4. Health promotion and vaccination
Improving population health prior to a health shock, through health promotion and vaccination in primary health care, is critical to improve health system preparedness and resilience. Not only primary health care (PHC) is key to maximise population health prior to a shock, but it also plays a central role during a health emergency to contain the spread of infection. New PHC developments have been implemented by LAC-7 countries to mitigate the COVID-19 pandemic, including informing the community on prevention measures, reaching-out to high-risk population, or facilitating the roll-out of COVID-19 vaccination. However, there is scope to strengthen public health activities into primary health care in LAC-7 countries, such as improving the collection of health information and increasing the level of professionalisation of community health workers. Further, the COVID-19 pandemic had dramatic impact on routine vaccination programme, which urgently calls for sustained catching-up programmes.
Improving population health (both physical and mental health) prior to a health shock is critical to improve health system preparedness to deal with emerging pathogens or health shocks such as COVID-19. This was one major lesson from the COVID-19 pandemic, as obesity and chronic diseases were shown to be risk factors for severe COVID-19 cases and death. In addition to improving population health, primary health care with a strong community-based approach is best placed to carry-out several public health activities during health emergencies including for example disseminating public health information, risk factor monitoring, epidemiological surveillance, and implementing vaccination roll-out. These are all critical activities, that when integrated into primary health care, help health systems to improve their resilience to a health shock, by increasing their ability to absorb and recover from a shock.
Providing an effective response for COVID-19 has represented a major challenge for health systems across the OECD and LAC countries. However, LAC-7 countries particularly faced several vulnerabilities during the COVID-19 pandemic, mostly due to lack of resources, fragmented health systems, socio-economic inequalities, and sometimes poor governance of the public health crisis. In some instances, countries have been making efforts to improve the effectiveness of COVID-19 response through a greater emphasis on the role of primary health care. Countries with well-established networks of primary care centres and community health workers implemented primary health care policies and actions to contain the spread of the pandemic and absorb its impact.
This chapter starts analysing primary health care performance before COVID-19 on health promotion and routine vaccination in LAC-7 countries, highlighting wide differences across the region in the promotion of child and maternal health, counselling for risk factors, and routine vaccination programmes. The chapter then discusses the importance of integrated public health activities into primary health care to monitor population health and carrying-out public health surveillance in LAC-7 countries. Finally, the chapter analyses the public health activities that have been scaled up into the primary health care in LAC-7 countries during the COVID-19 pandemic, focussing for example on informing and educating the community, identifying, and reaching out to high-risk population, or implementing COVID-19 vaccination. Evidence on the dramatic impact of COVID-19 on routine vaccination is also presented.
Inequalities in access to maternal health remain in LAC-7 countries
In LAC-7 countries, the promotion of child and maternal health is an important challenge. Around one-third of the deaths in the first year of life occur during the neonatal period, and conditions like pneumonia are amongst the leading infectious causes of childhood morbidity and mortality (PAHO, 2017[1]). Effective health systems can greatly limit the number of infant deaths, particularly by addressing life-threatening issues during the neonatal and childhood period. Basic care for infants and children includes promoting and supporting early and exclusive breastfeeding, identifying conditions requiring additional care, and counselling on when to take an infant or young child to a health facility (Tomczyk, McCracken and Contreras, 2019[2]).
The paediatrician is a highly skilled and qualified supervisor of paediatric primary health care (PPHC) team which is responsible for providing additional care and counselling to families, while limiting care fragmentation thanks to its holistic medical approach (Boudreau et al., 2022[3]). The PPHC can for example promote infant care through breastfeeding counselling to contribute to a healthy growth and decrease rates of stunting and obesity (Victora et al., 2016[4]). Nutritional counselling in primary health care is also important to make sure infants receive nutritionally adequate and safe complementary foods, while continuing breastfeeding up to two years of age and even beyond (UNICEF, 2021[5]).
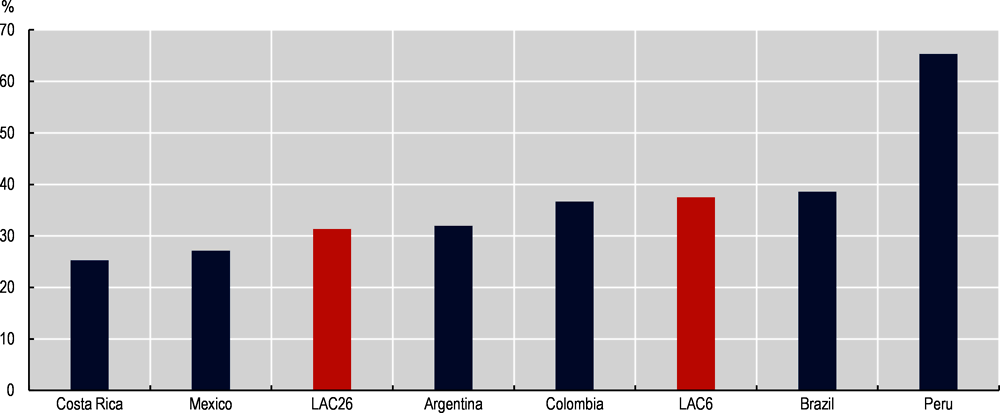
International figures show that Peru, with a rate of children exclusively breastfed during their first six months of life over 60%, is well above the averages of the region. In Brazil, Colombia and Argentina, around one in three infants under six months of age are being exclusively breastfed (close to the LAC-6 average), while both Mexico and Costa Rica exhibit rates below 30% (see Figure 4.1).
For children aged six months and older, Argentina and Brazil have a rate of over 90% for diets including any solid, semi-solid, and soft foods, while in Mexico this figure is just above 80%. In addition, over six out of ten children in Peru had continued being breastfed at age two; however, this only applies for less than three out of ten children in Brazil (see Figure 4.2).
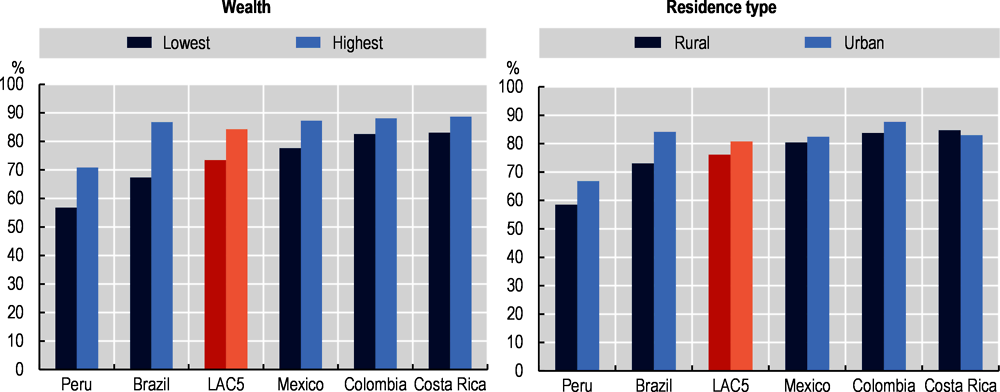
When it comes to birth control, more than 200 million women of reproductive age in developing countries are estimated to not be using a modern contraceptive method even if they want to avoid pregnancy (WHO, 2018[9]). Sexual and reproductive health and rights are closely linked to gender equality and women’s well-being: it affects newborn, child, adolescent, and maternal health, in addition to their capacity to determine future economic development and environmental sustainability (Starrs et al., 2018[10]). Family planning significantly reduces child and maternal mortality and morbidity, making it one of the most cost-effective public health measures (UNFPA, 2018[11]). It should be a key dimension of reproductive and sexual health services in both high-income and low-income countries (UNFPA, 2018[11]). However, there are signs of large inequalities in access to contraceptive prevalence across socio-economic characteristics in most LAC-7 countries. While PHC is well involved in the reproductive health agenda in Mexico (Box 4.1), contraceptive prevalence is 20% lower amongst people in the lowest income groups when compared to those in the highest income levels (see Figure 4.3). Colombia and Costa Rica have attained contraceptive prevalence levels of over 70% in urban areas as well as amongst the highest income levels, while values are slightly lower for those living in rural areas or with the lowest income. By contrast, the contraceptive prevalence is relatively low in Argentina (below 60%) regardless of residence type or income level.
There are also wide disparities across socio-economic groups in access to family planning in favour to people living in urban areas or those with higher income (Figure 4.4). Countries with higher access to family planning (such as Costa Rica, Colombia and Mexico) show narrower gaps between residence type or income level than in countries with lower access to family planning (Peru and Brazil) (see Figure 4.4). Access to family planning is 29% and 25% higher amongst high income groups than lower income groups in Brazil and Peru, respectively.
The reproductive health agenda includes policies and reproductive PHC services on adolescent health. The National Strategy to Prevent Teen Pregnancy comprises six components: (1) inclusive, integrated, and flexible education; (2) comprehensive education in sexuality; (3) employment opportunities for adolescents; (4) enabling environment; (5) comprehensive health services; and (6) early detection and care for girls, boys, and adolescents affected by sexual violence.
As part of the reproductive health agenda, social workers, family medicine nurses and public health staff in PHC facilities inform and educate adolescents on contraceptives and sexually transmitted diseases, provide contraceptives, and follow up of contraceptive users.
Additionally, IMSS-Bienestar implements the Rural Adolescent Care Centres programme (Centros de Atención Rural al Adolescente, CARAS) in rural areas. This programme provides reproductive counselling, contraceptives, and health promotion. IMSS-Bienestar estimates that CARAS averted 37 000 unintended adolescent pregnancies in 2019 (IMSS, 2020[12]).
Source: Secretaría de Salud (2020[13]) IMSS (2020[12]), http://www.imss.gob.mx/prensa/archivo/202003/120, Consejo Nacional de Población (2019[14]), https://www.gob.mx/cms/uploads/attachment/file/559766/informe2019-enapea.pdf.
There is scope to increase counselling in primary health care for risk factors to health
Beyond child and maternal health, PHC teams play a key role in improving population health by influencing patients’ lifestyles and providing appropriate guidance to avoid negative consequences of unhealthy lifestyle. An extensive body of literature demonstrate the effectiveness of interventions implemented in primary health care settings to address risk factors to health such as heavy drinking, unhealthy eating, or physical inactivity (Jané-Llopis et al., 2020[15]; OECD, 2022[16]).
However, available evidence suggests low levels of engagement from primary care physicians with patients’ lifestyles in some LAC-7 countries (Guanais and et al., 2018[17]). Counselling on healthy lifestyle is rarely implemented in the delivery of PHC services in Brazil, Colombia and Mexico. Only 24.3% of respondents in Brazil, 23.6% in Colombia, and 40.9% in Mexico indicated that the primary care physician discussed issues related to healthy lifestyles, such as diet, physical activity, and stress factors. In all three countries, a clear difference between public, private, and uninsured PCP’s willingness to discuss healthy lifestyles with patients was observed, with higher levels in the private sector. As public provider in LAC generally serve lower-income households, this further highlight how social inequality is also reflected on the access and quality of care being provided in the region.
