of Healthcare Purchaser Coalitions (2018), Employers’ perceptions & actions related to healthcare waste.
[50] Nedelkoska, L. and G. Quintini (2018), “Automation, skills use and training”, OECD Social, Employment and Migration Working Papers, No. 202, OECD Publishing, Paris, https://dx.doi.org/10.1787/2e2f4eea-en.
[36] NHS Digital (2019), Patient Online Management Information (POMI), https://digital.nhs.uk/data-and-information/data-collections-and-data-sets/data-collections/pomi.
[72] NHS England (2018), Digital-first primary care and its implications for general practice payments, https://www.engage.england.nhs.uk/survey/digital-first-primary-care/user_uploads/digital-first-access-to-gp-care-engagement-document.pdf (accessed on 5 July 2018).
[34] Oderkirk, J. (2017), “Readiness of electronic health record systems to contribute to national health information and research”, OECD Health Working Papers, No. 99, OECD Publishing, Paris, https://dx.doi.org/10.1787/9e296bf3-en.
[1] OECD (2019), Going Digital: Shaping Policies, Improving Lives, OECD Publishing, Paris, https://dx.doi.org/10.1787/9789264312012-en.
[82] OECD (2019), Health system accounts, https://stats.oecd.org/ (accessed on 12 May 2019).
[67] OECD (2019), “ICT Access and Usage by Households and Individuals”, OECD Telecommunications and Internet Statistics (database), https://dx.doi.org/10.1787/b9823565-en (accessed on 4 November 2019).
[60] OECD (2019), Recommendation of the Council on Artificial Intelligence, OECD Publishing, Paris, https://legalinstruments.oecd.org/en/instruments/OECD-LEGAL-0449.
[75] OECD (2019), Recommendation of the Council on Health Data Governance, OECD Publishing, Paris, https://legalinstruments.oecd.org/en/instruments/OECD-LEGAL-0433.
[44] OECD (2019), Survey on health data governance: preliminary results.
[39] OECD (2019), Using routine data to inform pharmaceutical policies, https://www.oecd.org/health/health-systems/Using-Routinely-Collected-Data-to-Inform-Pharmaceutical-Policies-Analytical-Report-2019.pdf.
[58] OECD (2018), Feasibility Study On Health Workforce Skills Assessment - Supporting health workers achieve person-centred care, https://www.oecd.org/health/health-systems/Feasibility-Study-On-Health-Workforce-Skills-Assessment-Feb2018.pdf.
[12] OECD (2017), New Health Technologies: Managing Access, Value and Sustainability, OECD Publishing, Paris, https://dx.doi.org/10.1787/9789264266438-en.
[29] OECD (2017), Tackling Wasteful Spending on Health, OECD Publishing, Paris, https://dx.doi.org/10.1787/9789264266414-en.
[9] OECD (2017), The Next Production Revolution: Implications for Governments and Business, OECD Publishing, Paris, https://dx.doi.org/10.1787/9789264271036-en.
[48] OECD (2016), Better Ways to Pay for Health Care, OECD Health Policy Studies, OECD Publishing, Paris, https://dx.doi.org/10.1787/9789264258211-en.
[45] OECD (2015), Health Data Governance: Privacy, Monitoring and Research, OECD Health Policy Studies, OECD Publishing, Paris, https://dx.doi.org/10.1787/9789264244566-en.
[25] OECD/WHO/World Bank Group (2018), Delivering Quality Health Services: A Global Imperative, World Health Organization, Geneva 27, https://dx.doi.org/10.1787/9789264300309-en.
[41] O’Neill, D. and D. Scheinker (2018), Wasted Health Spending: Who’s Picking Up The Tab?, https://doi.org/10.1377/hblog20180530.245587.
[56] Quaglio, G. et al. (2016), “E-Health in Europe: Current situation and challenges ahead”, Health Policy and Technology, Vol. 5, pp. 314-317, https://doi.org/10.1016/j.hlpt.2016.07.010.
[65] Rodwin, M. (2009), “The Case for Public Ownership of Patient Data”, JAMA, Vol. 302/1, p. 86, https://doi.org/10.1001/jama.2009.965.
[57] Rudin, R. et al. (2016), Identifying and Coordinating Care for complex patients: Findings from the Leading Edge of Analytics and Health Information Technology, RAND Corporation, http://www.rand.org/t/rr1234.
[49] Safavi, K., D. Bates and S. Chaguturu (2019), Harnessing Emerging Information Technology for Bundled Payment Care Using a Value-Driven Framework, https://catalyst.nejm.org/harnessing-it-bundled-payment-care/ (accessed on 20 Oct 2019).
[14] Shah, N., C. Farkas and B. Kocher (2019), Build vs. Buy: What Should Health Systems Do?, NEJM, https://catalyst.nejm.org/build-buy-health-integrated-systems/.
