2. Recent trends in internationalisation of medical education
The number of international students pursuing medical education away from their home country has increased significantly over the past decade, with some countries becoming popular destinations. For example, around half of all medical students in Ireland, nearly a third in Romania and a quarter in Poland are international students. This mobility of students is driven by demand and supply factors, including admission limits in medicine in the home countries of these students and active recruitment strategies of some medical schools. The mobility has been supported by the mutual recognition of qualifications, particularly across EU member states. Most international students from OECD countries studying medicine abroad intend to return to their home country to complete their postgraduate training and work as doctors. While most students from countries like Israel, Norway, Sweden, and France are able to do this, this is not the case for many students from countries like Canada or the United States who are facing a bottleneck when they wish to return to their home country, as the number of training/residency posts is significantly lower than the number of applicants. This raises the risks of a waste in human capital if these new international medical graduates are not able to complete their training.
The statistical data for Israel are supplied by and under the responsibility of the relevant Israeli authorities. The use of such data by the OECD is without prejudice to the status of the Golan Heights, East Jerusalem and Israeli settlements in the West Bank under the terms of international law.
2.1. Introduction
The number of international students (i.e. students enrolled in a study programme in a country other than their country of origin) rose from 2 million worldwide in 1999 to 5 million in 2016, of which 3.5 million were studying in OECD countries. They represent about 6% of the total number of university students across all OECD countries, with the proportion rising to more than one in ten students at the master’s level (OECD, 2018[1]). The international mobility of medical students is no exception: The number of international students enrolled in OECD countries in the field of health1 exceeded 270 000 in 2016, a 25% increase in just three years from around 215 000 in 2013.
As noted in Chapter 1 (see Table 1.A.1), the number of new domestically-trained medical graduates has increased significantly over the past decade across nearly all OECD countries, but in some countries a growing number of them are international students. Historically, international medical students studying in OECD countries were coming mainly from lower-income countries that did not have a sufficient capacity to train doctors. Nowadays, an increasing number come from other OECD countries rather than from outside the OECD area.
A number of factors have contributed to the growing international mobility of medical students: Numerus clausus policies that limit entry into medical education programmes in many countries have provided incentives for many students to study abroad, particularly in the European Union (EU) countries, because there is recognition of medical qualifications across all EU/EFTA countries since 2005. The accession of 13 new EU member states since 2004 has increased greatly the number of countries where EU/EFTA students can pursue a medical degree while being sure that it will be recognised in all others. Moreover, medical schools in some countries have engaged in active marketing strategies to attract international students – notably by creating programmes in English or French to reduce the language barrier – because these students bring additional incomes by paying higher tuition fees than domestic students.
The growing internationalisation of medical education entails additional complexities and uncertainties for national medical workforce planning and policies to regulate the number of graduates getting into further stages of medical training, because these international students are mobile: they may either stay in their country of education after graduation or return to their home country or move to a third country to pursue their postgraduate training and work as a doctor. While the growing number of these international graduates may help fill the needs for new doctors in the countries to which they will be heading, they may also put pressures to expand the number of internship and postgraduate specialty training places required to become a fully-trained doctor, either in the country where they have obtained their first medical degree or in their country of origin if they decide to return home.
This chapter provides an overview of recent trends in the international mobility of medical students enrolled in long-cycle study programmes, revealing the growing magnitude and complexity of the phenomenon. It also provides additional insights into the factors that motivate young people to emigrate at least temporarily to study medicine as well as the potential benefits and risks that these decisions might have on their professional careers and on the medical education and training systems in the countries of education and destination.
This chapter draws mainly on the findings from five country case studies presented in Part II of this report. These include four case studies of European countries that receive a large number of international medical students (France, Ireland, Poland, and Romania) as well as a study on the labour market integration of Canadian and foreign-born doctors trained in Canada or abroad.
2.2. A growing number of students follow medical education abroad before returning to their home countries
While data on the number of international medical students are not yet systematically captured across OECD or EU countries, the data available from some countries reveal that their numbers are growing (see also Box 2.1. For example:
-
In Ireland, the share of international medical students has been growing rapidly and accounted for half of all medical students in the academic year 2017/18 (Box 2.1) (Health Education Authority, 2018b[2]).
-
In Romania, the number of international students has grown rapidly since 2007 and has been estimated to reach nearly 30% of all medical students in 2018/19, based on the number of places in medical schools in English- and French-language programmes (see Figure 6.2 in chapter 6).