Programmes based in primary health care that measure the alcohol consumption of adult patients and give brief advice to heavy drinkers have been found effective in reducing alcohol consumption. Results from meta-analyses of several studies suggest a reduction in alcohol consumption of almost 12%. However, most implementation has been undertaken in high-income countries. Only recently, a PHC-based measurement, advice, and treatment plan for heavy drinking and comorbid depression is being implemented at municipal level in Colombia, Mexico and Peru (SCALA Programme) (Jané-Llopis et al., 2020[15]). While there is no evidence on the impact of this programme yet, there are several success factors that will bring many beneficial impacts. These include training approaches for a range of health care professionals, and municipal-based adoption and support mechanisms for joined-up action to improve health literacy. Such brief alcohol interventions in primary health care are implemented in several OECD countries, including Canada, the Czech Republic and Germany (OECD, 2022[18]).
There are also interesting examples across other OECD countries where primary health care plays a key role to encourage healthy eating and active lifestyles (OECD, 2022[18]). In Sweden for example, primary health care physicians write individualised prescriptions for physical activity to patients, with follow-up meeting to adjust the prescription and foster motivation as part of the programme called “Physical Activity on Prescription” (PAP). OECD analyses show that the PAP programme is a cost-effective, evidence-based intervention which can help increase physical activity, prevent disease, and reduce the health care expenditure. In 2019, 45 000 prescriptions for physical activity were prescribed in primary health care in Sweden, equating to approximately 14.1 prescriptions per 1 000 eligible people. According to OECD analyses, the current implementation of PAP in Sweden is estimated to result in a cumulative total gain of 737 life years (LY) and 979 disability-adjusted life years (DALYs) by 2050. In the Netherlands, Combined Lifestyle Intervention (CLI) are offered to patients with overweight of other risk factors. The CLI provides dietary advice, physical activity training, and counselling on behavioural change over a period of two years. Participants are referred by their general practitioner (GP) to a local CLI provider. These include physiotherapists, lifestyle coaches, and dieticians – either working individually or in a group. Around 18 000 people have participated in CLI since its inception in 2019. According to OECD simulations, CLI would lead to 12 565 life years (LYs) and 16 704 disability-adjusted life years (DALYs) gained by 2050 in the Netherlands. By 2050, CLI will accumulate health expenditure savings equivalent to EUR 11.2 per person in the Netherlands.
Given the increasing prevalence of risk factors to health and the rising burden of chronic non-communicable conditions in LAC-7 countries (see Chapter 3), more efforts are needed to provide proactive and preventive care notably through health counselling and patient education. This would certainly require investments in training for primary care workers (see Chapter 7), as well as a better knowledge of local health needs. Already in Chile, primary care practices are key actors in health promotion activities, for instance through the Vida Sana counselling and physical activity programme. The programme is run from primary health care by physicians, dieticians, psychologists, and physical therapists (see Box 4.2). The Vida Sana counselling and physical activity programme in Chile is a best practice example across the OECD from which other LAC-7 countries could learn.
The Vida Sana counselling and physical activity programme has been part of the national prevention package in Chile since 2014. To date, there are about 300 teams delivering this intervention throughout Chile. This one-year programme aims to improve physical activity and diet in patients with obesity or overweight patients with other risk factors. Participants receive individual and group counselling sessions with nutritionists and psychologists. To contain the delivery cost, medical doctors are only involved if the patient specifically requires medical attention in case of diseases. In addition, patients complete 144 hours of physical activity in classes guided by a physical education teacher, physical activity therapist, or kinesiologist. While the sessions take place in primary care centres, the programme is completely independent and run by dedicated counsellors.
Source: OECD (2019[19]), OECD Reviews of Public Health: Chile: A Healthier Tomorrow, https://doi.org/10.1787/9789264309593-en.
LAC-7 countries have effective vaccination programmes, with coverage rates close to other OECD countries
The World Health Organization (WHO) has estimated that vaccination can prevent between two and 3 million deaths per year worldwide from 20 life-threatening diseases, plus an additional 1.5 million deaths that could be spared thanks to global vaccination and the prevention of the spread of disease to unvaccinated individuals. Childhood vaccination programmes are one of the most effective health policy interventions, both in clinical efficiency and in cost-effectiveness, and frequently take up a significant share of national prevention strategies (Chan et al., 2017[20]).
Vaccination programmes are well in place all over LAC countries, including routine vaccination (i.e. diphtheria, tetanus toxoid, and pertussis – DTP3 – and measles) as well as additional vaccines (i.e. pneumococcus, rotavirus, and human papilloma virus). They are included at national or subnational level based on local morbidity, mortality, and cost-effectiveness analysis (OECD/The World Bank, 2020[21]).
International figures show that Costa Rica and Chile reached higher vaccination rates than the OECD average for DTP3 and measles for children aged one (around 95%). Similarly, Colombia has been able to achieve a high coverage of immunisation against measles and a DTP3 vaccination rate that is close to the OECD average. At the other end of the scale, Mexico is yet to achieve a high vaccination rate against measles (at 73% in 2019), while the same is true for Brazil on DTP3 immunisation coverage (at 70% in 2019) (Figure 4.5).
Nevertheless, barriers to vaccination still exist in the region. Contextual influences -such as lower socio-economic status and residence type – were amongst the most relevant, as well as individual and group influences such as a general mistrust in the health system or personal beliefs and attitudes (Guzman-Holst et al., 2020[24]). Policies aimed at increasing public confidence in the safety and efficacy of vaccines, through scientific knowledge for example, are an evidence-based tool that LAC-7 countries should better use to enhance vaccination strategies.
Vaccination coverage for measles and DTP3 is consistently higher amongst people with higher income in LAC-7 countries with available data. Brazil exhibits the largest gaps in vaccination coverage between high- and low-income groups (see Figure 4.6). Vaccination coverage for Measles and DTP3, respectively, is 16% and 25% higher amongst high income groups than low-income groups in Brazil.
Another vaccine-preventable disease, Influenza, is annually responsible for 3 to 5 million severe cases worldwide, along with up to 650 000 deaths (WHO, 2019[25]). Adults aged 65 and over are at greater risk of developing serious complications from this infectious disease, including pneumonia and sepsis, which can result in serious illness or death. The WHO recommends that 75% of older people should be vaccinated against seasonal influenza. Remarkably, vaccination rates against influenza for adults aged 65 and over in some LAC-7 countries are higher than the OECD average. This is the case in Chile and Mexico, with vaccination rates of over 80%, well above the OECD average of 45% (OECD, 2022[22]).
A high degree of integration between primary care and public health is needed to ensure delivery of health promotion activities
Integration of public health in primary health care promotes greater efficiency and effectiveness of health care services to improve population health. It yields substantial benefits to patients and wider population. There are several ways to promote greater integration, including for example bringing clinical and community-based professional into multi-disciplinary team, sharing population-based information on health risks and health problems, and using population-based programmes to strengthen health promotion and direct patients to medical care (Rechel, 2020[26]). Successful integration in part relates to systemic factors such as government strategies to bridges disciplines, appropriate programmes, and policies. In Costa Rica and Mexico, endorsement of integration by government has helped to improve integration between primary health care and public health.
Costa Rica has made public health central to the delivery of medical care. In fact, there is a high degree of integration between public health and primary health care since the 1994 reforms which transferred responsibility for the provision of all public health, preventive, and curative services from the Ministry of Health to the Social Security agency (Caja Costarricense de Seguro Social, CCSS). The overarching objective was to have one agency responsible for both organising preventive and curative services as well as making sure that neither preventive nor curative services overshadowed the other in the multidisciplinary primary health care team. In addition, shared value and long belief in the value of community-based approach for health promotion and disease prevention is an important factor driving to successful integration between public health and primary health care. It helps the team members to collaborate and provide a wide range of services such as education for individuals on how to maintain sanitation and hygiene to avoid disease spread, to conducting exams and tracking medical records (VanderZanden et al., 2021[27]).
Mexico also has a robust platform for ensuring such public health functions. The Undersecretariat of Prevention and Health Promotion (Subsecretaría de Prevención y Promoción de la Salud, SPPS) under the Mexican Government is responsible for developing, implementing, and evaluating public health policies through specific plans and programmes within the health sector. Ministry of Health clinics, health posts, and mobile services, as well as social security family medicine clinics and IMSS-Bienestar clinics deliver outpatient and community outreach public health services. For instance, PHC facilities with 10-19 doctor’s offices are expected to have a public health area staffed with public health nurses, community health workers (CHWs), and one epidemiologist. Those with 20 or more doctor’s offices should have two epidemiologists and a larger public health staff (IMSS, 2000[28]; Secretaría de Salud, 2010[29]).
Across the OECD, few countries have achieved high level of integration between primary health care and public health. Slovenia is a notable exception, where primary health care centres provide comprehensive care to its population, including health promotion, treatment, and response to emergency situations such as natural disasters and the COVID-19 pandemic. In fact, since 2004 each primary health care centre comprises a health promotion centre to enable a multi-disciplinary team to provide health promotion, counselling, group interventions to support heathier lifestyles for patients, and immunisation. Multi-disciplinary teams comprise nurses, physiotherapists, psychologists, and dieticians. Patients can attend individual and group classes on lifestyle changes regarding health nutrition, physical activity and mental health, smoking, and alcohol use (OECD/European Observatory on Health Systems and Policies, 2021[30]; WHO, 2018[31]). Health promotion action groups are also established to help identify and include hard-to-reach populations, such as those unemployed, Roma, and people with mental health problems.
Fostering linkages between public health and primary care is key to deliver a wide range of public health activities including community engagement, health promotion, health education, and immunisation. As the next sections emphasises, public health workers (such as community health workers) and use of electronic health records in primary health care settings are successful factors towards delivery of these activities.
Community health workers play a crucial role to undertake public health surveillance, but higher level of professionalisation is warranted
There is growing attention towards the important role played by community health workers (CHWs) to deliver essential public health services in the primary health care sector including public health surveillance, patient education, and assistance with navigating the health system. This is even more relevant given the global health workforce shortage estimated to be 65 million by 2030 (WHO, 2022[32]), and the emphasis on strengthening primary health care system to deliver more and better services.
CHWs are frontline public health workers, often members of the communities in which they work. They have valuable knowledge of people needs, local health beliefs, and are a trustful source of information. They promote health, reduce inequality, and improve public health by carrying out several activities ranging from community education, health counselling, social support, monitoring health status and risk factors to health, linking with health care systems (WHO, 2020[33]). In most cases, they oversee home visits, and at the clinic or health posts, they can organise appointments for other health workers and offer education and counselling sessions. In some countries, CHWs have also a role in collecting and reporting information on the health status of people in the community.
Available evidence shows that CHWs have a positive impact on disease prevention, healthy behaviour, and access to care. CHWs have been found effective in reducing neonatal mortality and child mortality attributable to pneumonia (Pallas et al., 2013[34]). The most recent systematic review suggests that most articles found evidence of programme effectiveness (for example on improving immunisation uptake, breastfeeding, and improving child health) and on cost effectiveness (for example on HIV) (WHO, 2020[33]). Amongst the selected LAC-7 countries, Brazil, Costa Rica and Peru are countries with a strong focus on CHWs to provide health promotion, disease prevention, and health surveillance, while in Argentina, Chile, Colombia and Mexico their roles and functions are relatively less defined.