[47] Sheikh, A. (ed.) (2019), “Health system costs for individual and comorbid noncommunicable diseases: An analysis of publicly funded health events from New Zealand”, PLOS Medicine, Vol. 16/1, p. e1002716, https://doi.org/10.1371/journal.pmed.1002716.
[79] Shrank, W., T. Rogstad and N. Parekh (2019), “Waste in the US Health Care System”, JAMA, Vol. 322/15, https://doi.org/10.1001/jama.2019.13978.
[53] Skills for Health (2012), How do new technologies impact on workforce organisation? Rapid review of international evidence, Skills for Health, Bristol.
[31] Slawomirski, L., A. Auraaen and N. Klazinga (2017), “The economics of patient safety: Strengthening a value-based approach to reducing patient harm at national level”, OECD Health Working Papers, No. 96, OECD Publishing, Paris, https://dx.doi.org/10.1787/5a9858cd-en.
[73] Swedish Ministry of Health and Social Affairs; SALAR (2016), Vision for eHealth 2025.
[30] The Economist (2019), Driverless cars are stuck in a jam, https://www.economist.com/leaders/2019/10/10/driverless-cars-are-stuck-in-a-jam.
[42] WHA (2018), First, do no harm: Calculating health care waste in Washington State, https://www.wacommunitycheckup.org/media/47156/2018-first-do-no-harm.pdf.
[5] Will, C. (2011), “Mutual benefit, added value? Doing research in the National Health Service”, Journal of Cultural Economy, Vol. 4/1, pp. 11-26, https://doi.org/10.1080/17530350.2011.535332.
[66] World Health Assembly (2004), WHA57.18. Human organ and tissue transplantation.
Notes
← 1. The systems and infrastructure that store data and the software that enables secure sharing all have significant costs. However, theses costs are distributed across all of the instances when the data are used and re-used. The more often this occurs the lower the marginal cost. It is also true that re-using data other analyses requires strong governance mechanisms that prevent unauthorised use and ensure security, privacy and consent. Governance is not cost-free but, again, the costs diminish at the margin and, as illustrated in this report, the returns can be considerable.
← 2. A public good is something that is non-rivalrous (use by one individual does not reduce availability to others or the good can be effectively consumed simultaneously by more than one person) and non-excludable (individuals cannot be excluded from its use) (Cowen, n.d.[83]). Classic examples of public goods are lighthouses and national defence forces. Data fulfil the non-rivalry criterion. However, they are frequently controlled by organisations, firms and individuals. This means that their non-excludability relies on public policy, specifically data regulation and governance. The importance of governance is a key theme of this chapter and this report.
← 3. In this report, the term ‘health system’ describes how the provision of services that aim to achieve health policy objectives is organised at national level. This includes organisations, agencies and institutions that deliver health care and medical services as well those responsible for public health interventions and policies. Health systems can also refer to sub-national system or network of health service providers, but the distinction is specified where relevant in this report.
← 4. See Chapter 6 (Data without borders) for further discussion of this issue.
← 5. See Chapter 5 (Box 5.1) for a definition of big data.
← 6. See Chapter 6 for further discussion on biomedical technology and routine data.
← 7. The reality of these predictions is addressed in Chapter 4 of this report.
← 8. An electronic medical record (EMR) – sometimes called an Electronic Patient Record – is a computerized medical record for individuals created in a service or an organisation that delivers care, e.g. hospital, physician's office or long-term care facility. EMRs are typically unique to the provider or organisation, and allow storage, retrieval and modification of its patient records. An electronic health record (EHR) is a longitudinal digital record that contains a history of all contact with the health system for an individual regardless of the settings, service and organisation at which the contact took place. This can be achieved by either having one EHR across all settings and organisations in a health system (‘one patient - one record’), or provide a platform that can link multiple EMRs so that the information can be shared between settings and relevant agencies that use the data. Source: OECD survey on secondary use of EHR data, 2016 (Oderkirk, 2017[34]).
← 9. For more detail on better service delivery and people-centred care, see Chapters 2 and 3.
← 10. More detail on risk-stratification is provided in Chapters 2 and 8.
← 11. More detail on managing biomedical technology using available data is provided in Chapter 7.
← 12. More detailed discussion on public health and Big Data can be found in Chapters 5 and 8.
← 13. A more detailed discussion on harnessing data for health system governance and stewardship can be found in Chapter 8.
← 14. More detail on potential funding models is provided in Chapter 8.
← 15. More detail is provided in Chapter 4.
← 16. More detail on approaches to harmonise health data is provided in Chapter 6.
← 17. Based on estimates that 2-4% of health expenditure in developed countries is invested in information systems.
Metadata, Legal and Rights
https://doi.org/10.1787/e3b23f8e-en
© OECD 2019
The use of this work, whether digital or print, is governed by the Terms and Conditions to be found at http://www.oecd.org/termsandconditions.