-
Poland has also become an increasingly popular destination for international medical students over the past two decades, accounting for a quarter of all medical students in 2017/18 (Ministry of Health of the Republic of Poland, 2017).
-
In Australia, the number of international students has also grown over the past decade to reach 2 668 students in 2017, accounting for 16% of all medical students in that year (Australian Government Department of Health, 2019[3]).
-
France has a long tradition of hosting a substantial number of international medical students with the overall number of students in undergraduate and postgraduate medical education totalling about 12 000 in 2017/18, although this number has come down over the past decade (Table 2.2 in Box 2.1).
The movement of international medical students increasingly occurs inside the OECD and EU area, rather than from non-OECD or EU countries to the OECD or EU area. For example, the most numerous groups of international medical students in Ireland and Poland come from other OECD countries, including Canada, Norway, Sweden, and the United States. In France, while many international medical students still come from Maghreb countries, the share of students coming from other OECD and European countries has been on the rise, accounting for more than a third of all international students in 2017/18.
Over the past two decades, thousands of Norwegian and Swedish students have enrolled in English-language medical education programmes in Central and Eastern European countries – with Poland becoming the most popular choice (Box 2.2). The number of Norwegian students pursuing their initial medical education outside their home country during the academic year 2017/18 was almost as large as those pursuing their studies in Norway (Norwegian State Educational Loan Fund, 2018[4]).
Ireland
All Irish medical schools have a large number of international students (Table 2.1). The biggest group among these international students are Canadian students (28% or 993), followed by students from Malaysia (18% or 667) and Kuwait (7% or 250).
Poland
Foreign students accounted for 25% (6 759 out of 26 381) of all full-time medical students in Polish medical schools in 2017/18 (Ministry of Health, 2018). Data from six of the biggest medical schools show that the majority of these students come from Norway, Sweden, Saudi Arabia, the United States and Canada.
Australia
The number of international students graduating from Australia’s medical schools increased by more than 40% between 2007 and 2017 (from 316 to 450). In 2017, 2 668 international students were enrolled in medical schools in Australia, accounting for 16% of total enrolments (Australian Government Department of Health, 2019[3]).
France
The number of international medical students in France remains substantial with around 12 000 students enrolled in 2017/18, but it has decreased by around 20% since 2010/11, now accounting for less than 9% of all students. One-third of these students came from Algeria, Morocco, and Tunisia, although their share has decreased in recent years. The second largest and growing group come from other EU countries (Table 2.2).
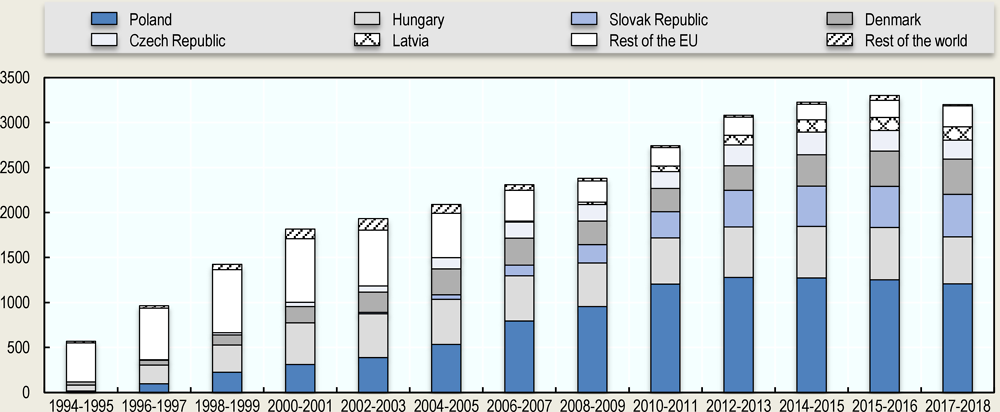
Over the past two decades, the number of Norwegian students studying medicine outside their country rose by about 40%. In 2017/18, over 80% of them were studying in Central and Eastern European countries, with the greatest number studying in Poland (Figure 2.1). The number in Poland increased strongly during the 2000s and has remained fairly stable at around 1 200 since 2010.