In Brazil, there are approximately 370 000 CHWs in 2020. They are responsible for education, health promotion, maintaining patient records, making regular house-calls, monitoring vaccination uptake, and providing referrals. CHWs have played a critical role to mitigate the impact of infectious diseases such as seasonal dengue in deprived communities (Neto et al., 2021[35]) and of Zika virus (Nunes, 2020[36]). During the Zika epidemic for example, CHWs promoted healthier living environment by informing people and community on how to prevent Zika virus circulation, disseminating important information on symptoms and vector control, and carrying-out incidence reporting. This was done through door-to-door household visits, identifying buildings, trashes where mosquitoes could reproduce, or other mosquito “hot-spots”. CHWs’ roles and responsibilities in collecting information were critical to identify population at risk, deploy response teams, and influence individual behaviour (Nunes, 2020[36]). Available evidence highlights that, in many remote and vulnerable municipalities, CHWs are not equipped with mobile phones and tablet computers to enable remote diagnoses and real time communication with the PHC facilities (Wadge et al., 2016[37]).
CHWs in Costa Rica have a high level of professionalisation with in-depth training and are well equipped with digital technologies. Multidisciplinary EBAIS teams (providing comprehensive and co-ordinated primary care) comprise an Asistente técnico de atención primaria or ATAP (a CHW named as a technical assistant) in addition to a physician, a nurse, and a medical clerk (named registros y estadísticas de la salud) (VanderZanden et al., 2021[27]; Pesec et al., 2017[38]). The technical assistant is responsible for health promotion activities, disease prevention, epidemiological data collection, basic sanitation activities, identification of disease risk factors, and referrals to EBAIS physicians or hospitals. During home visits, technical assistants collect data in the Ficha Familiar, including anthropometric measurements, vital signs, and home safety and sanitation, as well as conduct health education, and identify familial, behavioural, and environmental risk factors (Pesec et al., 2017[38]). They also organise information and education programme in community settings such as churches, schools, or town centres.
Peru also has a long tradition of work with CWH, who carried out voluntary actions related to health promotion and disease prevention. In 2020, there were 4 449 community health agents which are called Promotores de Salud. They have traditionally played a crucial role in the promotion of health at the community level to reduce mortality amongst children under the age of five through the Integrated Management of Childhood Illnesses. This programme incorporated family and community practices to promote infant and child health through community education, home-based care, and referrals.
In Argentina, Chile, Colombia and Mexico, there is scope to better define the roles and functions of CHWs. This calls for education and training programmes to professionalise CHWs and support implementation of new health promotion programmes towards increasing risk factors to health and public health surveillance. Key examples for learning are available internationally, such as in the United States, where States have developed CHWs’ training and curriculums at academic institutions (Box 4.3). Maintaining competences through continuing education to make sure CHWs acquire new skills throughout their carriers is also critical to ensure they can manage evolving and growing health needs (RHIhub, 2020[39]).
In the United States, many States offer CHWs training and curriculums at academic institutions. The content and organisation of the curriculum vary depending on local specificity and community health needs. Curriculums may address, amongst others, the following topics (RHIhub, 2020[39]):
Source: RHIhub (2020[39]), Community health Worker Curriculums; https://www.ruralhealthinfo.org/toolkits/community-health-workers/4/training/curriculum.
Few LAC-7 countries use EHR to encourage primary health care teams to engage in health monitoring and disease surveillance
Electronic Health Records (EHRs) is a key tool to provide a good understanding of the health status of the population. It allows to collect and analyse data for public health purposes and to disseminate public health information to assess and respond to public health problems (Aliabadi, Sheikhtaheri and Ansari, 2020[40]). Both high- and low-income countries are moving away from traditional disease surveillance system – such as manual reporting – to use EHR to identify new risk factors, analyse targeted interventions and assess outcomes at the individual and population levels. Available evidence shows that the use of EHR allows better surveillance of infectious and non-infectious diseases, enables to identify populations with high risk factors, and leads to improved management of patients with chronic diseases (see also Chapter 6) (Kruse et al., 2018[41]). During a pandemic, quick access to patient information and risk factors to health allows to identify and monitor those in high-risk groups and aggregate data at community level to make decisions about public health (CGI.br, 2020[42]).
Amongst the selected LAC-7 countries, few countries have implemented EHR in primary health care facilities. In Costa Rica and Chile more than 80% of primary health care practices use EHRs. It facilitates the delivery of comprehensive and continuous primary care, while contributing to monitor and improve population health by generating alerts or reminders to guide the primary health care workers in real time in their counselling and diagnosis.
In Costa Rica, the CCSS has developed the Unified Digital Health Record (Expediente Digital Único en Salud – EDUS) which is used by all primary health care teams. EDUS make patient charts to function as clinical guides and to create reminders for primary health care providers. This helps to keep track of individual patient history (for example on vaccination records) and risk factors for health, and to track community determinants of health. In addition, a medical data clerk (called Registros de Salud – REDES) completes patient intake and epidemiological surveillance. REDES help register patients and keep detailed records on a range of health quality metrics. All the data is funnelled up to the health area and to the national level, but it is also used at the local level by EBAIS teams to make improvement plans or to carry out targeted actions. EDUS is used across all CCSS network of health care facilities (clinics, hospitals and EBAIS), patients’ data can be consulted by any centre on real time, which helps to assure continuity of care.
In Chile, PHC teams have relatively up-to-date information about the main health risks of the population living in the geographic area of their catchment territory (municipality). Access to individual data is heterogeneous since it is dependent on EHR use and its adherence by individual providers. Unpublished data from the MoH estimated that in 2018, 85% of all primary health care centres are using EHRs (Meza, Vargas and Barros Rubio, 2019[43]).
In Brazil, an estimated 78% of PHC units had EHR systems in 2019, and around one in four PHC units still maintained clinical records and patient data in paper format only (CGI.br, 2020[42]). There are also wide disparities across regions: in 2019 adoption of EHR systems was higher in the South and Southeast regions (at 90% and 83% of facilities in those regions, respectively) compared to the Northeast and North regions (77% and 74%, respectively).
At the lower end of the scale are Argentina, Mexico, Peru, and Colombia, where electronic health records are underused for disease surveillance, notably because of a relatively low penetration amongst primary health care physician – at 17%, 50%, and 36%, respectively (Figure 4.7) (Global Health Intelligence, 2017[44]). However, Colombia has introduced in 2020 a nationwide EHR. The Ministry of Health and Social Protection will regulate the data that will be interoperable in the early stages of project development.
In Mexico, the first electronic health records in PHC facilities were introduced in 2003 by IMSS as a part of the family medicine improvement initiative. Currently, the fragmented public health sector has 65 different EHR systems that vary in content, information sources, and human resource capacity to manage them. This situation negatively affects reliability and information sharing for disease surveillance. The homologation of EHR systems amongst health institutions and training health and IT staff are critical to overcome the existing barriers (The Competitive Intelligence Unit, 2020[45]).
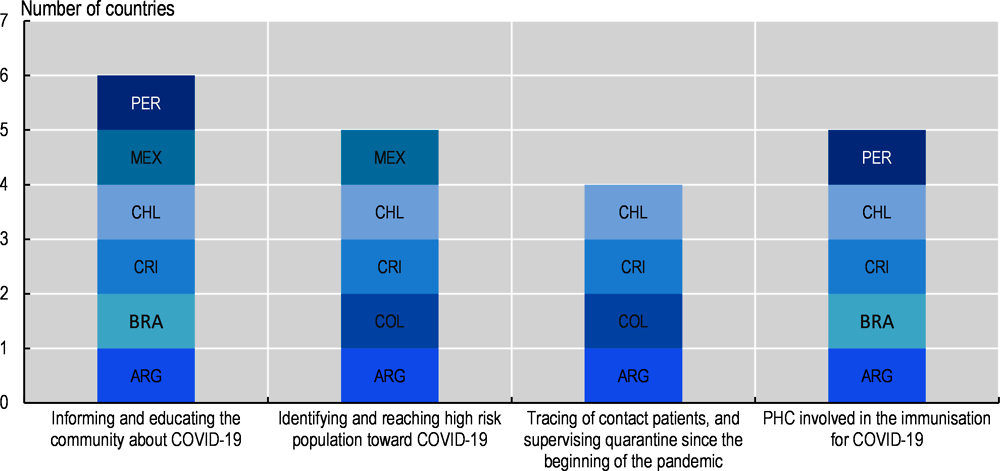
International learning from OECD and LAC-7 countries during the pandemic indicates that countries with stronger primary health care system have shown greater preparedness and resilience. In Costa Rica, for example, ATAPS have performed a broad range of public health functions to meet the needs of people and communities. By contrast, in Colombia and Mexico primary health care had too often limited involvement in public health activities to respond to COVID-19 (see Figure 4.8). This section presents the role of PHC across the LAC-7 countries, and highlights innovative local practices, in the following five dimensions of the COVID-19 pandemic: 1. informing and educating the community about COVID-19; 2. identifying and reaching high-risk population; 3. tracing contact patients and supervising quarantine; 4. roll-out of COVID-19 immunisation. The last section provide evidence of disruption in health promotion activities and vaccination during the COVID-19 pandemic.
PHC has created awareness on COVID-19 risks, and tailored messages and information campaigns
The lack of information on the pathogen, how the SARS-CoV-2 was more likely transmitted, and its effects on the health of the population (with the subsequent debates on vaccine safety and proper therapies to treat the infection) was one important challenge at the beginning of the pandemic in all countries. Risk communication from authorities in several OECD and LAC-7 countries has often been conflicting and confusing for the population. Effective communication to the public is essential to support the population to understand containment and mitigation measures, and act upon them effectively. In some instances, LAC-7 countries have used primary health care to create awareness on COVID-19 risks and tailor messages and information campaigns on non-pharmaceutical intervention (such as facemask use or social distancing).
In Peru, for example, the Health Promotion Direction of the Peruvian MoH organised over 6.4 000 anti-COVID-19 Community Committees with more than 40 000 community health agents, whose general objective is to contribute to the reduction of the transmission of COVID-19 via their mobilisation in the territory. These efforts were based on the long tradition in Peru of work with community health agents in co-ordination with health personnel even before the COVID-19 pandemic started (MinSa Peru, 2020[48]). Similarly, certain provinces of Argentina have prioritised the PHC approach to provide sufficient information to patients and communities on information and health education to patients on prevention of infection. For example, the province of Misiones has trained health promoters who carried out actions for facemask use, social distancing, and hygiene measures during the pandemic. In Chile, health teams delivered educational activities about COVID-19 at PHC centres. Brazil has provided training and guidelines for CHWs following the Ordinance GM/MSn°3.241/2020 to increase their capacity to provide education and information on COVID-19 to the community.
