Availability of doctors
Doctors and other health workers are crucial for addressing the health needs of the population in normal circumstances and even more so during exceptional circumstances such as the COVID-19 pandemic. Proper access to medical care requires a sufficient number of doctors, with a proper mix of generalists and specialists and a proper geographic distribution to serve the population in the whole country.
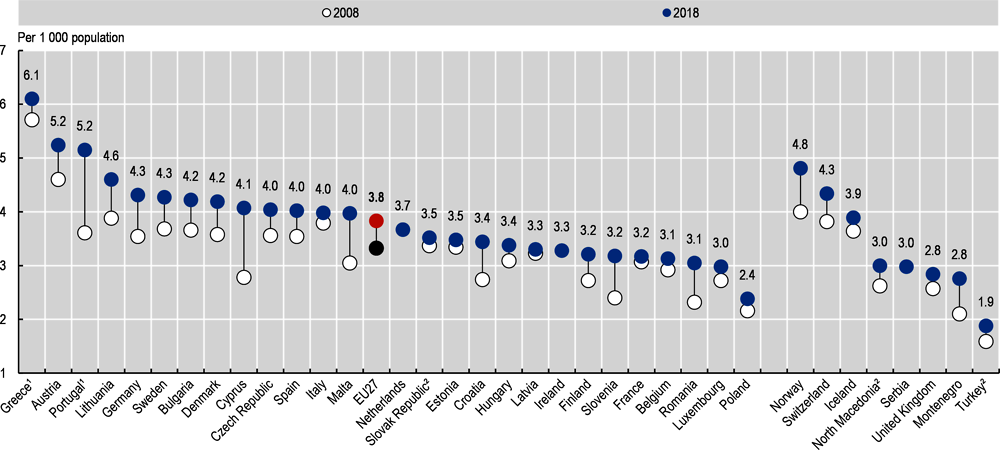
In 2018, Greece had the highest number of doctors with 6.1 per 1 000 population, but this number is an over-estimation as it includes all doctors licensed to practice (including retired physicians and those who might have emigrated to other countries). Austria and Portugal also had a high number of doctors per population, but the number in Portugal is also over-estimated for the same reason as in Greece (the number of practising doctors in Portugal is likely slightly below the EU average). On the other side of the spectrum, the number of doctors per capita was lowest in Poland, Luxembourg, Romania and Belgium (Figure 7.11).
Between 2008 and 2018, the number of doctors per capita increased in all EU countries, although the rise in France, Latvia, Estonia and the Slovak Republic has been very marginal. On average across EU countries, the number increased from 3.3 doctors per 1 000 population in 2008 to 3.8 in 2018, a growth of 15% taking into account the population increase.
There were a lot of concerns in the late 2000s about projected shortages of doctors arising from population ageing and the ageing of the medical workforce (OECD, 2008). These concerns prompted many EU countries to take actions to anticipate the retirement of a large number of doctors, notably by increasing the number of medical students, to replace those retiring (OECD, 2016). Several countries also took actions to postpone the retirement of current doctors and recruited more doctors from abroad (OECD, 2019a).
In many countries, the main concern has been about growing shortages of general practitioners, particularly in rural and remote regions. Whereas the overall number of doctors per capita has increased in nearly all countries, the share of general practitioners (GPs) has come down in most countries. On average across EU countries, only about one in five doctors were GPs in 2018 (Figure 7.12). Greece and Poland have the lowest share of GPs, while Portugal, Finland and Belgium have been able to maintain a better balance between GPs and specialists. Several countries have taken steps over the past decade to increase the number of postgraduate training places in general medicine. For example, in France, about 40% of all new postgraduate training places have been allocated to general medicine since 2017, a greater proportion than in most other EU countries. However, in France as in other countries, it remains a challenge to attract a sufficient number of medical students to fill the available training places, given the lower remuneration and perceived prestige of general practice (OECD/European Observatory of Health Systems and Policies, 2019).
The uneven geographic distribution of doctors and difficulties in recruiting and retaining doctors in remote and sparsely populated areas is another persisting challenge in many European countries. In all countries, the density of physicians is generally greater in urban regions, reflecting the concentration of specialised services such as surgery in urban centres as well as physicians’ preferences to live and practice in cities. Differences in the density of doctors between urban and rural regions are highest in the Slovak Republic, the Czech Republic and Greece (OECD, 2019b).
Many countries provide different types of financial and other incentives to attract and retain doctors in underserved areas, including one-time subsidies to help them set up their practice as well as recurrent payments such as income guarantees and bonus payments. A number of countries have also introduced measures to encourage students from underserved regions to enrol in medical schools (OECD, 2016).
Practising physicians are defined as doctors who are providing care for patients. In some countries, the numbers also include doctors working in administration, management, academic and research positions (“professionally active” physicians), adding another 5-10% of doctors. Greece and Portugal report all physicians entitled to practice, resulting in an even greater overestimation. In Belgium, a minimum threshold of activities (500 consultations per year) is set for general practitioners to be considered to be practising, resulting in an under-estimation compared with other countries that do not set such a threshold.
References
OECD (2008), The Looming Crisis in the Health Workforce: How Can OECD Countries Respond?, OECD Publishing, Paris, https://doi.org/10.1787/9789264050440-en.
OECD (2016), Health Workforce Policies in OECD Countries: Right Jobs, Right Skills, Right Places, OECD Publishing, Paris, https://doi.org/10.1787/9789264239517-en.
OECD (2019a), Recent trends in International Migration of Doctors, Nurses and Medical Students, OECD Publishing, Paris, https://doi.org/10.1787/5571ef48-en.
OECD (2019b), Health at a Glance 2019: OECD Indicators, OECD Publishing, Paris, https://doi.org/10.1787/4dd50c09-en.
OECD/European Observatory on Health Systems and Policies (2019), France: Country Health Profile 2019, State of Health in the EU, OECD Publishing, Paris/European Observatory on Health Systems and Policies, Brussels, https://doi.org/10.1787/d74dbbda-en.