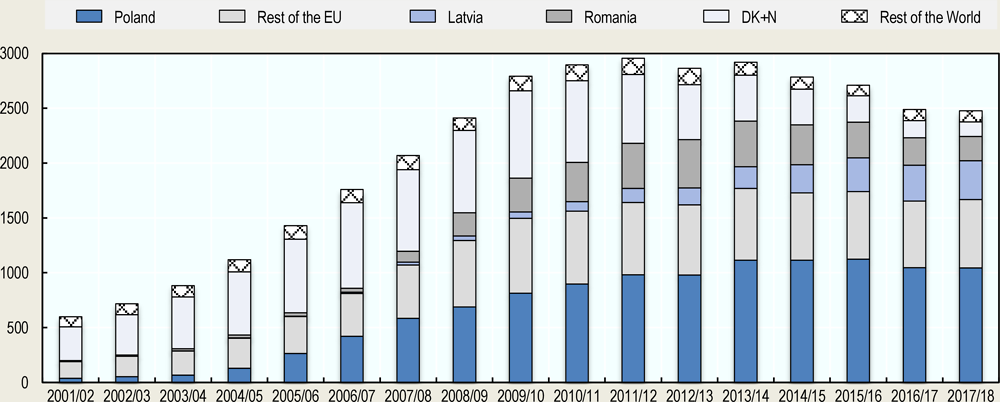
Similarly, the number of Swedes pursuing medical studies abroad has increased greatly between 2001/02 and 2011/12 to reach a peak of about 3 000, after which the number has decreased to about 2 500 in 2017/18 (Figure 2.2). Poland is also the main destination, attracting over 40% (or 1 044) of the students in 2017/18. The second and third most popular destinations in 2017/18 are Latvia (14% or 354) and Romania (9% or 222), respectively (Swedish Board of Student Finance, 2018).
Additional information can be derived from the countries where the international medical graduates are pursuing their postgraduate specialty training and practice. Data from the United States and France, for example, show that a growing share of foreign-trained doctors are in fact people born in these countries, who completed their first medical degree abroad before returning to their home country:
-
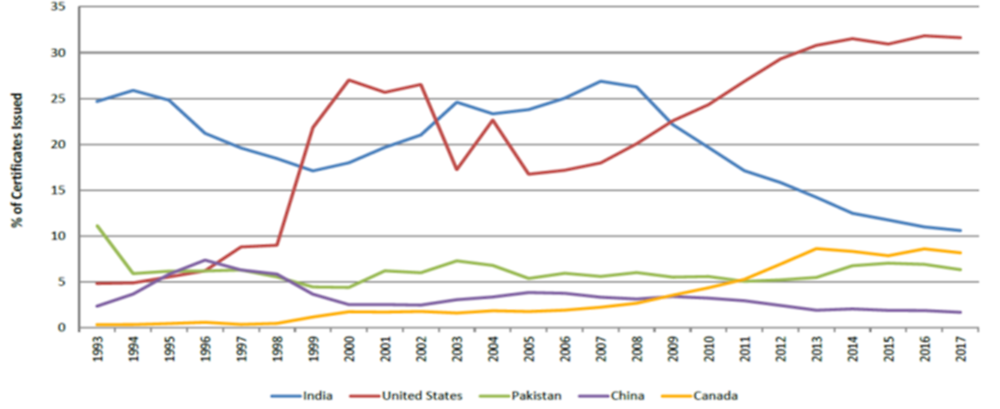
In the United States, a growing share of international medical graduates are American citizens who studied mostly in the Caribbean before coming back to the United States (Figure 2.3). In 2017, American citizens were by far the most numerous group (more than 30%) of international graduates who obtained certification in the United States (up from 17% in 2007). American graduates trained abroad have largely replaced Indian graduates coming to the United States.
-
In France, among all international medical graduates attending the exam for entry into postgraduate training in 2017, the largest group was, in fact, made up by French citizens (133 out of 328) who obtained their first medical degree in another EU country.2 Romania was the country of education for the vast majority of them (110 out of the 133).
The case of Ireland illustrates another layer of complexity in the international mobility of medical students and graduates. In 2016, medical graduates from four Asian and African countries – India, Nigeria, Pakistan, and Sudan – accounted for over a quarter (28%) of all junior doctors seeking or having a postgraduate training place in Ireland. However, a significant share of these medical graduates did not complete their first medical degree in their home country or in Ireland, but rather in a Central and Eastern European country before going to Ireland (Table 2.3). This was the case for many Indian junior doctors who graduated from medical schools in Bulgaria and Romania before moving to Ireland. Similarly, almost half of the Nigerian junior doctors graduated from medical schools in Hungary, Romania, and Poland, with only around 40% of them obtaining their diploma from Nigerian medical schools (Royal College of Surgeons in Ireland, 2018[6]).