In Colombia, the role of primary health care to provide information and health education to patients and communities on prevention of infection was limited. Rather, community leaders received training on risk communication that allowed them to inform communities on the COVID-19 pandemic and how to prevent the spread of the virus. Key messages on COVID-19 were also disseminated to indigenous communities in the Wayúunaiki language, as a joint effort by the local authorities in the department of La Guajira with the support from the Pan-American Health Organization (ReliefWeb/WHO, 2020[49]).
Some good examples of effective communication to populations and communities and dissemination of public health messages on infection prevention and control measures by primary health care can be found in other OECD countries. In Australia, primary health care workers have had a key role in reaching and supporting vulnerable community members throughout the COVID-19 pandemic. They have ongoing trusting relationships with many people in their local community and are well placed to provide information about COVID-19 in response to individual concerns and needs. Another initiative has involved members of an immigrant community working directly with health workers from that community and government staff to co-design approaches to education and vaccination that were appropriate to their culture. Younger members of the community have been engaged via social media, including Facebook, Zoom, Instagram, and WhatsApp. In the United States also, CHWs have provided accessible and culturally appropriate information and education on COVID-19 through programmes such as the New York State’s Maternal and Infant Community Health Collaborative Initiative (MICHC). This approach, specifically targeted to vulnerable communities, has contributed to the reduction of racial, ethnic, economic, and geographic disparities (Rahman, Ross and Pinto, 2021[50]).
Several PHC actions have been implemented in LAC-7 countries to identify and reach out high-risk population
COVID-19 is known to affect more severely elderly population, those suffering from underlying health conditions (such as obesity, cancer, hypertension, diabetes, and chronic obstructive pulmonary disorder), people living in more deprived areas, as well as low-income groups or indigenous population (Katz, 2021[51]; OECD, 2021[52]). For example, at the beginning of the COVID-19 crisis, patients aged 60 and over represented over 93% of deaths – while this figure was of 58% amongst people aged 80 or older- across 21 OECD countries with comparable data one year after the onset of the pandemic (OECD, 2021[52]). While the LAC countries have a relatively younger population than OECD countries (see Chapter 3), it is critical to proactively identify and engage with these high-risk individuals. The examination of policies and practices across LAC-7 countries shows that some developments and innovations were introduced.
In Argentina, the Ministry of Health and the health authorities from provinces implemented actions to identify, locate, and classify more than 4 000 public and private long term care residences to quickly respond in case of a rapid rise of COVID-19 infections. In addition, the long-term care workers were trained in infection and prevention protocols, while contingency plans were prepared to tackle the COVID-19 crisis. In addition, the Sumar Programme incentivised the active identification of people aged 64 and older without formal health coverage; and even though various sources of information were integrated at the provincial level for the identification of this population, the role of PHC teams in their identification was important through field activities. In Chile, primary health care worked in close co-operation with the social sector to provide support to the elderly. During the COVID-19 pandemic, PHC workers delivered food and milk from the National Food Programme to the elderly.
Other LAC-7 countries, including for example Costa Rica and Mexico, focussed on reaching-out to underserved communities. Costa Rica adopted technical guidelines for COVID-19 prevention in indigenous territories. These included the promotion of community participation, the integration of indigenous health knowledge, as well as communication and prevention actions. In addition, a multidisciplinary team of women was formed that includes the presence of indigenous leaders to work closely with communities (FILAC, 2020[53]) (MinSa Costa Rica, 2020[54]). Similarly, Mexican health authorities focused on people living in remote and marginal urban areas by implementing and deploying community health promotion brigades, epidemiological brigades, and clinical care units with PHC providers. This programme was first applied in the states of Sonora, Coahuila, Yucatán and Tabasco by the Mexican MoH and with the support of the National Institute of Public Health. Health promotion brigades are composed of at least two health promoters. The work programme is planned and co-ordinated with the directors from the PHC unit (Secretaría de Salud de México, 2020[55]; Secretaría de Salud de México, 2021[56]), including:
Analyse the COVID-19 risk factors profile from the population (provided by the local health unit), update this information through home visits and phone surveys.
Perform a general questionnaire and respiratory exam to refer them to the health unit, after being contacted by the specialised health brigade (which will also receive the information collected on household visit and phone survey).
Educate patients and communities on measures to contain the risk of infection (e.g. hand washing techniques, social distancing, recommendations to follow on public spaces), and main symptoms and risk factors related to COVID-19.
Ensure other health promotion activities beyond COVID-19 in accordance with the local population needs. Checks are made on national health cards to verify if children vaccination is up to date (emphasis on DTP3 and DT for adults – informs PHC unit on residents that require vaccination) and rehydration care for parents with children under the age of five (serums are distributed).
Manage pregnant women attending antenatal care and conduct risk assessments in pregnant women. Collect phone numbers from an adult in the household as a focal point for PHC unit contact with that family.
Perform and distribute gender-focused and culturally sensitive informative material on COVID-19 and other health issues elaborated by state-level health authorities.
There are other good examples across OECD countries, for example in Türkiye, where family physicians gave telephone counselling to older patients with chronic diseases (Kumpunen et al., 2021[57]). Similarly, in Finland and the United Kingdom all people using long-term care services were identified as vulnerable during the pandemic and were proactively offered PHC services (Kumpunen et al., 2021[57]). Such proactive policies help to quickly deploy extra support for those most in need.
COVID-19 surveillance, contact tracing, and quarantine supervision were lacking in several LAC-7 countries
An effective strategy that tests, tracks people infected, and traces their contacts (TTT) is needed to limit the number of COVID-19 cases and, subsequently, deaths. This strategy encompasses the ability of public health authorities to effectively trace contact patients and supervise quarantines. It is especially applicable in the initial phases when the transmission is yet on a scale that is containable. A systematic review assessed the effectiveness of contact tracing, quarantine, and isolation strategies in the prevention and control of COVID-19. From the 22 selected studies consisting of observational and modelling studies, results show that these strategies were independently effective. However, the effectiveness and efficiency were shown to be further increased if implemented in a timely manner during the health emergency and when coverage is large (Tadele Girum, 2020[58]).
In Argentina, CHWs played a leading role in follow-up COVID-19 and tracing of close contacts, through the DETECTAR programme. This programme is based on door-to-door visits to people with symptoms and those that have been in close contacts with confirmed COVID-19 cases, with results integrated to the National Health Surveillance System (SNVS) which reported all COVID-19 cases. Vulnerable communities and areas with outbreaks are the focus of DETECTAR with a team of between 15 and 45 people. Personnel from this programme not only takes people body temperature and check for other symptoms of the disease, but they also give guidance on COVID-19 prevention. When a potential case is signalled, the person is referred to a triage centre, in which a team composed of different health workers interview and collect their personal data before performing a test in a mobile health facility close to the triage centre (see also Chapter 5) (PAHO, 2020[59])
Colombia established a programme for testing, tracing, and isolation of contacts of probable or suspected cases of COVID-19. The programme, called PRASS (Pruebas, Rastreo y Aislamiento Selectivo Sostenible), has been quickly implemented during the first phase of the pandemic, guiding teams responsible for this activity. Implementation of tracing and tracking teams and procedures is the responsibility of local health secretariats, health promotion entities (EPS), the National Tracking Contact Centre, National Institute of Health (INS), and health provider institutes (IPS). PRASS teams are interdisciplinary groups, for example, an IPS team may include administrative personnel that co-ordinates activities, and nurses or clinical support personnel trained in telephone and face-to-face tracking, evaluation, and follow-up of confirmed or suspected COVID-19 cases and their contacts (MinSalud Colombia, 2020[60]).
In Brazil, Peru, Chile and Mexico, the surveillance system was not appropriate to implement effective tracing mechanism. In Peru, the strengthening of COVID-19 surveillance and diagnosis activities in the onset of the pandemic were carried out through temporary intervention teams (called emergency response teams) for diagnosis and clinical follow-up that responded to local health authorities and that were not linked to PHC. The Integral Intervention Teams (IIT), and the primary health care teams that work in COVID-19 facilities, started to use SICOVID (integrated system for COVID-19) for reports after the initial phase of the pandemic (MINSA, 2020[61]). In Chile, the public health surveillance system, EPIVIGILA, was supposed to work in real-time regarding infectious diseases notification -either confirmed or probable cases. However, the high demand on health care overloaded the system during the beginning of the pandemic, effectively delaying data registration in EPIVIGILA. At first, the surveillance system only allowed the registration of a limited number of contacts, and it lacked the necessary data fields for tracing COVID-19 cases efficiently. Furthermore, EPIVIGILA is not interoperable with EHR in primary care or with the National Registry of Immunisations, making difficult the disease outbreak response. At local level, the Centinela strategy implemented in the Renca municipality in Chile was successful by improving epidemiological surveillance and conduct testing and tracing activities (see Chapter 5).
Similarly, at the beginning of the COVID-19 pandemic in Mexico, health authorities adhered to a sample-based sentinel surveillance model to monitor the pandemic, analysing and reporting laboratory samples of only 10% of suspected COVID-19 cases with mild symptoms, 100% of suspected patients with severe symptoms, and 100% of cases meeting the definition for severe acute respiratory infection (Secretaría de Salud de México, 2021[62]; Sánchez-Talanquer, González-Pier and Sepúlveda, 2021[63]). This limited testing hindered detection and tracing, affecting adequate quarantine measures, and contributing to the spread of SARS-CoV-2.
Adequate surveillance systems are key during infectious diseases outbreaks. However, for a region such as LAC that has experienced previous health emergencies, like the AH1N1 pandemic in 2009, and that is highly exposed to other infectious diseases such as Zika virus, malaria, or yellow fever, surveillance systems should be highly improved and broadened, as well as rely more on the involvement of PHC teams to enhance surveillance capacity (see Box 4.4).
Having real-time data on outbreaks, collected for example by PHC centres or teams, could help prevent clusters and save lives by acting before community spread starts or goes exponential. In addition, establishing regional bodies to allow for the sharing of these data between countries could also help control outbreaks that may occur in areas close to national borders. Some good examples of initiatives to strengthen surveillance system at primary health care level and to implement tracing strategies can be found across other OECD countries. France for example used a sentinel network implemented by PHC physicians. The network was supported by a specific application integrated into the information system of primary health care facilities. The purpose of this application was to allow for case reporting, surveillance protocols, and COVID-19 case descriptions (Prado et al., 2021[64]). In Luxembourg, an effective contact tracing system was set up to identify contacts, administer quarantine and isolation, and manage clusters of infection (OECD, 2022[65]). The contact tracing team comprised 200 people, and the system provided positive results. The time between identification of laboratory confirmed cases and notification was generally 24-48 hours, and it provided personalised support.
2009 AH1N1 pandemic in Mexico and LAC
Latin America and the Caribbean has not been exempted from previous epidemics and outbreaks, whether they be human-to-human infectious diseases or vector-borne diseases. For example, the 2009 pandemic of the infectious respiratory disease produced by the influenza A virus subtype H1N1 greatly affected the LAC region.
