Mortality following stroke
Stroke is the second leading cause of death after heart disease in Europe (see the indicator “Mortality from circulatory diseases” in Chapter 3). Across EU countries, stroke accounted for 375 000 deaths in 2017, and the number is expected to rise by one-third by 2035 due to population ageing and increases in some risk factors (OECD/The King’s Fund, 2020). Of the two types of stroke, about 85% are ischaemic (caused by clotting) and 15% are haemorrhagic (caused by bleeding).
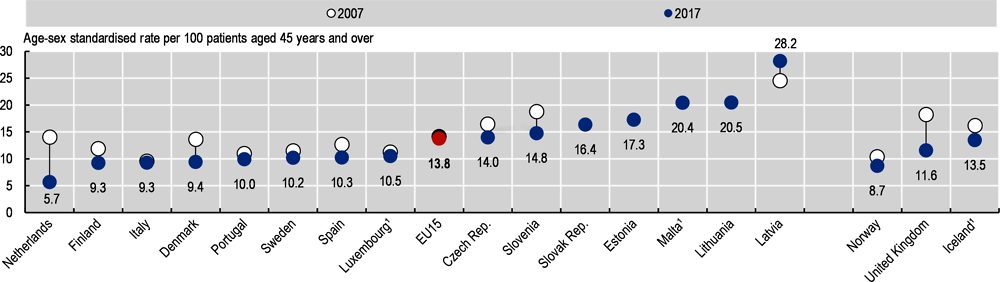
Figure 6.15 shows mortality rates within 30 days of hospital admission for ischaemic stroke where the death occurred in the same hospital as the initial admission (unlinked data). Figure 6.16 shows mortality rates where deaths are recorded regardless of where they occurred, including in another hospital or outside the hospital (linked data).
Using unlinked data, the mortality rates within 30 days of hospital admission for ischaemic stroke were highest in Latvia, Malta and Lithuania with rates over 15% in 2017. They were lowest in Nordic countries (Denmark, Iceland, Norway and Sweden) and in the Netherlands with rates of less than 6%. Generally, countries that have 30-day mortality rates for ischaemic stroke lower than the EU average also tend to have lower 30-day mortality rates for acute myocardial infarction (AMI) (see indicator “Mortality following acute myocardial infarction”). This suggests that certain aspects of acute care delivery influence outcomes for both stroke and AMI patients.
Across the smaller group of countries that reported linked data, the case-fatality rates were highest in Latvia and Lithuania, with over 20% of patients dying within 30 days of being admitted to hospital for stroke. They were lowest in the Netherlands and Norway, with rates below 9%. These rates are higher than those based on unlinked data because they capture all deaths.
Treatment for ischaemic stroke has advanced greatly over the last decades, with more effective systems and processes now in place in many European countries including specialised stroke units involving multidisciplinary teams devoted to care for stroke patients, and medical progress such as thrombolysis and thrombectomy (OECD, 2015). Between 2007 and 2017, 30-day case-fatality rates for ischaemic stroke decreased by over 15% on average across EU countries, based either on unlinked data (a reduction from 11.4% to 9.0%) or linked data (a reduction from 14.2% to 12.0%).
Since the onset of the COVID-19 pandemic, reduced or delayed access to care for stroke patients and stretched resources for stroke care delivery have been reported in some countries (Aguiar de Sousa et al., 2020; Bersano et al., 2020). This highlights the importance of continuous monitoring of mortality rates after hospital admissions for stroke to assess any impact of COVID-19 in the provision of timely and quality care to stroke patients.
Mortality rates following hospital admissions for ischaemic stroke vary not only across countries, but also across different hospitals in each country. Figure 6.17 shows that differences in 30-day mortality rates across hospitals within each country are often larger than differences across countries. Reducing these variations is key to providing more equitable care and reducing overall mortality rates.
Strategies to reduce mortality rates from stroke include providing timely transportation of patients, timely delivery of reperfusion therapy through pre-hospital triage via telephone or in the ambulance, evidence-based medical interventions and access to high-quality specialised facilities such as stroke units (OECD, 2015).
National mortality rates are defined in indicator “Mortality following acute myocardial infarction”. The definition of ischaemic stroke only includes ICD-10 codes I63-I64 and may differ from broader definitions used at the national level.
Figure 6.17 is a turnip plot that graphically represents the relative dispersion of rates across hospitals in each country. The data include only ICD-10 I63 (cerebral infarction). Hospitals with fewer than 50 stroke admissions are excluded to improve data reliability. Rates are adjusted for age, sex, co-morbidity, stroke severity and previous stroke (linked data only).
References
Aguiar de Sousa, D. et al. (2020), “Maintaining stroke care in Europe during the COVID-19 pandemic: Results from an international survey of stroke professionals and practice recommendations from the European Stroke Organisation”, European Stroke Journal, https://doi.org/10.1177/2396987320933746.
Bersano, A. et al. (2020), “Stroke care during the COVID-19 pandemic: experience from three large European countries”, European Journal of Neurology, Vol. 27, https://doi.org/10.1111/ene.14375.
OECD/The King's Fund (2020), Is Cardiovascular Disease Slowing Improvements in Life Expectancy?: OECD and The King's Fund Workshop Proceedings, OECD Publishing, Paris, https://doi.org/10.1787/47a04a11-en.
OECD (2016), OECD Reviews of Health Systems: Latvia 2016, OECD Publishing, Paris, https://doi.org/10.1787/9789264262782-en.
OECD (2015), Cardiovascular Disease and Diabetes: Policies for Better Health and Quality of Care, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/2074319x.