In summary, the profile of international medical students and foreign-trained doctors is changing. An increasing share of them is made up of students from OECD countries who complete their first medical degree outside their home country with the intention to return there to take up postgraduate training and practice as a doctor. One of the implications of this growing movement is that the full medical education and training process increasingly takes place in more than one country, with the first (more theoretical) medical degree being obtained in one country and the second step (more practical and clinical) internship and the subsequent postgraduate specialty training being carried out in another. This may cause some planning issues and create some bottlenecks for students as they wish to move from the first medical degree to postgraduate training if not enough places are available (see also Section 2.4). Another relatively new phenomenon is that migrant doctors born in some Asian and African countries (such as India or Nigeria), which are traditionally perceived as net exporters of medical practitioners, often complete their medical education in OECD or other European countries, most likely with the intention to get access to labour markets in the OECD or EU area.
2.3. A number of “push” and “pull” factors drive student mobility
Studying medicine abroad is not a new phenomenon, but the factors driving the international mobility and composition of international medical students have changed.
Traditionally, international medical students studying in OECD and other EU countries were coming mainly from countries that did not have a sufficient capacity to train doctors (often through bilateral agreements). Over the past 15 years, a number of factors have contributed to a growth in the internationalisation of the medical education, though. These factors include the reduction of barriers to the mobility of students through the recognition of qualifications – especially within the EU/EFTA area –, active recruitment strategies of medical schools in some countries to attract more international students, and the numerus clausus policies in many countries that continue to provide incentives to study abroad for students not admitted in their home country.
The largest groups of international medical students in Ireland, Poland, and Romania (coming mainly from countries like Canada, France, Norway, and Sweden) decide to study abroad because of the limits on the intake of medical students in their home countries, even in those cases where they have to pay higher tuition fees themselves (Table 2.4).
Even for the students from Norway and Sweden, two countries where all students are eligible for scholarships even if they decide to study outside their country, these subsidies are not sufficient to cover all the tuition fees and cost of living to pursue their studies in other EU/EFTA countries like Poland or Romania, since the foreign-language programmes in the latter countries are more expensive. These students may get additional government loans from their own country, which they will need to pay back once they have completed their studies. Many North American international medical students also fund their studies through government loans that they will have to pay back. Only some students from Malaysia receive analogous loans to study in Ireland, with most of them having to pay upfront all of their studies through private funding (own/family savings).
The international mobility of students has also been supported by deliberate strategies of medical schools in some countries to attract more international students. These strategies have included developing medical education programmes in English and French to reduce language barriers, developing agreements with other (non-EU/EFTA) countries on the recognition of diplomas and qualifications, and the active recruitment of students through agents representing schools in selected foreign countries.
International students are an additional source of funding for the medical schools through tuition fees they pay, which are either higher than the tuition fees for the domestic students or from which the domestic students are exempt (Table 2.4, Box 2.3). In Ireland, medical schools can more or less flexibly expand the intake of international students (while the intake of national students remains subject to a numerus clausus), while in Poland, the Ministry of Education in co-operation with the Ministry of Health set the maximum number of admissions to all study programmes. In Romania, the expansion in the number of international students is subject to some external assessment of the medical schools’ teaching capacity, with an increase in international students being compensated by a decrease in the number of Romanian students.
Tuition fees paid by international students are an alternative source of funding for the medical schools in Poland, Romania, and Ireland.
Medical schools in Poland and Romania estimate that the tuition fees paid by international students are close to the marginal cost of education for each additional student, and the remaining funds are used to offer extra pay to the staff involved in international study programmes, usually in the form of paid over-time. In Poland, the average cost of medical education in 2016 was estimated to be around 10 500 USD per student (Ministry of Health of the Republic of Poland, 2016), which is slightly less than the tuition fees paid by students in the English programme. The additional revenues brought by international students are part of the schools’ efforts to attract and/or retain qualified staff, thus addressing the emigration of medical personnel from Poland and Romania. In Romania, a part of these tuition fees is used to offer merit-based scholarships to some international students, thereby largely covering their tuition fees. At the Medical University in Cluj-Napoca (which has the largest number of students in the English and French programmes in the country), for example, around 20% of international students receive a scholarship.