On a country-specific case, Mexico began preparing a National Influenza Preparedness Plan (NIPP) shortly after the SARS 2003 epidemic emerged in Asia. Completed in 2005, this plan was already being tested at a national level by 2006. In the absence of LAC regional health mechanisms, Mexico’s NIPP was complemented with the North American Plan for Avian and Pandemic Influenza developed by the governments of Canada, Mexico, and the United States. This national plan allowed Mexico to face the 2009 AH1N1 pandemic with stockpiles of strategic medicines and personal protective equipment (PPEs), pre-tested risk communication campaigns, and networks to distribute vaccines more efficiently. Nevertheless, the preparedness for intensive care units beds, ventilators, and the number of qualified personnel to use these tools were not sufficient, as has been the case during the COVID-19 pandemic.
Many lessons that ought to have been learned from the 2009 AH1N1 pandemic were not applied consistently not only in Mexico but also in most of LAC. We can cite for example the late involvement of the highest-level authorities, who generally convened after the arrival of SARS-CoV-2 to the region and therefore delayed inter-sectoral readiness. In addition, the slow reaction to acquire strategic medical resources such as PPEs, drugs, and laboratory supplies allowed regions affected before LAC to exponentially increase their demand for these goods, thus distorting global markets and making these medical supplies scarcer and more expensive, hindering the capacity of LAC countries to face the COVID-19 pandemic.
Epidemiological surveillance: the 2015-16 Zika virus outbreaks in the northeast of Brazil
The northeast of Brazil has experienced significant Zika virus outbreaks, which included cases associated with microcephaly and other birth defects. During certain peaks, more than 200 000 cases were reported in Brazil (by the end of 2016), having the highest number of cases worldwide as well as the most cases associated with birth defects (2 366). To track the evolution of this outbreak, a genomic and epidemiological surveillance effort was undertaken.
The ZiBRA mobile genomics laboratory screened 1 330 samples from patients in 82 municipalities across the federal states of Alagoas, Bahia, Paraiba, Pernambuco and Rio Grande do Norte, with the support of the MoH and other institutions. The samples that were provided by public health laboratories and the Fundação Oswaldo Cruz (FIOCRUZ) were screened for the presence of Zika virus using real-time quantitative PCR tests. The analyses undertaken with these samples allowed to estimate that Zika virus was present in northeast Brazil by early 2014 and was likely to have spread from there to other areas of Brazil and the rest of LAC.
Source: Di Paolantonio (2020[66]), https://www.oecd.org/about/civil-society/youth/Shaping-the-Covid-19-Recovery-Ideas-from-OECD-s-Generation-Y-and-Z.pdf; Córdova-Villalobos (2017[67]), http://www.anmm.org.mx/GMM/2017/n1/GMM_153_2017_1_102-110.pdf; Hernández-Ávila (2020[68]) https://doi.org/10.1177/0840470420921542; Faria et al. (2017[69]), https://doi.org/10.1038/nature22401; Giovanetti et al. (2020[70]), https://doi.org/10.1016/j.celrep.2020.01.085.
Procurement issues delayed the capacity of PHC to facilitate the roll-out of COVID-19 vaccination in LAC-7 countries
A watershed moment in the COVID-19 pandemic was the rollout of COVID-19 vaccines that started in late 2020 (OECD, 2021[71]). Nevertheless, LAC, as other developing regions in the world, suffered from a lack of access to vaccines and then had difficulties to administer vaccines to their population mainly due to logistics and misinformation.
As a response to procurement issues, LAC-7 countries heavily relied on the COVID-19 Vaccines Global Access (COVAX) mechanism to ensure access to COVID-19 vaccines. COVAX is a global initiative led by the World Health Organization (WHO) that aims to promote vaccine equity worldwide; all countries in the LAC region have joined this effort except for Cuba, which relies on domestically produced vaccines only. Participation in COVAX is done in two ways: self-funded countries (paying for their vaccines purchased through the mechanism at market price) and low-income countries (EU-LAC-Foundation, 2021[72])
PHC is key to undertake swift and maintained community health efforts that can address a sound COVID-19 recovery through the implementation of COVID-19 vaccine distribution (Wilkinson et al., 2021[73]). Having a long history of delivering vaccination programmes, primary care teams are uniquely placed to facilitate uptake and delivery of COVID-19 vaccines in the community, including for people living in deprived, rural, and remote areas. Knowledge about medical and personal information of the local population, and long-time relationship with patients are key elements for successful and personalised vaccination roll-out (Pinaka et al., 2021[74]; Lewis, Nuzum and Schneider, 2021[75]) (Chiolero, 2021[76]).
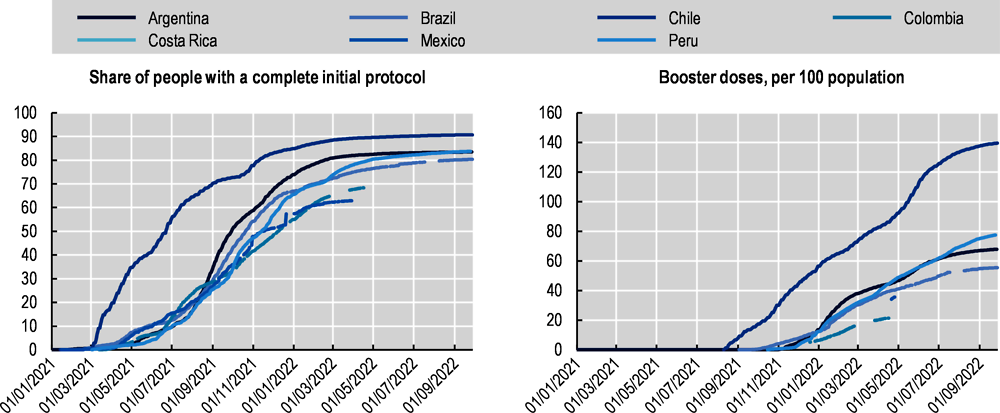
With these regards, Chile out-performs other countries in the LAC region (see Figure 4.9). The country’s success in the administration of COVID-19 vaccines relates to a robust health care delivery system built long before COVID-19 hit, but also to an early strategic purchasing of vaccine doses (Aguilera et al., 2021[77]; Castillo, Villalobos Dintrans and Maddaleno, 2021[78]). In addition, the Chilean Ministry of Health set new regulations to prepare the COVID-19 immunisation programme, strengthened the infrastructure for safe storage and distribution of vaccines, and set up personnel training to guarantee the quality, safety, and access to vaccines. Nurses, doctors, or a trained health care technician can carry out vaccinations; however, other health professionals such as psychologists, medical technologists, dentists, midwives, and pharmacists could do so under the emergency state. In addition, the MoH and municipalities implemented mobile posts to facilitate geographical access to vaccines. During the COVID-19 campaign, the country added 1 800 new vaccination points over the regular vaccination sites for seasonal campaigns such as influenza (Aguilera et al., 2021[77]). New vaccination points were profusely publicised in national and local media outlets, and the MoH website published information about COVID-19 vaccines and practical details about the immunisation campaign (#YoMeVacuno). The Salud Responde hotline oversaw answering the population’s questions and doubts about vaccines and the immunisation process.
As in Chile, primary health care facilitated the implementation of COVID-19 vaccine distribution in Argentina, Peru, Brazil and Costa Rica:
In Argentina the COVID-19 vaccination strategy was initially based on the co-ordination, communication, and participation mechanisms of the Provincial Immunisation Programmes, with progressive involvement of PHC teams. In addition, some health centres raised awareness about the importance of the vaccine by offering virtual counselling and services and sending out communications to those who may be hesitant or lack access to health care services (promujer health centre). There are also good local initiatives, such as in the province of La Rioja, which carried-out actions to ensure the COVID-19 vaccination of the population. Influenza immunisation was also ensured for adults aged 65 and over either at home or at collection points. Strategic points were then established for the COVID-19 vaccination of adults, pregnant women, and patients at risk inside their cars, called Operativo Vacunauto. In addition, the health agents of the entire capital, together with the EOC (Emergency Operations Committee) teams, carried out the COVID-19 vaccination of those people with incomplete immunisation schedules, or who did not have access to the vaccine.
In Peru, physicians and nurses made assessments to people before the administration of the vaccines; but only nurses were allowed to administrate COVID-19 vaccines. The population is vaccinated by districts considering epidemiological aspects such as the risk of excess mortality, population density, and accessibility for vaccination. However, vaccination for indigenous communities is delivered considering only the territorial scope and regardless of age (MinSa Peru, 2021[80]). COVID-19 vaccination is administered in vaccination centres located in open spaces but are delivered by health teams from PHC centres; assigned by the Health Networks or the local Health authority (MINSA, 2021[81]).
In Costa Rica, PHC carried out COVID-19 vaccination through the Expanded Programmes of Local Immunisations, directed by the Departments of Nursing and Basic Health Care Teams (EBAIS), which oversaw training auxiliary nursing staff and ATAPS to administer the vaccines and subsequently register immunisations in the Integrated Vaccination System SIVA.
Brazil capitalised of its National Immunisation Programme (Programa Nacional de Imunizaçoes) which entails recommended vaccination campaigns offered in communities, including in schools and people’s houses, by the primary health care team. Vaccination is a routine and embedded practice at primary health care level since 1973, making it possible to scale-up COVID-19 vaccination programme quickly. As in many OECD countries, the Brazilian SUS was capable to implement vaccination drives with little vaccine hesitancy (Lotta et al., 2022[82]).
By contrast, PHC did not play a central role in COVID-19 vaccination in Colombia and Mexico. More specifically, in Colombia, responsibility to guarantee access to the vaccine lays to a great extent on health promotion entities (EPS) and Secretariats of Health of National territories. During the rollout of the vaccination plan, these entities allocated a vaccination point in the municipality of residence of affiliates, or the workplace of health workers. Primary health care facilities have not been the central mechanism to approach the population to be vaccinated. Similarly, in Mexico PHC services have not been directly involved in the vaccination strategy (Secretataría de Salud de México, 2020[83]; Secretaría de Salud de México, 2021[84]). Each of the 32 Mexican states has a co-ordinator for the COVID-19 vaccination strategy, and the government installed more than 1 000 vaccination centres in military and civil facilities and deployed vaccination brigades all over the country. Each vaccination brigade comprises thirteen members: public servants working for the Secretary of Wellness; two social programme promoters; four members of the Armed Forces belonging to the Navy, Army, or National Guard; two civil society volunteers; one physician overseeing the technical vaccination components and trained to detect and treat adverse reactions; and two nurses (Secretaría de Salud de México, 2021[84]).
