Medical graduates
The number of new medical graduates is a key indicator to assess the number of new entrants into the medical profession; these will be available to replace doctors who will be retiring and to respond to any current or future expected shortages of doctors. The number of medical graduates in any given year reflects decisions made a few years earlier related to student admissions either through explicit numerus clausus policies (the setting of quotas on student admissions) or other decision-making processes, although graduation rates are also affected by student dropout rates.
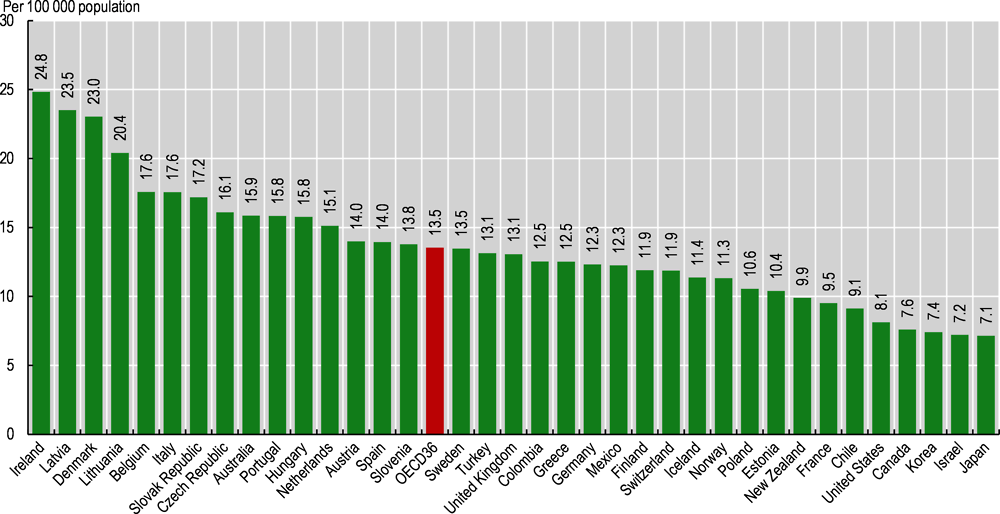
Overall, the number of medical graduates across OECD countries increased from 93 000 in 2000 to 114 000 in 2010 and to 149 000 in 2019. In 2019, the number of new medical graduates ranged from about seven per 100 000 population in Japan, Israel and Korea to more than 20 in Ireland, Denmark, Latvia and Lithuania (Figure 8.19).
In Ireland, the high number of medical graduates is to a large extent due to the large share of international medical students, who in recent years have made up about half of all students. Many students and graduates from Irish medical schools come from Canada, the United States and the United Kingdom, as well as other non-OECD countries. After obtaining their first medical degree, these international medical students in many cases leave Ireland – either because they prefer to complete their training and practise in their home country or because they have difficulty securing an internship. Paradoxically, this means that Ireland needs to import doctors trained in other countries to address doctor shortages (OECD, 2019[12]).
In other countries, the internationalisation of medical education is also reflected in a growing number of international medical students and graduates. Many medical schools in Poland, the Czech Republic and Hungary have attracted a growing number of international medical students, who in most cases do not plan to remain in the country after graduation. Polish medical schools, for example, offer medical studies in English, and 25% of all medical students are foreigners (OECD, 2019[12]).
In Israel, the low number of domestic medical graduates is compensated by the high number (about 60%) of foreign-trained doctors. A large share of these foreign-trained doctors are in fact Israeli-born people who have returned to Israel after completing their studies abroad because of the limited number of places in Israeli medical schools.
In contrast, Japan does not currently rely on foreign-trained doctors in any significant way (see indicator “International migration of doctors and nurses”). Japan has increased the number of students admitted to medical schools in recent years, which has resulted in some increase in the number of medical graduates.
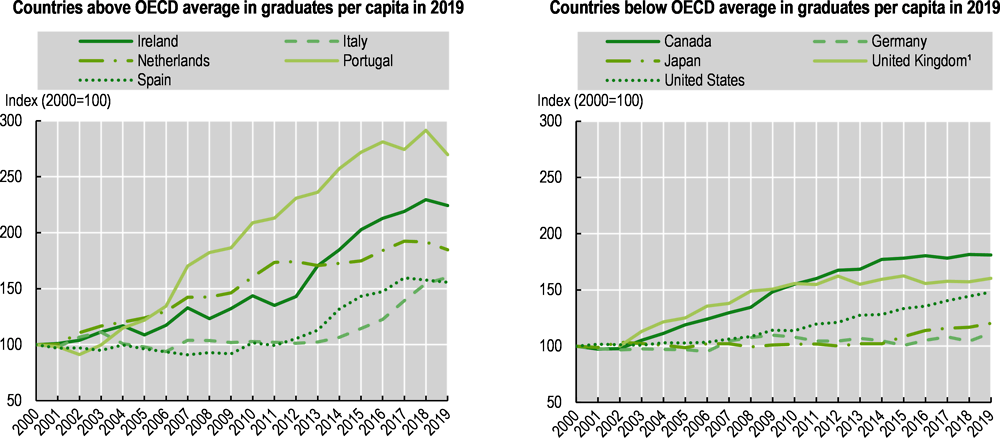
The number of new medical graduates per population has increased in all OECD countries since 2000 in response to concerns about current or future shortages of doctors, but with varying growth rates. Two-fold increases or more have occurred in several countries such as Portugal, Ireland and the Netherlands, while there has been a 50% increase in Italy, Spain and the United States (Figure 8.20).
In Portugal, the strong increase in the number of medical graduates since 2000 reflects both an increase in the number of places in existing universities and the creation of new medical schools outside Lisbon and Porto. The increase in the numerus clausus has been driven by concerns about doctor shortages, which is exacerbated by the uneven distribution of doctors across the country. However, the growing number of medical graduates in Portugal has raised concerns that this might result in bottlenecks, as not all new medical graduates may be able to find postgraduate specialty training places to complete their training immediately.
In the Netherlands, the number of students admitted to medical schools increased by 50% between 1999 and 2003 (from about 2 000 to 3 000 per year) in response also to concerns about doctor shortages, and it has remained at this higher level. In addition, a number of university medical centres allow students with a bachelor’s degree in certain other fields to enrol into a master’s degree in medicine, increasing the pool of students who can obtain a doctorate degree. In 2019, the Advisory Council on Medical Manpower Planning recommended that the intake of medical graduates in postgraduate training programmes should be increased in general medicine, geriatric medicine and occupational medicine, among other specialty areas (ACMMP, 2019[18]).
In Norway, a special commission appointed by the Ministry of Education and Research in 2019 recommended an increase in the number of training slots in medical schools of 69% by 2027 to ensure that 80% of doctors are trained domestically (Grimstad Commission, 2019[19]). As it stands, about 40% of all doctors are foreign-trained, including many Norwegian citizens returning to their home country following education abroad (see indicator “International migration of doctors and nurses”). This resulted in a 13% increase in the number of medical training slots in autumn 2020.