In Ireland, the estimated unit cost of medical education is between approximately USD 120 000-144 000, depending on the duration of the studies (Campbell, 2015[7]). This is reflected in and consistent with the medical schools’ opinion that the cost of teaching a medical student is around USD 23 000 to 28 500 annually. Considering that on average the tuition fees paid by international medical students is around USD 56 000 (Table 2.4), representatives of the Irish medical schools recognise that international students subsidise the education of Irish students. They often express the concern that the medical schools would not be able to offer the high standards of education without these international students.
2.4. In some countries international medical graduates face a bottleneck in accessing postgraduate training required to become a doctor
The further training and career paths of international medical students are often not documented. Evidence from some countries such as Norway and Sweden indicates that most students from these countries who got their medical degree abroad manage to enter into postgraduate specialty training in their home country and then obtain the right to practice there. The access to postgraduate training positions in France for French and foreign students with a medical degree from another EU/EFTA country is also relatively easy, as all these students are allowed to go through the qualifying exam (the ECN) and will be offered an internship post, even if they get a very low mark at the exam. However, the post that they will be offered will often not be in the specialty or the region where they wanted to pursue their postgraduate training because the allocation is based on the ranking in the exam (i.e. students with the highest marks choose first) and students with a foreign degree generally end up having lower marks (see chapter 3).
On the other hand, a substantial number of students from other countries like Canada and the United States can face significant difficulties in accessing internship and postgraduate training either in the countries where they got their first medical degree or in their home countries, where they often want to pursue their career. If they cannot pursue their internship and postgraduate training, all their investment of financial as well as human capital in obtaining their first medical degree risks being wasted, as they will never become fully registered doctors.
In Ireland, the current selection procedure for entry into internship prioritises Irish (and other EU/EFTA) graduates of Irish medical schools3 (NDTP, 2018[8]). Therefore, the vast majority of international medical students in Ireland – coming from non-EU/EFTA countries such as Canada and Malaysia – will either need to go back to their home country or move to another country to find an internship and postgraduate specialty training post. Paradoxically, at the same time, Ireland struggles with shortages of doctors and recruits many foreign-trained doctors from other countries (see also chapter 4).
In Canada, most residency posts in the first step of the residency matching process are reserved for graduates from Canadian medical schools, with only a limited share opened for Canadian and foreign international medical graduates. The second step in this residency matching process, which is used to fill any unfilled positions, is more equally open to both Canadian and international medical graduates (CaRMS, 2019[9]). As a result, in 2018 and 2019, only about 20% of Canadian and foreign graduates with a medical degree obtained outside Canada and the United States managed to find a residency posts in Canada, about the same proportion as in 2010. This compares to around 95% for medical graduates who have obtained their degree in Canada (CaRMS, 2019[9]). This low success rate of Canadian international medical graduates might explain the increase in the number applying for postgraduate training in the United States in recent years (Figure 2.3).
In the United States also, international students face stiff competition in the residency matching process because the number of domestic and international applicants significantly exceeds the number of available residency positions, although the bottleneck is less severe than in Canada. The success rate in the residency matching process for both American and foreign international medical graduates was around 60% in 2019 (National Resident Matching Program, 2019[10]).
In Poland and Romania, all graduates of medical schools have equal access to medical internship and postgraduate specialty training (residency). However, the decisions on the number of available internship/residency posts have traditionally not taken into account the international students, based on the assumption that most of them will leave the country after obtaining their first medical degree; and this is indeed the case for the majority of international graduates of Polish and Romanian medical schools who are not pursuing further training in these countries because they consider the working conditions to be relatively poor.
2.5. The international mobility of students brings additional challenges to national health workforce planning and policies
The growing international mobility of medical students is not always taken into account in national health workforce planning, either in the countries where they pursue their medical studies or in their countries of origin.
Since the majority of international students enrolled in medical schools in Poland and Romania return to their home countries or move to third countries upon completing their first medical degree, they are not accounted for in the planning of the domestic supply of doctors. However, there is a potential risk in these countries that a number of domestic students may be squeezed out, as medical schools might be tempted to give preference to international students who generate higher revenues through higher tuition fees. In Poland, the expansion of places for international students has been much more moderate than the expansion of places for domestic students. The opposite has happened in Romania, where the decisions on the intake of domestic and international students are almost entirely left to the medical schools. If the demand for doctors increases in Romania in the years ahead, the pool of Romanian medical graduates may not be sufficient to respond to this demand.