The community-based approach of primary health care gives strong argument to capitalise on primary health care team to facilitate the rapid implementation of vaccine distribution and roll-out in case of future health emergency. The PHC network is also extremely useful to reach population living in deprived, rural, and remote areas. International experiences show that several OECD countries have also deployed mobile primary health care units to increase vaccination coverage. In Australia for example, most vaccines have been provided by primary care providers, including family doctors, primary care nurses, and pharmacists working in local clinics, where these established relationships have been critical in educating members of the local community, allaying concerns, and optimising vaccine uptake. Vaccine initiatives that are taken directly to members of at-risk communities have been effective in reducing barriers to vaccination. A mobile vaccination clinic in Melbourne has been providing COVID-19 information and vaccines to up to 40 homeless people every day visiting a variety of locations, including homelessness services, drop-in centres, crisis accommodation facilities, and rooming houses. The vaccination team includes two nurse immunisers, a peer worker who has a lived experience of homelessness, a social worker, and a clerical support worker (Cohealth Care for All, 2021[85]). Similarly, in the United States, PHC has been a key ally on overcoming vaccination hesitancy, by allowing patients to receive COVID-19 vaccines in familiar settings such as community centres.
Large disruption of health promotion and vaccination during COVID-19 occurred in all LAC-7 countries during the pandemic
The COVID-19 pandemic has not only direct health effects on the population suffering from the disease, but also indirect health effects due to the disruption of preventive services such as ordinary health promotion and immunisation. In a WHO Pulse survey, almost one in every two of the 129 participating countries signalled disruptions to routine facility-based and outreach immunisation services, for example. Disruptions in routine immunisation, even after the increase of COVID-19 vaccination campaigns, were more generally signalled in outreach immunisation services and amongst school-aged children. While a recovery from disruption was observed in Q1 2021, countries signalling disruptions increased by 14% in facility-based immunisation and 7% in outreach immunisation in Q4 2021 when compared to Q1 2021 (WHO, 2022[86]).
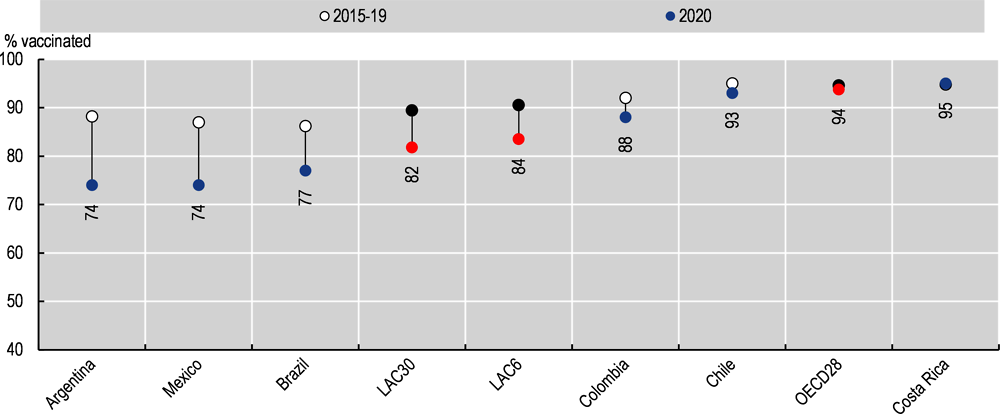
Latin American and Caribbean countries have not equally been exempted from routine immunisation disruptions. Coverage for DTP3 vaccines amongst children aged 1 have fallen in 2020 across the region (82%) when compared to the average between 2015 and 2019 (89%). This has also been the case for OECD member countries – although to a lower extent- moving down from a 95% coverage in 2015-19 to 94% in 2020. Countries like Argentina, Mexico, and Brazil fell below an 80% DTP3 immunisation coverage in 2020, while Costa Rica was the only selected country to exhibit a slight increase in 2020 when compared with the 2015-19 average (see Figure 4.10).
There are also growing available evidence showing disruption in health promotion and immunisation in Brazil, Mexico, Chile, Peru and Colombia.
In Brazil, immunisation coverage fell by 18% during the first year of the COVID-19 crisis according to estimates using databases from the Brazilian unified health system (DATASUS). In addition, PHC and home visits were reduced by 30% across the country when contrasting the period from March to December 2020 with previous years. The COVID-19 crisis has provoked a significant reduction of health promotion and vaccination in Brazil (de Oliveira et al., 2022[87]).
In Mexico, data from the Mexican Institute of Social Security (IMSS), suggests changes in service use and outcomes from April to December 2020 compared to the year before the pandemic. Decreases were observable on contraceptive services (-54%) and child vaccinations (-36%), for example (Doubova et al., 2021[88]).
While the Chilean Ministry of health ordered to maintain health care access for children under the age of five in PHC, the country saw a 66% reduction in children’s consultations. In fact, the number of children aged 24-48 months receiving health care in 2019 was 293 331, while in 2020, this figure decreased by two-thirds down to 97 594. The lack of health workforce, with nurses being included in epidemiological surveillance teams, triage, and later in the vaccination strategy managed by PHC is an important factor explaining disruption in children’s health care.
In Peru, total vaccine coverage for children aged under 12 months decreased from 76.7% in 2019 to 61.1% in 2020, with vaccines such as the pentavalent lowering their coverage in the same age group from 78.5% (2019) to 63.8% (2020). This low routine vaccination coverage during the COVID-19 pandemic has generated an increase in the number of susceptible population under the age of five, both for diseases in eradication and elimination -polio, measles, rubella, and neonatal tetanus-, as well as for diseases under control -diphtheria, whooping cough, chickenpox, and hepatitis B (MinSa Peru CDC, 2021[89]).
Colombia has also experienced a disruption of child and adult immunisation during the COVID-19 pandemic. While vaccination services did not close during the pandemic, vaccination coverage rates for 26 vaccine-preventable diseases included in Colombia’s Amplified Immunisation Programme fell behind the 95% expected target for 2020 (Gestarsalud, 2020[90]). A modelling study carried out by the Institute of Health Metrics and Evaluation (IHME) estimates a 5% and 3% disruption in 2020 for DTP3 and measles vaccination coverage, respectively. Reasons for vaccine disruptions include lockdowns that created barriers for children and parents to reach immunisation sessions, fear of contracting COVID-19, the reconversion of health workers to pandemic response duties, as well as lack of personal protective equipment (PPE) and disruptions in the vaccine supply chain (IHME, 2021[91]).
Consequences from the routine immunisation disruption are already visible. Measles cases reported around the world have increased by 79% in the first two months of 2022 when compared to the same period in 2021 (UNICEF/WHO, 2022[92]). Significant numbers of children are being left without protection against vaccine-preventable diseases due to vaccine-access inequalities, disruptions, and resource diversion that have been caused by the COVID-19 pandemic. This will likely result in alarming outbreaks of vaccine-preventable diseases in the years to come.
To overcome the disruption of routine immunisation and recover services over the long term, some other OECD countries have implemented policies to reach pre-pandemic coverage levels (see Box 4.5). These include focusing on catch-up immunisation strategies, strengthening health information systems, increasing resource mobilisation, and fostering resilience in health systems. However, in order for these to be more effective, it is crucial to identify vulnerable children who have been missed from immunisation campaigns during the pandemic, and provide targeted catch-up immunisation services to low coverage areas (Shet et al., 2022[93]). PHC could play a determinant role in this targeted approach.
In Canada, due to the missed routine vaccination linked to the COVID-19 pandemic, three components have been defined for catching-up with pre-pandemic vaccination coverage levels:
1. Identification of non-vaccinated people across the life course.
2. Detection of vaccine delivery gaps, adaptation and adjustment of immunisation campaigns, and development of appropriate and tailored strategies for catching up.
3. Communication, documentation, evaluation, and readjustment of the immunisation programmes.
Ensuring that routine immunisation and catch-up programmes are properly undertaken during the pandemic is key to strengthen the immunisation coverage in Canada.
Source: MacDonald et al. (2020[94]), “COVID-19 and missed routine immunizations: designing for effective catch-up in Canada”, https://doi.org/10.17269/s41997-020-00385-4.
The role and reach of PHC could be expanded across the LAC-7 countries to increase preparedness and resilience for future outbreaks. For a start, strong PHC which focuses on health promotion and vaccination improves the overall health of the population prior to health emergency, which enhances preparedness to deal with emerging pathogens or health shocks such as the COVID-19 pandemic. This was evident during the COVID-19 pandemic, as obesity and more generally chronic diseases were shown to be risk factors for serious cases and death from the disease (OECD, forthcoming[95]). Yet, given the increasing risk factors to health and rising burden conditions in all LAC-7 countries, there is scope to strengthen health promotion and vaccination into primary health care. In fact, significant variation in performance remains (for example on unsatisfied demand for family planning, counselling for risk factors to health, and vaccination programmes), with marked socio-economic inequality (for example in Peru and Brazil).
In many aspects, PHC has contributed to the COVID-19 emergency response in LAC-7 countries by carrying out some public health activities. Some LAC-7 countries have used primary health care to create awareness on COVID-19 risks and tailor messages on non-pharmaceutical intervention. This was the case in Costa Rica, Peru and Argentina, where CHWs provided information to patients and communities on COVID-19 diseases and prevention of infection. Some developments and innovations were also introduced to proactively identify and engage with high-risk individuals (in Argentina, Costa Rica and Mexico) and to trace contact patients (such as Argentina and Colombia). However, in other LAC-7 countries (including Peru, Chile, Brazil and Mexico) the surveillance system was not appropriate to effectively identify and monitor high-risk populations and aggregate data at community level to make decision about public health. Improving the collection of real-time data on infection and clusters, collected by PHC teams, and integrated at a national and regional level, will help to respond proactively to future shocks. Strong PHC teams can also facilitate the uptake and delivery of outbreak disease vaccination, such as the COVID-19 vaccination campaign. While most of LAC-7 countries faced procurement issues to access COVID-19 vaccine (except Chile), they have capitalised on well-established vaccination campaigns, embedded into the community and primary care settings, health workers’ daily activity, and people lives. Chile, Argentina, Peru, Costa Rica and Brazil are good examples of COVID-19 vaccination programmes implemented at primary health care level.
As in many OECD countries, most LAC-7 countries faced indirect health effects including for example the disruption of routine health promotion and immunisation. Coverage for DTP3 vaccines amongst children aged one have for example fallen in 2020 across the region (82%) when compared to the average between 2015 and 2019 (89%). Largest reductions are found in Argentina, Mexico and Brazil. These alarming trends put children at risk of preventable diseases, and urgently call for strengthening routine immunisation programmes and implementing plans to reach out those who have missed routine vaccination, being often the most disadvantaged who do not have access to health services.
Critically, LAC-7 countries should develop national and regional epidemic preparedness plans -building on influenza-specific plans, which give a central and well-defined role to PHC teams and CHWs. Programmes for epidemiological surveillance, pre-tested risk communication strategies, and vaccine distribution networks are some of the key aspects that would allow these epidemic preparedness plans to work efficiently and make the most of PHC during future outbreaks. Other episodes such as the 2015-16 Zika virus epidemic, and recurring outbreaks of Dengue, Chikungunya, Yellow Fever and Cholera in the region are also worth analysing to improve the effectiveness of the response through a wider use of PHC (Di Paolantonio, 2020[66]). A greater level of professionalisation for CHWs is also extremely relevant both to improve population health in LAC-7 countries and to carry out several public health functions during a health emergency.
