Overweight and obesity among adults
Being overweight, including pre-obesity and obesity, is a major risk factor for various non-communicable diseases including diabetes, cardiovascular diseases and certain cancers (OECD, 2019[28]). Overweight-related diseases are expected to cause life expectancy to decrease by 2.7 years on average in OECD countries over the next 30 years; they are also expected to give rise to treatment costs equivalent to 8.4% of health spending (OECD, 2019[28]). High consumption of calorie-dense food, trans-fats and saturated fats, and increasingly sedentary lifestyles have contributed to growing global obesity rates. High body mass index was estimated to cause 5 million deaths worldwide in 2019 (Institute for Health Metrics and Evaluation, 2020[36]). In addition, obesity puts people at increased risk of developing severe COVID-19 symptoms and of dying from COVID-19 (Katz, 2021[37]; Tartof et al., 2020[38]). Beyond health and medical conditions, obesity has wider social and economic impacts. Women and men with lower incomes are more likely to be obese, entrenching inequality. Individuals with at least one chronic disease associated with overweight are less likely to be employed; when they are at work, they are more likely to be absent or less productive than healthy individuals (OECD, 2019[28]).
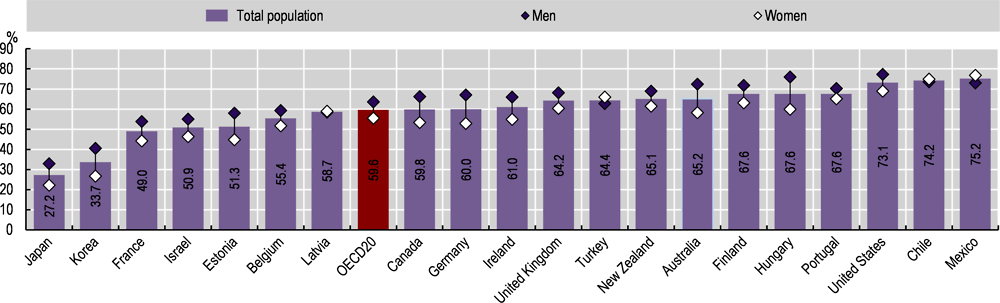
Measured height and weight data show that 60% of adults were overweight or obese in 2019, on average across 20 OECD countries with comparable data (Figure 4.15). In 17 of these 20 countries for which measured data is available, over half of the adult population was overweight or obese in 2019. For Mexico, Chile and the United States, this proportion exceeded 70%. Conversely, in Japan and Korea, fewer than 35% of adults were overweight or obese. Men were more likely than women to be overweight or obese in most countries, except in Chile, Latvia, Mexico and Turkey. The gender gap was relatively wide in Australia, Germany and Hungary (a difference of 14-16 percentage points).
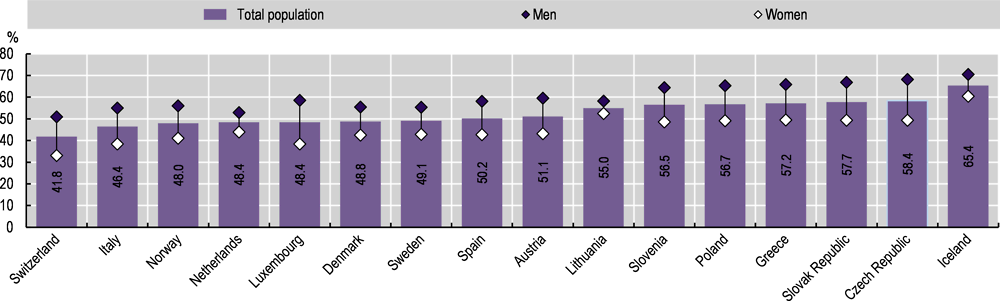
As an alternative to measured data, countries can monitor obesity using self-reported height and weight data. These estimates are less reliable, however, and are typically lower than those based on measured data. Across the 16 OECD countries for which measured data are not available, self-reported overweight (including obesity) rates ranged from 41.8% in Switzerland to 58.4% in Iceland in 2019 (Figure 4.16). As with measured data, men were more likely than women to be overweight or obese in all countries. The gender gap was relatively wide in the Czech Republic, Luxembourg, the Slovak Republic and Switzerland (a difference of 18-20 percentage points).
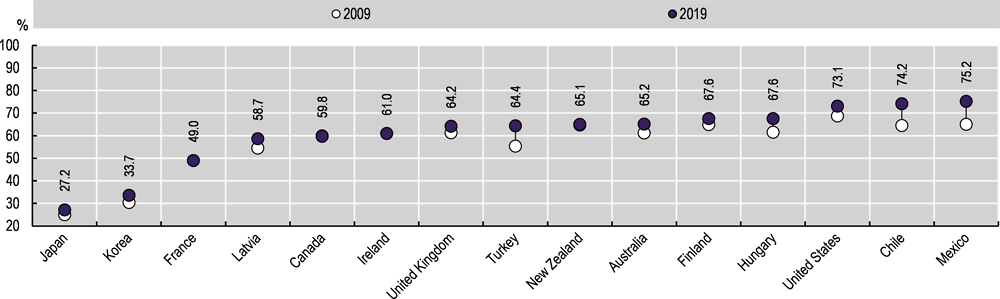
The proportion of overweight and obese adults increased between 2009 and 2019 in most OECD countries, including in countries where rates were relatively low (Figure 4.17), such as Japan, where it increased by 2.1 percentage points, and Korea, where it increased by 3.2 percentage points. In countries with relatively high rates of overweight and obese adults, the proportion also increased – including by 10.1 percentage points in Mexico, 9.7 percentage points in Chile, and 9 percentage points in Turkey. Overweight and obesity rates in Canada, France and Ireland remained stable between 2009 and 2019, and they increased at a relative lower pace in New Zealand.
OECD member countries have implemented a suite of regulatory and non-regulatory initiatives to reduce overweight population rates. Prominent examples include mass media campaigns to promote the benefits of healthy eating; promotion of nutritional education and skills; taxes on energy-dense food and drink items to discourage consumption; simplified food labelling to communicate nutritional value; and agreements with the food industry to improve the nutritional value of products. Promoting physical activity and reducing sedentary time also help to address the obesity problem. For instance, one-third of OECD countries have implemented prescription of physical activity by primary care doctors. Innovative initiatives of workplace programmes for wellness and reduced sedentary behaviour – such as in Japan and Ireland – can be found, although they are implemented relatively infrequently (OECD, 2019[28]).
Overweight is defined as abnormal or excessive accumulation of fat, which presents a risk to health. The most frequently used measure is body mass index (BMI), which is a single number that evaluates an individual’s weight in relation to height (dividing weight in kilograms by height in metres squared). Based on WHO classifications, adults over the age of 18 with a BMI greater than or equal to 25 are defined as pre-obese, and those with a BMI greater than or equal to 30 as obese. Data come from national sources – in a few instances these may differ from data shown in the OECD 2019 report on obesity, which uses data from the WHO Global Health Observatory, with age-standardised estimates and other methodological differences. Overweight includes both pre-obesity and obesity. The method for calculation of BMI is the same for men and women and for adults of all ages. BMI data can also be collected using self-reported estimates of body height and weight. BMI estimates based on self-reported data are typically lower and less reliable than those based on measured data.
This indicator reports on official statistics collected in the OECD Health Statistics 2021 database. For self-reported overweight (including obesity) rates, these statistics were complemented with the European Health Interview Survey wave 3 data (2019) for Denmark (latest data from 2017) and Poland (latest data from 2014).