In Ireland, the main stakeholders responsible for medical education and training are well aware of the current paradoxical situation whereby many international graduates of Irish medical schools are forced to leave Ireland in search for internship posts despite the fact that the country is struggling with a shortage of doctors and ends up recruiting many in other countries. The main factors contributing to the current bottlenecks in internship posts are, on the one hand, a limited consultant trainer capacity (which is related to doctor shortages) and, on the other hand, the failure to reconfigure the hospital system, which results in the maintenance of too many small hospitals that are not allowed to provide internship and specialty training.
In France, the Ministry of Health has started to take into account foreign-trained doctors in its health workforce planning and projections, without distinguishing between French students who completed their first medical degree abroad and others with a foreign degree. The most recent projection assumes that 1 500 foreign-trained doctors will come to France each year between 2015 and 2040), a number which is roughly equal to the inflow of foreign-trained doctors over the previous five years from 2010 to 2015 (Bachelet and Anguis, 2017[11]).
In Sweden, Swedish medical students studying outside the country are included in the national medical workforce planning, based on the assumption that they will all come back to complete their postgraduate training and work as doctors. Moreover, the 2012 modification of the regulations governing the practice of junior doctors streamlined the transition into training in Sweden for students who obtained their first medical degree in another EU/EFTA country (Swedish National Board of Health and Welfare, 2012[12]). Swedish medical students studying outside the country are therefore considered to be an attractive pool of medical practitioners for the Swedish health system, in addition to those who got their first medical degree in Sweden.
Also in Norway, the vast majority of Norwegian students who got a first medical degree abroad manage to complete their training and obtain the right to practice. The Norwegian government recently increased the numerus clausus on the number of students admitted in the Norwegian medical schools, which may reduce the number of Norwegians going to study abroad.
In summary, in some countries like Ireland, Poland, and Romania, international medical students are considered more as a source of additional funding for medical schools than an additional pool of physicians-in-training who would eventually become available for the country’s national health system. In other countries like Sweden and Norway that have maintained some fairly tight domestic numerus clausus policies while supporting domestic students to get a first medical degree abroad, the latter are included in the countries’ health workforce planning and are able to complete their postgraduate training when they come back. In yet other countries like Canada and the United States, a sizeable number of domestic students have gone to study medicine abroad, in most cases with the hope to return to their home country afterwards, but a substantial share of them have not been able to find a residency post at home to complete their clinical training, because the number of these posts has been significantly lower than the number of domestic and/or international applicants. This raises a potential risk of a waste in human capital if these international students are not able to complete their training.
2.6. Conclusions
The number of international medical students pursuing an education away from their home country has increased significantly over the past decade, now accounting for half of all medical students in Ireland, nearly a third in Romania, one-quarter in Poland, and around one in ten in France.
A number of factors have contributed to this internationalisation of medical education, including the reduction of barriers to the mobility of students through the recognition of qualifications especially when moving within the EU/EFTA area, the growing offer of international medical education programmes in some countries (particularly in some new EU member states), and the numerus clausus policies that limit entry into medical education programmes in many countries (or high tuition fees – for example, for American students). The movement of international medical students increasingly occurs also within the OECD and EU/EFTA area, with many students intending to return to their home country to practice as doctors.
The growing opportunities for students to study medicine abroad may allow them to fulfil their educational goals when they have not been admitted at home, while, at the same time, promoting fruitful international exchanges and experiences. However, the growing internationalisation of medical education may also entail some potential risks for these students, if they face difficulties in getting access to internship and postgraduate training posts and may also raise issues for national medical workforce planning and policies.
In countries that have been successful in attracting a large number of international medical students (such as Ireland, Poland, and Romania), medical schools benefit from, or might even have become dependent on, the tuition fees paid by these international students to retain their highly-skilled staff and to develop. However, a potential risk is that the increase in the number of international students might come at the expense of domestic students who may be squeezed out if the education capacity is limited. Given that domestic students are more likely to remain and practice as doctors in their country than international medical students, this could reduce the pool of domestic candidates available to respond to any increase in the demand for doctors. While this has not occurred in Poland, where the expansion of places for international students has been much more moderate than the expansion in the number of domestic students, the opposite has happened in Romania, where medical schools have more freedom regarding decisions on the intake of domestic and international students.