References
[77] Aguilera, X. et al. (2021), “The story behind Chile’s rapid rollout of COVID-19 vaccination”, Travel Medicine and Infectious Disease, Vol. 42, p. 102092, https://doi.org/10.1016/j.tmaid.2021.102092.
[40] Aliabadi, A., A. Sheikhtaheri and H. Ansari (2020), “Electronic health record–based disease surveillance systems: A systematic literature review on challenges and solutions”, Journal of the American Medical Informatics Association, Vol. 27/12, https://doi.org/10.1093/jamia/ocaa186.
[3] Boudreau, A. et al. (2022), “Pediatric Primary Health Care: The Central Role of Pediatricians in Maintaining Children’s Health in Evolving Health Care Models”, Pediatrics, Vol. 149/2, https://doi.org/10.1542/peds.2021-055553.
[78] Castillo, C., P. Villalobos Dintrans and M. Maddaleno (2021), “The successful COVID-19 vaccine rollout in Chile: Factors and challenges”, Vaccine: X, Vol. 9, p. 100114, https://doi.org/10.1016/j.jvacx.2021.100114.
[42] CGI.br (2020), ICT in Health 2019.
[20] Chan, M. et al. (2017), “Reaching everyone, everywhere with life-saving vaccines”, The Lancet, Vol. 389/10071, pp. 777-779, https://doi.org/10.1016/s0140-6736(17)30554-8.
[76] Chiolero, A. (2021), “Primary healthcare for a long term and sustainable vaccination strategy”, BMJ, Vol. 372, https://doi.org/10.1136/bmj.n650.
[85] Cohealth Care for All (2021), Taking vaccine to people experiencing homelessness, https://www.cohealth.org.au/media-release/taking-vaccine-to-people-experiencing-homelessness/.
[14] Consejo Nacional de Población (2019), Estrategia Nacional para la Prevención del Embarazo en Adolescentes (ENAPEA), Informe 2019 [National Strategy for the Prevention of Pregnancy in Adolescents (ENAPEA), Report 2019], https://www.gob.mx/cms/uploads/attachment/file/559766/informe2019-enapea.pdf.
[67] Córdova-Villalobos, J. (2017), The 2009 pandemic in Mexico: Experience and lessons regarding national preparedness policies for seasonal and epidemic influenza, Gaceta Médica de México 2017;153:102-10, Mexico, http://www.anmm.org.mx/GMM/2017/n1/GMM_153_2017_1_102-110.pdf.
[87] de Oliveira, M. et al. (2022), “Repercussions of the COVID-19 pandemic on preventive health services in Brazil”, Preventive Medicine, Vol. 155, p. 106914, https://doi.org/10.1016/j.ypmed.2021.106914.
[7] DHS Program (2022), The Demographic and Health Surveys (DHS) Program, https://dhsprogram.com/.
[66] Di Paolantonio, G. (2020), Fostering resilience in the post-COVID-19 health systems of Latin America and the Caribbean, OECD, Paris, https://www.oecd.org/about/civil-society/youth/Shaping-the-Covid-19-Recovery-Ideas-from-OECD-s-Generation-Y-and-Z.pdf.
[88] Doubova, S. et al. (2021), “Disruption in essential health services in Mexico during COVID-19: an interrupted time series analysis of health information system data”, BMJ Global Health, Vol. 6/9, p. e006204, https://doi.org/10.1136/bmjgh-2021-006204.
[72] EU-LAC-Foundation (2021), COVID-19 Vaccines: The Global Challenge of Equitable Distribution and Access, https://eulacfoundation.org/sites/default/files/attachments/I%20EU-LAC%20Policy%20Brief_EN_0.pdf.
[69] Faria, N. et al. (2017), “Establishment and cryptic transmission of Zika virus in Brazil and the Americas”, Nature, Vol. 546/7658, pp. 406-410, https://doi.org/10.1038/nature22401.
[53] FILAC (2020), Second Report: Regional Indigenous Platform against COVID-19. Communities at Risk and Good Practices, https://indigenasCOVID-19.red/wp-content/uploads/2020/06/FILAC_FIAY_segundo-informe-PI_COVID-19.pdf.
[90] Gestarsalud (2020), Caída en cobertura de vacunación amenaza con resurgimiento de enfermedades prevenibles en medio de la pandemia, https://gestarsalud.com/2020/10/08/caida-en-cobertura-de-vacunacion-amenaza-con-resurgimiento-de-enfermedades-prevenibles-en-medio-de-la-pandemia/.
[70] Giovanetti, M. et al. (2020), “Genomic and Epidemiological Surveillance of Zika Virus in the Amazon Region”, Cell Reports, Vol. 30/7, pp. 2275-2283.e7, https://doi.org/10.1016/j.celrep.2020.01.085.
[44] Global Health Intelligence (2017), Electronic Medical Records Growing in Latin America, https://globalhealthintelligence.com/ghi-analysis/electronic-medical-records-growing-in-latin-america/.
[17] Guanais, F. and et al. (2018), From the Patient’s Perspective: Experiences with Primary Health Care in Latin America and the Caribbean, Inter-American Development Bank, https://doi.org/10.18235/0001255.
[24] Guzman-Holst, A. et al. (2020), “Barriers to vaccination in Latin America: A systematic literature review”, Vaccine, Vol. 38/3, pp. 470-481, https://doi.org/10.1016/j.vaccine.2019.10.088.
[68] Hernández-Ávila, M. (2020), Mexico: Lessons learned from the 2009 pandemic that help us fight COVID-19, Canadian College of Health Leaders, Volume: 33 issue: 4, page(s): 158-163, https://doi.org/10.1177/0840470420921542.
[91] IHME (2021), Global COVID-19 Routine Childhood Vaccination Disruption 2020, https://doi.org/10.6069/5AT6-9874.
[12] IMSS (2020), Durante 2019, el programa IMSS-Bienestar redujo 37,000 embarazos no deseados en adolescentes a través de los CARA [Press Release No. 120/2020, During 2019, the IMSS-Bienestar program reduced 37,000 unwanted pregnancies in adolescents through CARA], http://www.imss.gob.mx/prensa/archivo/202003/120.
[28] IMSS (2000), Norma que establece las disposiciones para la aplicación de la Vigilancia epidemiológica en el Instituto Mexicano del Seguro social, 2000-001-020, Actualización 2017 [Norm that establishes the rules for Epidemiological Surveillance in the Mexican Institut, IMSS, Mexico, http://www.imss.gob.mx/sites/all/statics/pdf/manualesynormas/2000-001-020.pdf.
[15] Jané-Llopis, E. et al. (2020), “Implementing primary healthcare-based measurement, advice and treatment for heavy drinking and comorbid depression at the municipal level in three Latin American countries: final protocol for a quasiexperimental study”, BMJ Open, Vol. 10/e038226, https://doi.org/10.1136/bmjopen-2020-038226.
[51] Katz, M. (2021), “Regardless of Age, Obesity and Hypertension Increase Risks With COVID-19”, JAMA Internal Medicine, Vol. 181/3, p. 381, https://doi.org/10.1001/jamainternmed.2020.5415.
[41] Kruse, C. et al. (2018), “The use of Electronic Health Records to Support Population Health: A Systematic Review of the Literature”, Journal of Medical Systems, Vol. 42/214, https://doi.org/10.1007/s10916-018-1075-6.
[57] Kumpunen, S. et al. (2021), “Transformations in the landscape of primary health care during COVID-19: Themes from the European region”, Health Policy, https://doi.org/10.1016/j.healthpol.2021.08.002.
[75] Lewis, C., R. Nuzum and E. Schneider (2021), Engaging and Supporting Primary Care Providers in the Fight Against COVID-19, https://www.commonwealthfund.org/blog/2021/engaging-and-supporting-primary-care-providers-fight-against-covid-19.
[82] Lotta, G. et al. (2022), “COVID-19 vaccination challenge: what have we learned from the Brazilian process?”, The Lancet Global Health, Vol. 10/5, https://doi.org/10.1016/S2214-109X(22)00049-3.
[94] MacDonald, N. et al. (2020), “COVID-19 and missed routine immunizations: designing for effective catch-up in Canada”, Canadian Journal of Public Health, Vol. 111/4, pp. 469-472, https://doi.org/10.17269/s41997-020-00385-4.
[43] Meza, L., I. Vargas and X. Barros Rubio (2019), “Health demand management : characterisation of primary care centers”, Medwave, Vol. 19, https://doi.org/10.5867/medwave.2019.S1.
[81] MINSA (2021), Vaccinating is Life, MINSA Ministry of Health, Lima, http://bvs.minsa.gob.pe/local/MINSA/5486.pdf.
[61] MINSA (2020), Approve Administrative Directive No. 287-MINSA-2020-DGIESP: Administrative Directive that regulates the processes, records and access to information to guarantee the comprehensive monitoring of suspected and confirmed cases of COVID -19 (Integrated System, MINSA Minsitry of Health, Lima, https://cdn.www.gob.pe/uploads/document/file/581449/RM_183-2020-MINSA_Y_ANEXOS.PDF.
[54] MinSa Costa Rica (2020), Guideline for Medical Assessment of Suspicious Cases due to covid-19 in Indigenous Territories that Require Transfers from Communities with Difficult Geographical and Cultural Access, https://www.ministeriodesalud.go.cr/sobre_ministerio/prensa/docs/ls_pg_015_lineamientos_prevencion_territorios_indigenas_07082020.pdf.
[80] MinSa Peru (2021), Updated National Vaccination Plan against COVID-19, Peru, 2021, https://cdn.www.gob.pe/uploads/document/file/1805113/Plan%20Nacional%20Actualizado%20contra%20la%20COVID-19.pdf.
[48] MinSa Peru (2020), Comités ciudadanos anti COVID-19: el momento de la participación comunitaria, https://www.youtube.com/watch?v=dsLjlB2SC1U.
[89] MinSa Peru CDC (2021), Peru Epidemiological Bulletin SE 43-2021 (from October 24 to 30, 2021), https://www.dge.gob.pe/epipublic/uploads/boletin/boletin_202143_02_194945.pdf.
[60] MinSalud Colombia (2020), Pruebas, Rastreo y Aislamiento Selectivo Sostenible - PRASS, https://www.minsalud.gov.co/salud/publica/PET/Paginas/Pruebas-Rastreo-y-Aislamiento-Selectivo-Sostenible.aspx.
[35] Neto, J. et al. (2021), “Building the capacity of community health workers to support health and social care for dependent older people in Latin America: a pilot study in Fortaleza, Brazil”, BMC Geriatr, Vol. 21/526, https://doi.org/10.1186/s12877-021-02477-3.
[36] Nunes, J. (2020), “The everyday political economy of health: community health workers and the response to the 2015 Zika outbreak in Brazil”, Review of International Political Economy, Vol. 27/1, https://doi.org/10.1080/09692290.2019.1625800.
[65] OECD (2022), Evaluation of Luxembourg’s COVID-19 Response: Learning from the Crisis to Increase Resilience, https://doi.org/10.1787/2c78c89f-en.
[18] OECD (2022), Guidebook on Best Practices in Public Health, OECD Publishing, https://doi.org/10.1787/4f4913dd-en.
[16] OECD (2022), Healthy Eating and Active Lifestyles: Best Practices in Public Health, OECD Publishing, Paris, https://doi.org/10.1787/40f65568-en.
[22] OECD (2022), OECD Health Statistics 2022, https://www.oecd.org/health/health-data.htm.
[71] OECD (2021), “Access to COVID-19 vaccines: Global approaches in a global crisis”, OECD Policy Responses to Coronavirus (COVID-19), OECD Publishing, Paris, https://doi.org/10.1787/c6a18370-en.
[52] OECD (2021), Health at a Glance 2021: OECD Indicators, OECD Publishing, Paris, https://doi.org/10.1787/ae3016b9-en.
[47] OECD (2021), Policy survey on the role of primary health care during the COVID-19 pandemic.
[46] OECD (2021), Survey of Electronic Health Record System Development and Use, 2016 and 2021.
[19] OECD (2019), OECD Reviews of Public Health: Chile: A Healthier Tomorrow, OECD Reviews of Public Health, OECD Publishing, Paris, https://doi.org/10.1787/9789264309593-en.
[95] OECD (forthcoming), Ready for the Next Crisis? Investing in Resilient Health Systems, OECD Health Policy Studies, OECD Publishing, Paris.
[30] OECD/European Observatory on Health Systems and Policies (2021), Slovenia: Country Health Profile 2021, State of Health in the EU, OECD Publishing, Paris, https://doi.org/10.1787/1313047c-en.
[21] OECD/The World Bank (2020), Health at a Glance: Latin America and the Caribbean 2020, OECD Publishing, Paris, https://doi.org/10.1787/6089164f-en.
[79] Our World in Data (2022), Coronavirus Pandemic (COVID-19), https://ourworldindata.org/coronavirus.
[59] PAHO (2020), Detecting: Argentina’s testing and contact tracing strategy to break the COVID-19 transmission chain, https://www.paho.org/en/stories/detecting-argentinas-testing-and-contact-tracing-strategy-break-covid-19-transmission-chain.
[1] PAHO (2017), Health in the Americas+, 2017 Edition. Summary: Regional Outlook and Country Profiles, Pan American Health Organization, Washington DC, https://www.paho.org/salud-en-las-americas-2017/wp-content/uploads/2017/09/Print-Version-English.pdf.
[34] Pallas, S. et al. (2013), “Community Health Workers in Low- and Middle-Income Countries: What Do We Know About Scaling Up and Sustainability?”, Am J Public Health, Vol. 103/7, https://doi.org/10.2105/AJPH.2012.301102.
[38] Pesec, M. et al. (2017), “Primary Health Care That Works: The Costa Rican Experience”, Health Affairs, Vol. 36/3, https://doi.org/10.1377/hlthaff.2016.1319.
[74] Pinaka, O. et al. (2021), “The role of local primary healthcare units in increasing immunization uptake among children in vulnerable social groups through vaccination campaigns”, Public Health in Practice, https://doi.org/10.1016/j.puhip.2021.100185.
[64] Prado, N. et al. (2021), “Ações de vigilância à saúde integradas à Atenção Primária à Saúde diante da pandemia da COVID-19: contribuições para o debate”, Ciência & Saúde Coletiva, Vol. 26/7, pp. 2843-2857, https://doi.org/10.1590/1413-81232021267.00582021.
[50] Rahman, R., A. Ross and R. Pinto (2021), “The critical importance of community health workers as first responders to COVID-19 in USA”, Health Promotion International, Vol. 36/5, pp. 1498-1507, https://doi.org/10.1093/heapro/daab008.
[26] Rechel, B. (2020), Integrating Primary Care and Public Health, World Health Organization, Regional Office for Europe, https://apps.who.int/iris/handle/10665/332481.
[49] ReliefWeb/WHO (2020), Colombia responds to COVID-19 with an intercultural health model, https://reliefweb.int/report/colombia/colombia-responds-covid-19-intercultural-health-model.
[39] RHIhub (2020), Community health Worker Curriculums, https://www.ruralhealthinfo.org/toolkits/community-health-workers/4/training/curriculum.
[63] Sánchez-Talanquer, M., E. González-Pier and J. Sepúlveda (2021), Mexico’s Response to Covid-19: A Case Study, UCSF, https://globalhealthsciences.ucsf.edu/sites/globalhealthsciences.ucsf.edu/files/mexico-covid-19-case-study-english.pdf.
[13] Secretaría de Salud (2020), Programa de Acción Específico. Salud Sexual y Reproductiva 2020-2024 [Specific Action Program. Sexual and Reproductive Health 2020-2024].
[29] Secretaría de Salud (2010), Modelos de recursos para la planeación de las unidades médicas de la Secretaria de Salud [Resource models for planning the medical units of the Ministry of Health], Secretaría de Salud, Mexico.
[84] Secretaría de Salud de México (2021), “Operativo Correcaminos”, Estrategia operativa de la Política Nacional de vacunación contra el virus SARS-CoV-2 para la prevención de la COVID-19 en México, http://vacunacovid.gob.mx/wordpress/documentos-de-consulta/.
[56] Secretaría de Salud de México (2021), Comunicado 183, Estrategia basada en atención primaria de la salud, pilar en mitigación de COVID-19 a nivel comunitario, https://www.gob.mx/salud/prensa/183-estrategia-basada-en-atencion-primaria-de-la-salud-pilar-en-mitigacion-de-COVID-19-a-nivel-comunitario.
[62] Secretaría de Salud de México (2021), Lineamiento Estandarizado Para La Vigilancia Epidemiológica Y Por Laboratorio De La Enfermedad Respiratoria Viral, https://coronavirus.gob.mx/wp-content/uploads/2021/02/Lineamiento_VE_y_Lab_Enf_Viral_Ene-2021_290121.pdf.
[55] Secretaría de Salud de México (2020), Estrategia de promoción de la salud, prevención, atención y mitigación de la COVID-19 en el marco de la atención primaria de la salud, https://coronavirus.gob.mx/wp-content/uploads/2020/10/APS_COVID_v17_08_2020.pdf.
[83] Secretataría de Salud de México (2020), Política Nacional Rectora de Vacunación Contra el SARS-CoV-2 para la Prevención de la COVID-19 en México, Documento rector, https://coronavirus.gob.mx/wp-content/uploads/2021/01/PolVx_COVID_-11Ene2021.pdf.
[93] Shet, A. et al. (2022), “Impact of the SARS-CoV-2 pandemic on routine immunisation services: evidence of disruption and recovery from 170 countries and territories”, The Lancet Global Health, Vol. 10/2, pp. e186-e194, https://doi.org/10.1016/s2214-109x(21)00512-x.
[10] Starrs, A. et al. (2018), “Accelerate progress—sexual and reproductive health and rights for all: report of the Guttmacher– Lancet Commission”, The Lancet, Vol. 391/10140, pp. 2642-2692, https://doi.org/10.1016/s0140-6736(18)30293-9.
[58] Tadele Girum, K. (2020), “Global strategies and effectiveness for COVID-19 prevention through contact tracing, screening, quarantine, and isolation: a systemic review”, Tropical Medicine and Health, Vol. 48/91, https://doi.org/10.1186/s41182-020-00285-w.
[45] The Competitive Intelligence Unit (2020), Electronic health recor in Mexico, https://static1.squarespace.com/static/587fdc951b10e30ca5380172/t/618994ae44eb47201b6d7fa0/1636406447871/The+CIU-Working+Paper+Series+2020-III+Electronic+Health+Record_ENG+v24+.pdf.
[2] Tomczyk, S., J. McCracken and C. Contreras (2019), Factors associated with fatal cases of acute respiratory infection (ARI) among hospitalized patients in Guatemala, BMC Public Health.
[11] UNFPA (2018), Strategic plan 2018-2021, United Nations Population Fund, https://www.unfpa.org/resources/strategic-plan-2018-2021.
[5] UNICEF (2021), Fed to Fail? The Crisis of Children’s Diets in Early Life. 2021 Child Nutrition Report, United Nations Children’s Fund, New York, https://data.unicef.org/resources/fed-to-fail-2021-child-nutrition-report/.
[6] UNICEF (2021), Infant and young child feeding, https://data.unicef.org/topic/nutrition/infant-and-young-child-feeding/.
[8] UNICEF MICS Programme (2022), UNICEF Multiple Indicator Cluster Surveys (MICS) Programme, https://mics.unicef.org/surveys.
[92] UNICEF/WHO (2022), UNICEF and WHO warn of perfect storm of conditions for measles outbreaks, affecting children, https://www.who.int/news/item/27-04-2022-unicef-and-who-warn-of--perfect-storm--of-conditions-for-measles-outbreaks--affecting-children.
[27] VanderZanden, A. et al. (2021), What Does Community-Oriented Primary Health Care Look Like? Lessons from Costa Rica, https://www.commonwealthfund.org/publications/case-study/2021/mar/community-oriented-primary-care-lessons-costa-rica.
[4] Victora, C. et al. (2016), “Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect”, The Lancet, Vol. 387/10017, pp. 475-490, https://doi.org/10.1016/s0140-6736(15)01024-7.
[37] Wadge, H. et al. (2016), “Brazil’s Family Health Strategy: Using Community Health Workers to Provide Primary Primary Care”, The Commonweath Fund Publication, Vol. Case study 13.
[23] WHO (2022), Global Health Observatory, https://www.who.int/data/gho.
[32] WHO (2022), Global Strategy on Human Resources for Health: Workforce 2030: Reporting at Seventy-fifth World Health Assembly, https://www.who.int/news/item/02-06-2022-global-strategy-on-human-resources-for-health--workforce-2030.
[86] WHO (2022), Third round of the global pulse survey on continuity of essential health services during the COVID-19 pandemic: November–December 2021: interim report, 7 February 2022, https://apps.who.int/iris/handle/10665/351527.
[33] WHO (2020), What do we know about community health worker? A systematic review of existing reviews, https://www.who.int/publications/i/item/what-do-we-know-about-community-health-workers-a-systematic-review-of-existing-reviews.
[25] WHO (2019), Global Influenza Strategy 2019-2030, World Health Organization, https://apps.who.int/iris/handle/10665/311184.
[9] WHO (2018), Family planning / Contraception, World Health Organization, https://www.who.int/news-room/fact-sheets/detail/family-planning-contraception.
[31] WHO (2018), Health promotion centres in Slovenia: Integrating population and individual services to reduce health inequalities at community level, https://www.euro.who.int/en/countries/slovenia/publications/health-promotion-centres-in-slovenia-integrating-population-and-individual-services-to-reduce-health-inequalities-at-community-level-2018.
[73] Wilkinson, E. et al. (2021), “Primary Care’s Historic Role in Vaccination and Potential Role in COVID-19 Immunization Programs”, The Annals of Family Medicine, Vol. 19/4, pp. 351-355, https://doi.org/10.1370/afm.2679.