The international mobility of medical students may also raise issues of coordination between the first step in the medical education process (i.e. the obtention of a first medical degree) and the second step that is more oriented towards clinical training (i.e. the internship and postgraduate training period required to obtain the right to practice as a doctor). The growing number of international medical students can create pressures to increase further the number of internship and postgraduate training places to allow more graduates to complete their training, either in the countries where they have obtained their first medical degree or in their home countries. In countries where there are current or projected shortages of doctors, it may be desirable to increase the number of internship and postgraduate training places to respond to these needs, if sufficient training capacity can be mobilised. In countries where the number of domestically-trained doctors is expected to be sufficient to respond to future demands, increasing the training capacity may lead to surpluses.
For those international medical graduates who manage to find a postgraduate training place in their home country, which is the case for example for most Norwegian and Swedish students who studied abroad, this raises the issue of whether the access to the first phase of the medical education in these countries should not be opened up more by increasing the number of students admitted. This would have the advantage of treating more equitably those students who had to study abroad and paid higher tuition fees compared to those who were domestically-trained and paid much lower (or no) tuition fees.
The additional hurdles that international medical students can face in some countries in accessing internship and postgraduate training places might mean that some have to patch together their education in three or more countries or even work in non-training positions in the hope of finally becoming a fully-trained doctors. This may also result in “brain waste” if they are not able to complete their training in due time or at all to obtain the right to practise. In those countries that are providing government loans to students to study medicine abroad, there is also a need to ensure that these loans are wisely used.
Finally, the analysis illustrates important implications for the interpretation of the data on foreign-trained doctors, as it is increasingly important to recognise that not all foreign-trained doctors are non-native. In some countries (e.g. Norway, Sweden, and the United States) a large and growing number are students who obtained their first medical degree abroad before coming back to their home country to complete their training and work. In these cases, it is difficult to talk about a “brain drain” from the countries where they studied, particularly since in most cases these international students pay the full cost of their education abroad.
References
[3] Australian Government Department of Health (2019), Australian Government Department of Health, https://medicaldeans.org.au/data/.
[11] Bachelet, M. and M. Anguis (2017), Les médecins d’ici à 2040 : une population plus jeune, plus féminisée et plus souvent salariée.
[7] Campbell, T. (2015), Medical Workforce Analysis: Ireland and the European Union compared, Department of Public Expenditure and Reform (DPER).
[9] CaRMS (2019), Canadian Resident Matching Service, https://www.carms.ca/match/r-1-main-residency-match/ (accessed on 5 July 2019).
[2] Health Education Authority (2018b), HEA (2006-2016) student data, http://hea.ie/statistics-archiv (accessed on 2018).
[10] National Resident Matching Program (2019), Results and Data: 2019 Main Residency Match, National Resident Matching Program, https://mk0nrmpcikgb8jxyd19h.kinstacdn.com/wp-content/uploads/2019/04/NRMP-Results-and-Data-2019_04112019_final.pdf.
[8] NDTP (2018), National Doctors Training and Planning Unit Annual Report, NDTP - National Doctors Training and Planning Unit.
[4] Norwegian State Educational Loan Fund (2018), Norwegian State Educational Loan Fund.
[1] OECD (2018), Education at a Glance 2018: OECD Indicators, OECD Publishing, Paris, https://dx.doi.org/10.1787/eag-2018-en.
[5] OECD (2015), “Changing patterns in the international migration of doctors and nurses to OECD countries”, in International Migration Outlook 2015,, OECD Publishing, https://doi.org/10.1787/migr_outlook-2015-6-en.
[6] Royal College of Surgeons in Ireland (2018), Ireland’s international medical workforce: Analysis of linked medical council and medical employee databases.
[12] Swedish National Board of Health and Welfare (2012), Läkarstudenter från EU kan få vikariera i Sverige., http://www.socialstyrelsen.se/nyheter/2012juni/lakarstudenterfraneukanfavikarieraisverige.
Notes
← 1. The data cover all OECD countries except Canada, Italy, Japan, Slovenia, and the United Kingdom. The field of health includes medicine but also dental studies, pharmacy, nursing, and midwifery.
← 2. The other top nationalities among international medical graduates applying for a medical internship in France were students from Italy (122) and Romania (32).
← 3. The current intern-matching procedure prioritises those graduates of Irish medical schools who entered these schools through the Irish State’s Central Applications Office (CAO) admissions system, the majority of whom are Irish nationals. As a rule, foreign candidates enter the medical schools through separate channels.